Perspective: Breast Milk
Janet Colson
Learning Outcomes
After reading and discussing this text, students should be able to:
- Trace the history of infant feeding practices over the last three centuries.
- Explain the importance of human milk for infant survival.
- Differentiate between cross-nursing, wet-nursing, and milk-sharing.
- Identify the pros and cons of pasteurizing human milk.
Introduction
Shortly after my father’s birth in 1918, his mother developed the Spanish flu, requiring her to be hospitalized for several weeks. During my grandmother’s absence, a neighbor cared for my father, who was less than a month old at the time. The neighbor fed him from her own breasts, a practice known as wet-nursing.
A century later, the global COVID pandemic had a similar effect on newborns. Today, because wet-nursing is taboo in most countries, mothers too ill to nurse have the option to purchase another woman’s breast milk. Human milk is available to buy from accredited milk banks or from enterprising women selling their milk for extra income. Some lucky parents may have a friend or relative willing to supply breast milk free of charge, a practice known as milk sharing. According to public health officials, mothers unable to nurse should only use another woman’s milk that has been pasteurized, similar to the milk sold in grocery stores.[1] This type milk is known as pasteurized human donor milk.
How did we, as a global community, transition from a birth mother nursing from her own breasts, to outsourcing infant feeding to paid wet nurses, to having a market for pasteurized human milk? We can trace the history to at least 1000 BC.
Milk for Human Infants
Human breast milk has always been the gold standard for feeding infants. Humanity would not exist today had our ancestral mothers refused to nurse. Perhaps one of the earliest written records of nursing is found in Exodus from the Old Testament bible. The author describes how Moses’ mother hides him in a basket to prevent his execution and a princess finds the young infant and decides to adopt him. Realizing that he will need a wet nurse, Moses’ big sister tells the princess that her mother is willing to nurse the babe.[2] Not knowing that the woman is Moses’ actual birth mother, the princess pays her to serve as his wet nurse.
Although not common, hiring a wet nurse is still an option for today’s parents, but there are several other methods. As shown in Table I, the World Health Organization (WHO) recommends human milk, fed directly from the natural mother’s breasts, as the best method.[3] If an infant is too weak to nurse from the birth mother’s breasts, the woman should pump and feed her milk through a bottle or other feeding device. If the birth mother cannot produce enough milk to meet the needs of her infant, use of pasteurized human milk from an accredited donor milk bank ranks third. Fourth in this ranking is the use of a wet-nurse. Because it is not socially accepted in all cultures, WHO clarifies their stance: “Wet-nursing may be an option depending on acceptability to mothers and families, availability of wet nurses, and services to support mothers and wet nurses.”[4] Commercial infant formula is the least favorable method of infant feeding and should only be used if other methods are not feasible.
Table 1: The World Health Organization’s hierarchy for infant feeding
| Rank | Type of Milk and Feeding Method |
|---|---|
| First | Human milk fed directly from the birth mother’s breast |
| Second | Human milk pumped from the birth mother and fed through a bottle or other feeding device |
| Third | Pasteurized human milk from an accredited donor bank |
| Fourth | Wet-nurse if acceptable to mother and family |
| Last | Commercial infant formula |
(source: World Health Organization[5])
Most commercial formulas are made from cow’s milk—with vitamins and minerals added to make it resemble human milk—or from soy protein formulated in a similar way. In 1981, after WHO’s concern about the global decrease in breastfeeding, the organization published the “International Code of Marketing Breast-Milk Substitutes.”[6] Their aim was “to contribute to the provision of safe and adequate nutrition for infants, by the protection and promotion of breast-feeding, and by ensuring the proper use of breast-milk substitutes, when these are necessary.”[7] The same year, the Codex Alimentarius established regulations specifying the minimum content of 29 nutrients in infant formula.[8] The regulations have been updated several times to coincide with advances in research on nutrient needs of infants. The Codex requires that infant formula labels include a statement describing the superiority of breastfeeding such as “Breast milk is the best food for your baby.”[9]
Infant Feeding AND GROWTH During the Early Months
Ideally, breast milk should be the only source of food given to infants for the first six months of life, with continued breastfeeding as the baby begins eating cereals and other solid foods. The American Academy of Pediatrics[10] recommends breastfeeding until age one and beyond, whereas WHO[11] and the Canadian Pediatric Society[12] both recommend continuation to two years of agin and beyond. Some mothers define “beyond” as five or six years, a practice criticized by mainstream parents, but acceptable to less traditional parents.
