3 Clinically Relevant Anatomy of the Head and Neck Structures Involved in Whiplash
3.1 The Neck: A Broader Perspective
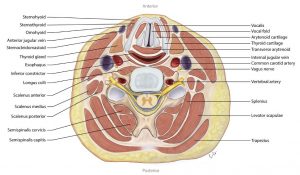
The human neck supports the relatively heavy skull and face. It contains several important neurovascular structures amidst a tight arrangement of musculoskeletal structures (Figure 3-1). The cervical spine forms the core of the neck around which other structures are laid out. The cervical spine normally has a convex curve facing forwards, called cervical lordosis.
3.2 The Support Structure: The Skeleton
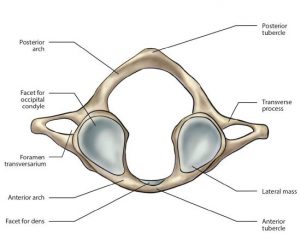
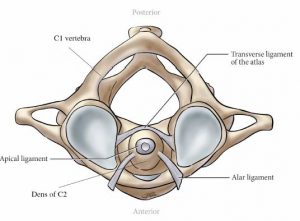
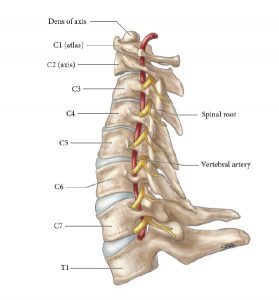
The cervical spine consists of seven vertebral levels: C1 to C7 (Figure 3-2). At the top, the occiput (C0), which is the lower part of the skull, is attached to atlas (C1 vertebra) by a pair of synovial joints. The axis (C2 vertebra) is attached to the atlas by another pair of synovial joints. The atlas and axis differ considerably from the other cervical spine vertebrae in their shape and function (Figure 3-3 and Figure 3-4). The occipitoatlanto-axial joints form the cranio-vertebral junction. There are no intervertebral discs between the occiput and the atlas, or between the atlas and the axis. These two uppermost cervical joints are supplied by the ventral rami of the first and second cervical spinal nerves.1 The inferior articular facet joint surface of C0 is convex and couples with the concave superior articular facet of C1 (Figure 3-3 and Figure 3-4). Motion at the C0-C1 level primarily includes flexion and extension. At the C1-C2 level, the articular surface is convex at the C1 inferior articular facet and is coupled with a convex superior facet of C2, thus allowing the 45 degrees of rotation at this level. Injury to C0-C1 and C1-C2 joints can occur with whiplash injury and can cause cervicogenic headache.
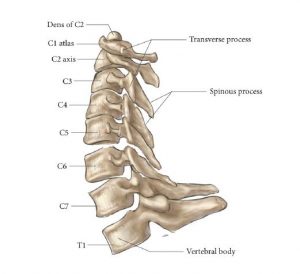
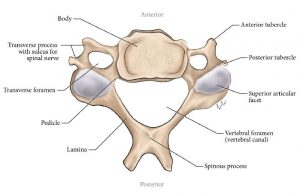
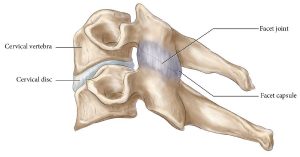
The C3 to C7 vertebrae typically have a body, which is absent in C1 and C2. Cervical vertebrae, from C2 to C7, are joined to each other by a pair of facet joints, present on either side (Figure 3-5).2 The facet joints, also called zygapophyseal joints, are commonly involved in the injury sustained by whiplash patients (see Chapter 4 – Mechanisms of Injury). These are synovial joints with a joint capsule and synovial fold (Figure 3-6). The oblique angle of orientation of the facet joint in relation to the cervical spine influences the plane of movement, thus allowing for varied degrees of flexion, extension, rotation, and sideways movement. These joints are rich in mechanoreceptors and unmyelinated nociceptors. They are richly innervated by A-delta and C fibers along the joint capsule.3 The facet joints are supplied by medial branches of the primary dorsal rami from the two levels adjoining each joint (above and below).
REVIEW 3.1
Which of the following regarding the atlanto-occipital joint is true?