Human milk has the perfect nutrient content for optimal infant growth. Table 2 includes a few of the nutrients found in various mammalian milks. Human milk is much lower in protein and minerals than milk from other mammals, which is the ideal amount needed for a human baby’s growth pattern. Humans grow much more slowly than other mammals, gaining about one ounce per day in the first few months of life, whereas calves add an extra two to three pounds a day, topping out at 500 to 800 pounds by twelve months. A healthy human infant may weigh a mere twenty-one or twenty-two pounds by their first birthday.
Table 2: Comparison of nutrients in mammalian milks per 100 grams
| Nutrient | Human Milk | Cow Milk | Goat Milk | Buffalo Milk |
|---|---|---|---|---|
| Energy (kcal) | 70 | 64 | 69 | 97 |
| Protein (g) | 1.03 | 3.28 | 3.5 | 3.75 |
| Fat (g) | 4.38 | 3.36 | 4.14 | 6.8 |
| Carbohydrate (g) | 6.89 | 4.65 | 4.45 | 5.15 |
| Calcium (mg) | 32 | 119 | 134 | 169 |
| Phosphorus (mg) | 14 | 93 | 111 | 117 |
| Sodium (mg) | 17 | 49 | 50 | 52 |
| Vitamin C (mg) | 5 | 1.5 | 1.3 | 2.3 |
(source: USDA Food Data Central[13])
Background on Preterm Babies
Weight and gestational age at birth reflect the health status and survival rate of newborns. Infants born at or after 38 weeks of gestation are considered full term; those born earlier are pre-term. Birth weights vary by stage of gestation, as noted in Table 3.[14] Based on 2019 U.S. data, slightly less than two percent of infants are born at very low birth weight (less than 1,500 grams). These very small preemies frequently do not survive. Eight percent are low birthweight, weighing less than 2,500 grams.[15] Those weighing at least 3,000 grams are the healthiest, with few complications.
Table 3: Typical infant birthweight by gestational age of infants
| Birthweight Category | Birthweight (g [lbs.]) | Gestational age (wks.) | |
|---|---|---|---|
| Very low birthweight | 1000 (2.2) | 28 | (pre-term) |
| 1500 (3.3) | 31 | ||
| Low birthweight | 2000 (4.4) | 33 | |
| 2500 (5.5) | 35 | ||
| Average birthweight | 3000 (6.6) | 38 | (term) |
| 3500 (7.7) | 40 | ||
| 3700 (8.2) | 42 |
(Adapted from the Utah Department of Health Fetal Growth Chart[16])
Until neonatal intensive care units (NICUs) became common in the 1970s, preemies weighing 1,500 grams or less had a very low chance of surviving. Today, necrotizing enterocolitis (NEC) is a life-threatening intestinal condition occurring in about 10% of these very small infants. The condition, characterized by intestinal inflammation and perforations, often results in death.[17] Neonatologists recognize that giving these babies infant formula worsens NEC; survival is much greater if infants are fed human milk. However, many women who deliver prematurely are unable to produce an adequate amount of milk. Survival of these infants improves when given pasteurized human donor milk.
Nutritional Needs of Young Infants
Infants’ bodies are unable to digest and metabolize the high amounts of protein, calcium, phosphorus, and sodium in milk from cows and other large mammals. Commercial infant formula mimics the low protein and mineral content of human milk. Before the availability of commercial infant formula, infants given cow’s or goat’s milk developed severe diarrhea and eventually died due the damage it caused in their immature bodies. Today’s infants should not be given cow’s milk until at least age one because of this high protein and mineral content.
A woman’s breast milk fulfills her own baby’s nutritional needs, not those of a baby who is older or younger than the child she birthed. Nutrients in breast milk vary by the age and needs of a woman’s biological child, not for the infant of a friend, family member, or complete stranger.
Health Benefits of Human Milk
In addition to the ideal balance of nutrients, human milk is often called “liquid gold” because of the numerous bioactive substances such as hormones, immunoglobulins, probiotics, prebiotics, and oligosaccharides it contains. In addition to the immunoglobulins that are absorbed by the gastrointestinal tract, current research shows the high levels of oligosaccharides contain anti-adhesive properties that may decrease absorption of viruses and bacteria, thereby reducing infections.[18] Even though formula manufacturers claim their products are “closest to mother’s milk” by trying to replicate the nutrient and bioactive ingredients, they will never be able to replicate nature’s nutriment.