- It forms the cranio-cervical junction and is a synovial joint without an intervertebral disc
- It is the joint between C1 and C2 levels, and allows for flexion-extension movements
- It is the junction between the skull and the cervical spine, and allows for rotational Movements
- It is the junction between the skull and the cervical spine, and allows for flexion-extension movements
Correct answer: 1
3.3 The Neural Structures: Spinal Cord, Cervical Nerves & Root Ganglion
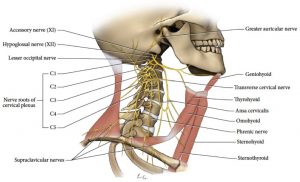
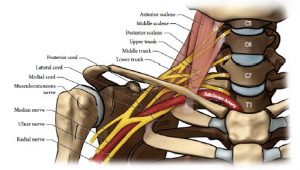
The spinal cord runs within the spinal canal and gives rise to eight pairs of cervical spinal nerves. These spinal nerves exit in an anterolateral direction, superior to their respective vertebral level (Figure 3-7). The C8 nerve exits below the C7 level, superior to the first thoracic vertebra. The anterior rami (divisions) of the upper cervical nerves form the cervical plexus (Figure 3-8); the lower cervical anterior rami, from C5 and below, form the major part of the brachial plexus (Figure 3-9). The brachial plexus, formed by C5-T1 anterior rami, is responsible for the innervation of the upper limb structures. Any injury to the nerve roots at this level can cause pain radiating to the upper limb. The medial branch of the dorsal ramus of C2 forms greater occipital nerve (GON), whereas the lesser occipital nerve originates as part of sensory branches from the cervical plexus from either the C2 or C3 ventral ramus.4 The dorsal ramus of C1 beyond the posterior arch of the atlas and the vertebral artery is known as the suboccipital nerve.4
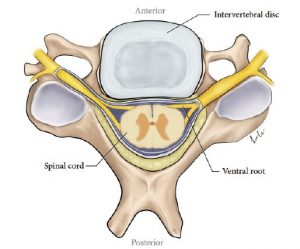
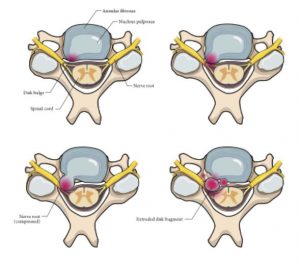
The intervertebral disc, which acts as a cushion between the two vertebral bodies, can be injured during trauma. Figure 3-10 and Figure 3-11 show discs with and without herniation.
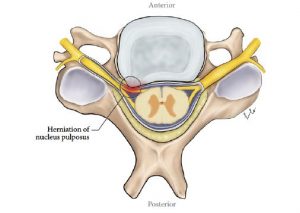
In Amanda’s case, the disc in between C5 and C6 had protruded without disc herniation. The outer layer of the disc remained intact containing the nucleus pulposus that forms the inner core of the disk. Due to this the left C6 nerve root had been involved causing radicular symptoms without obvious signs of radiculopathy.5 Involvement of a nerve root can cause radicular pain due to irritation and presence of inflammatory mediators. Significant involvement, including of motor and sensory fibers can cause radiculopathy (Table 3-1). The symptoms of radicular pain and radiculopathy can overlap, but are different and distinguishable as dermatomal and myotomal nerve supply is different.6 Characteristic features of cervical root involvement are shown in Table 3-1. The anterior and posterior nerve rootlets correspondingly form anterior and posterior nerve roots at each level. The entire nerve root continues as a peripheral spinal nerve from the spinal foramina. The posterior root is formed by afferent (sensory) fibers. The cell bodies of these peripheral axons are contained in the dorsal root ganglia (DRG). The DRG and the nerve roots are susceptible to injury – both directly and indirectly. Unlike a peripheral nerve, they are unprotected by a thick epineurium, and they can be injured due to the sudden movements associated with significant reductions to the intervertebral foramen.7 Indirectly, they can be injured due to the sudden volume and pressure changes within the vascular system. Internal and external venous plexuses normally accommodate large changes in volume; however, rapid motions associated with whiplash and the actual resistance and inertia of the fluid column itself can lead to significant pressure gradients causing stress and injury to nerve roots and the DRG.8 The dorsal rami of cervical nerves innervate the musculoskeletal structures in the dorsal part of the body. They all give rise to medial and lateral branches (Figure 3-12). The medial branches innervate the facet joints and other posterior paraxial muscles (the applied anatomy of medial branches is useful to understand the interventional treatment of facet joint pain).9 The lateral branches innervate the paravertebral muscles and soft tissue. The medial branch of C2 dorsal ramus is known as the GON (Table 3-2). It receives communicating branches from the third occipital nerve. The GON is well recognized as a cause for cervicogenic headache and could be a source of pain due to whiplash injury. Its nerve supply extends posteriorly from the occipital region to as far as the coronal suture on the top of the skull. It also supplies the area around the mastoid process and behind the pinna. The C3 dorsal ramus gives rise to two medial branches of which the bigger, constant branch is called the third occipital nerve. This overlies the C2-C3 joint and supplies the occipital area. It also communicates with the GON. The anatomy of the medial branches is important in the context of interventional treatment for facet joint pain.9
TABLE 3.1 Physical findings associated with cervical radiculopathy
| Disk Level | Root | Pain Distribution | Weakness | Sensory Loss | Reflex Loss |
| C4 – C5 | C5 | Medial scapular border, lateral upper arm to elbow | Deltoid, supraspinatus, infraspinatus muscles | Lateral upper arm | Supinator reflex |
| C5 – C6 | C6 | Lateral forearm, thumb and index finger | Biceps, brachioradialis, wrist extensor muscles | Thumb and index finger | Biceps reflex |
| C6 – C7 | C7 | Medial scapula, posterior arm, dorsum of forearm, third finger | Triceps, wrist flexors, finger extensor muscles | Posterior forearm, third finger | Triceps reflex |
| C7 – C8 | C8 | Shoulder, ulnar side of forearm, fifth finger | Thumb flexors, abductors, intrinsic hand muscles | Fifth finger | _____ |
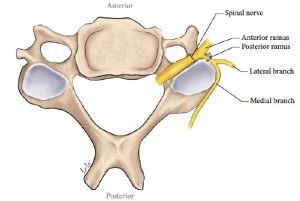
TABLE 3-2 Nerves commonly associated with a whiplash injury and their origin
| Greater occipital nerve | Medial branch of C2 dorsal ramus |
| Lesser occipital nerve | Sensory branch of cervical plexus (ventral rami) |
| Suboccipital nerve | Branch of C1 dorsal ramus |
| 3rd occipital nerve | Important branch of medial branch of C3 dorsal ramus |
| Cervical plexus | Ventral rami of C1–C4 |
| Brachial plexus | Ventral rami of C5–T1 |
REVIEW 3.2 What is the most likely clinical diagnosis in the following patient?
A patient from a vehicular accident presents with a one-month history of pain shooting down into his right upper limb. He has pain radiating to the shoulder and lateral aspect of the upper arm. Examination showed no sensory or motor signs, and reflexes are normal.
- Right C7 radiculopathy
- Right C8 radicular pain
- Right cervical discogenic pain
- Right C5 radicular pain
Correct answer: 4
3.4 Intervertebral Discs
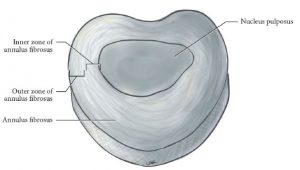
The intervertebral discs are present between two vertebral bodies throughout the cervical spine, except between C1 and C2. Primarily, they are fibrocartilaginous structures with their outer part being formed by the annulus fibrosus and the inner part formed by the nucleus pulposus (Figure 3-13). The outer part of the disc is richly innervated. The inner part is tightly contained within the annulus. When there is an injury causing rupture or tear of the annulus, the inner material can leak out to cause inflammation, thereby causing pain and stiffness10 (Figure 3-14). Discogenic pain is usually limited to the midline structures, around the injured disc. The criteria for such a diagnosis are still not clear, but involve both clinical and imaging findings.11 Injury to the disc can also lead to herniation or extrusion of the disc material. This displacement can involve the accompanying nerve root exiting at that level or traversing the spinal canal at that level. This gives rise to radicular pain, as in the case of Amanda. Involvement of motor and sensory fibers can lead to radiculopathy. The symptoms and signs of cervical radicular disease have been discussed earlier
(Table 3-1).
REVIEW 3.3
Which of the following is true?