Methods of Feeding Human Milk
Although wet-nursing is rare in developed countries, the practice was common from prehistoric time until the early 1900s, when widespread use of infant formula became the norm. In fact, it was the only way to keep infants alive. Throughout history, wealthy families sent their newborns to live with a wet nurse until the child could drink from a cup and eat regular foods. Even poor families turned to wet nurses if the mother died at birth or was too ill to care for her own infant.[19]
Hormonal changes that occur at the delivery of a newborn stimulate milk production in a woman’s breasts. Nutrients are highest in milk produced for the first few months, when infants are growing rapidly, and decrease substantially after six months. Therefore, the ideal wet nurse is one who has recently given birth, when her milk is at its prime. During the 18th and 19th centuries, slave owners throughout the Americas often forced enslaved women who had recently given birth to nurse their wives’ newborns, instead of allowing the slaves to nurse their own infants. This practice often resulted in death of the enslaved infants, who were given cow’s milk or dirty water. [20]
After abolition and slaves were set free, poor women took over as wet nurses for the wealthy. It became a well-organized profession, with doctors often helping wealthy new mothers hire a suitable wet nurse. Because a nursing woman needed to have recently given birth, the woman’s biological infant often suffered because she gave preference to the the paying infant, similar to the fate of enslaved infants.
Today, nursing another woman’s infant is still practiced, although not broadly publicized. Mothers may join an informal nursing co-op and nurse each other’s children, a practice known as cross-nursing. A quick internet search will show the top websites for promoting wet-nurse services, and also for buying and selling expressed milk. Only the Breast[21] and Breast Feeding Moms Unite[22] are two top sites. Of the 3,500 postings on Only the Breast, 17 are for wet nurses.
Chestfeeding
"Chestfeeding" is term and practice that has emerged among people who choose to feed their babies from their chest, but who do not identify with the term breastfeeding for one of a number of reasons. Trans men who have undergone surgery to remove most of their breast tissue ("chest masculinization" or "top" surgery) as well as cis-gender women who have have experienced breast-related trauma often prefer this term. Similarly, a non-binary person may choose not to use the term breastfeeding, given the female-gendered association it carries. If a trans man chooses to retain their uterus and ovaries, pregnancy is possible, and lactation is often possible after delivery. Alternately, some trans women may want to feed an adopted baby, in which case hormone therapy with nipple stimulation can make lactation possible.
Breast Pumps and Expressed Milk
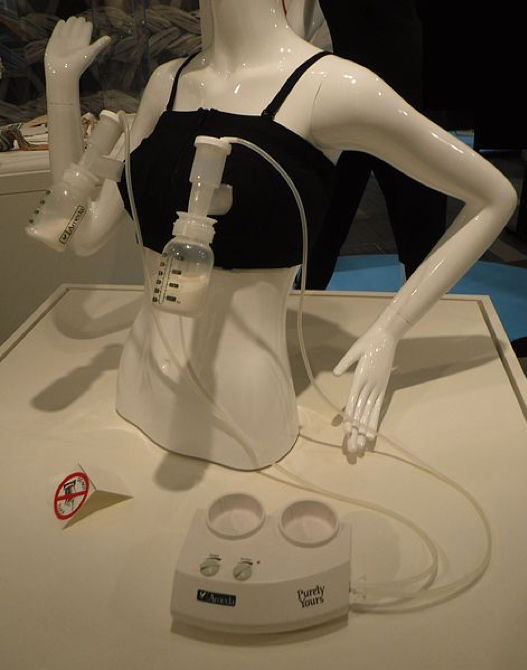
Breast pumps have been around for about 200 years. The earliest ones consisted of a syringe connected to a glass bowl.[23] These early pumps were painful and not efficient in suctioning milk, unlike the double electric pumps available today that work on both breasts simultaneously. (See Figure 1.) In the U.S., the Patient Protection and Affordable Care Act of 2010 requires insurance companies to provide a pump for breastfeeding parents and specifies that employers allow time for women to pump during the workday.[24] The U.S. does not require employers to give paid maternity leave like most other developed countries, resulting in many women returning to work a few weeks after birth. Providing a pump encourages continued breastfeeding throughout the first year.
Women vary in their milk production, with some able to pump an additional 20 to 30 ounces each day after feeding their own babies. Entrepreneurial mothers may choose to sell their surplus milk to other parents as a source of income. Based on Only the Breast postings, most women charge between US$1.00 and US$2.00 per ounce, with vegan milk priced slightly higher.[25] A few altruistic mothers freely give their excess milk, representing a huge savings to parents in need.
One problem with pumping and storing milk is that it loses some nutritional value. Small amounts of nutrients cling to the tube and collection container while pumping. Pouring milk into a plastic bag to freeze, and from there into a bottle for feeding, results in additional nutrient loss. An infant nursing directly from their mother’s own breast thus provides the highest quality nutriment.