- Intervertebral discs are not well innervated
- With a disc bulge, inflammatory mediators are released
- Discogenic pain is referred to the nerve root involved
- Intervertebral discs are fibrocartilaginous structures
Correct answer: 4
3.5 The Binding Structures: Cervical Ligaments of Importance
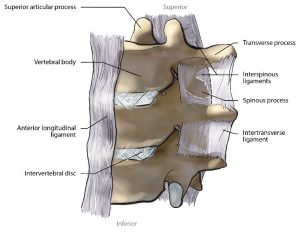
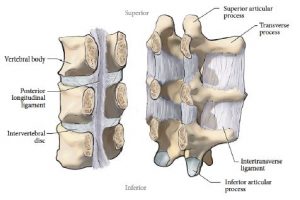
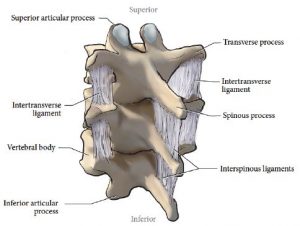
The ligaments are structures responsible for holding the cervical vertebral elements together (Figure 3-15, Figure 3-16, Figure 3-17). Among them, there are six important ligaments. The anterior and posterior longitudinal ligaments span the anterior and posterior part of the vertebral bodies and merge with underlying annular fibers from the disc. The interspinous ligaments are posteriorly situated ligaments, and join together the adjacent spinous processes. These merge with the supraspinous ligaments, which may not be present in all adults. Ligamentum flavum is the thickest and the most elastic ligament in the body. It is present between two laminae. The capsular ligaments encase the facet joints in each side and may be deficient, especially in the medial aspect. There are other ligaments in the upper cervical spine such as the alar and transverse ligaments.4 Minor to major injury to these ligaments is possible with a whiplash injury and not all can be observed with imaging studies. In fact, recent studies have highlighted that capsular strain and injury to the capsular ligament are common, especially if the head is rotated.12,13 Clinically it is also correlated that as many as 57% of whiplash victims with chronic symptoms for more than two years reported having their head turned at the time of impact. Others have also noted serious injuries to alar and transverse ligaments associated with the upper spine, with victims having their head turned.14
3.6 The Vascular Structures
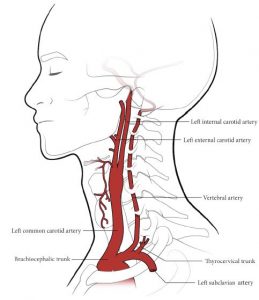
Carotid arteries, the vertebral artery and the thyrocervical trunk supply the structures of the head and neck (Figure 3-18). The common carotid artery bifurcates at the level of C4 (thyroid cartilage) into external and internal carotid arteries. The external carotid artery supplies structures outside the cranial cavity by dividing into multiple branches within the parotid gland.15 The vertebral artery is a branch of the subclavian artery. It is composed of viscous and elastic elements. Underneath the outer collagen fibers, its media consists of both elastic and smooth muscle fibers. After its origin, it enters the foramen tranversarium at the C6 level and passes upwards within the respective transverse foramen. At C1, it passes along the posterior arch and then medially, entering the cranial cavity through the foramen magnum. The vertebral arteries then converge to form the basilar artery. The vertebral artery is proposed to be involved during whiplash injury.16 During a whiplash injury, vertebral artery injury is known to occur due to coupled extension and rotational components. It has been observed that the vertebral artery goes through elongation causing transient vascular compromise and its injury may also involve intimal tears. Neither the internal carotid artery nor the vertebral artery supply any structure of the neck and entirely supply the brain and the spinal cord. Branches of the thyrocervical trunk supply the myofascial structures.
3.7 The Myofascial Structures
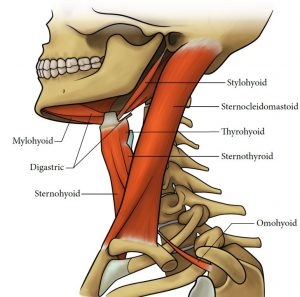
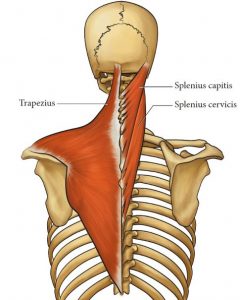
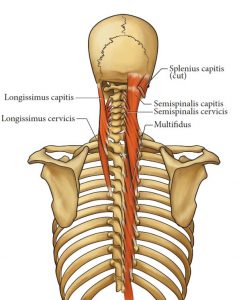
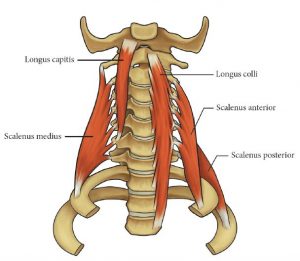
The neck has various layers of myofascial tissues. The superficial fascia includes the superficial dermis, fat and the platysma, which is a thin muscle present anteriorly. The deep cervical fascia effectively divides the neck into three parts. The investing layer encloses the sternocleidomastoid and trapezius muscles, both anterolaterally and posterolaterally. The pretracheal layer surrounds the muscles present anterior to the vertebral bodies, including the infrahyoid muscles. Muscles posterior to the transverse processes are enclosed within the prevertebral layer. In the front, they cover the scalene muscles. The posterior paravertebral muscles are arranged in superficial and deep muscle layers.17 The superficial muscles such as trapezius and sternocleidomastoid do not attach to any vertebral elements (Figure 3-19) (Figure 3-20). The deeper muscles including splenius capitis and cervicis, semispinalis capitis and cervicis, longissimus capitis and cervicis, scalenes, and longus capitis and colli, attach on multiple cervical vertebrae (Figure 3-20) (Figure 3-21) (Figure 3-22). The deepest layer is the multifidus, which is present at several levels (Figure 3-16). Multifidus attaches directly to the facet capsule. There is indirect evidence linking muscle injury occurring during the accident to chronic pain associated with the whiplash.18 Muscles are an integral part of neuromuscular control and are considered to be involved in the pathogenesis of chronic pain. During the actual injury, the rapid neck muscle activation may alter the load and stress experienced by other deeply situated vital structures. Those patients with chronic pain associated with whiplash injury demonstrate abnormal neuromuscular patterns, and may develop secondary functional alterations due to chronic sensitization. Further details about cervical musculature and their importance in whiplash injury are discussed in Chapter 7.
3.8 References
- Hoppenfeld JD. Cervical facet arthropathy and occipital neuralgia: headache culprits. Curr Pain Headache Rep 2010;14:418-23.
- Swartz EE, Floyd RT, Cendoma M. Cervical spine functional anatomy and the biomechanics of injury due to compressive loading. J Athl Train 2005;40:155-61.
- Yoganandan N, Pintar FA, eds. Frontiers in Whiplash Trauma: Clinical and Biomechanical. Amsterdam: IOS Press; 2000. 17 p.
- Interventional spine: An algorithmic approach. Slipman CW, ed. Philadelphia, PA: Saunders Elsevier; 2008.
- Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. Am Fam Physician 2010;81:33-40.
- Corey DL, Comeau D. Cervical radiculopathy. Med Clin North Am 2014;98:791-9, xii.
- Tominaga Y, Maak TG, Ivancic PC, Panjabi MM, Cunningham BW. Headturned rear impact causing dynamic cervical intervertebral foramen narrowing: implications for ganglion and nerve root injury. J Neurosurg Spine 2006;4:380-7.
- Svensson MY, Bostrom O, Davidsson J, et al. Neck injuries in car collisions–a review covering a possible injury mechanism and the development of a new rear-impact dummy. Accid Anal Prev 2000;32:167-75.
- Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine 1982;7:319-30.
- Raj PP. Intervertebral disc: anatomy-physiology-pathophysiologytreatment. Pain Pract 2008;8:18-44.
- Malik KM, Cohen SP, Walega DR, Benzon HT. Diagnostic criteria and treatment of discogenic pain: a systematic review of recent clinical literature. Spine J 2013;13:1675-89.
- Yoganandan N, Pintar FA, Klienberger M. Cervical spine vertebral and facet joint kinematics under whiplash. J Biomech Eng 1998;120:305-7.
- Winkelstein BA, Nightingale RW, Richardson WJ, Myers BS. The cervical facet capsule and its role in whiplash injury: a biomechanical investigation. Spine 2000;25:1238-46.
- Kaale BR, Krakenes J, Albrektsen G, Wester K. Head position and impact direction in whiplash injuries: associations with MRI-verified lesions of ligaments and membranes in the upper cervical spine. J Neurotrauma 2005;22:1294-302.
- Johnson MH, Thorisson HM, Diluna ML. Vascular anatomy: the head, neck, and skull base. Neurosurg Clin North Am 2009;20:239-58.
- Taneichi H, Suda K, Kajino T, Kaneda K. Traumatically induced vertebral artery occlusion associated with cervical spine injuries: prospective study using magnetic resonance angiography. Spine 2005;30:1955-62.
- Blouin JS, Siegmund GP, Carpenter MG, Inglis JT. Neural control of superficial and deep neck muscles in humans. J Neurophysiol 2007;98:920-8.
- Elliott JM. Are there implications for morphological changes in neck muscles after whiplash injury? Spine 2011;36(25 Suppl):S205-10.