The Practice of Milk-Sharing
Research has also been done on the experience of milk-sharing mothers.[26] Representing both milk recipients and milk donors, mothers from various continents shared their opinions about the bonds formed with the donor or recipient, health aspects of giving milk, and opinions of other family members. As they noted:
“In Islamic culture, we have to maintain the relationship because me giving my milk to another baby has created a familial bond [meaning that] my children and my milk children cannot marry one another.” [Donor]
“It gives you kind of a lifelong connection. It’s hard to explain but I look at my son’s ‘milk siblings’ with fondness.” [Donor]
“For so long I was very cynical about life and other people, but being able to be involved in the modern ‘It takes a whole village to raise a baby’ idea has changed my perceptions of what is going on in our society.” [Recipient]
“My son gained 10 pounds in 3 months after we started receiving donor milk. He did not gain any weight his first month of life. He is healthy and happy.” [Recipient]
“I think the only negative repercussions were from my family who [are] not keen on breastfeeding. I got weird looks and disgusted words.” [Recipient]
Unpasteurized Human Milk
Health care experts frown on individuals selling or giving breast milk because it is unpasteurized. Researchers at Ohio State analyzed the microbial content of breast milk bought online. They found bacterial contamination in 75% of the samples, reflecting poor collection, storage, or shipping techniques.[27] Pasteurization would have destroyed the bacteria, making it safe for babies. In another study, the same researchers bought 102 human milk samples; a shocking ten percent contained cow’s milk.[28] Parents buy human milk assuming it is 100 percent human milk, devoid of cow’s milk or other additives. Infants who have a milk allergy may suffer a life-threatening reaction when given the adulterated milk. Some parents may also be tempted to water down their milk to increase profit, resulting in inadequate nutrients and calories.
While pasteurization protects against pathogenic microbes, it has its downside. The high heat processing destroys many of the bioactive substances and vitamin content. In a review of 44 studies that examined the nutrient and bioactive content of pasteurized human, results showed that the immunoglobulins, enzymes, and vitamin C levels were much lower in the pasteurized product than in the fresh milk. However, most other nutrients were unaffected.[29]
Non-Profit Human Milk Banks
Human milk banks are services that accept, pasteurize, and bottle donated breast milk and provide it to the frail pre-term babies in hospital NICUs. The first American milk bank opened in the early 1900s in Boston, after physicians realized that very small infants failed to thrive if given the cow’s milk formula common at the time. The word spread and human milk banking grew steadily in North America. By the 1980s, Canada had 23 milk banks and the U.S. had 30. However, the HIV/AIDS crisis in the mid-1980s resulted in closure in all but one in Canada and the vast majority in the U.S.[30]
In 1985, the Human Milk Banking Association of North America (HMBANA) organized and now accredits nonprofit milk banks in Canada and the U.S. The Association developed international guidelines for pasteurized human donor milk. Canada has four HMBANA-accredited milk banks and the U.S. has 25, with several applying for accreditation.[31] Milk banks face several problems. In addition to health crises (such as the COVID pandemic’s effect of decreasing donations), their operating cost is high. They must pay to screen the mothers, test for purity and bacterial levels in the milk, then pasteurize, bottle, package, store, and ship the final product. As a result, the banks must charge US$4.00 to US$5.00 per ounce for the pasteurized human milk to cover their expenses.[32] A tiny preterm infant may drink only one ounce per feeding, but as they grows, the amount increases to 20 to 30 ounces per day.
Although North American efforts are better than most other countries, Brazil is considered the global leader in donor milk banks:
With a history of the practice dating back to the 1930s, the country also has a three decade-old public health law that stipulates all the steps required to operate a [human donor] bank, based on advice from scientists at the respected research organization, FIOCRUZ. Today, Brazil has 217 milk banks, plus another 126 milk collection points, with at least one bank in each of the country’s 26 states—from Amazonas to São Paulo. Last year, 166,848 Brazilian women donated breast milk; an even larger number of infants reaped the benefits.
This huge system is centrally organized; every state has a reference bank… An online portal called RedeBLH, which has won praise from foreigners, facilitates a vast data collection operation, and enables the public, as well as the government, to stay informed. FIOCRUZ’s Fernandes Figueira Institute—where the national reference bank is kept—also disseminates information via a newsletter, conducts research, and runs undergraduate and graduate programs on policy and applied methodologies for milk banking.[33]
Human Milk for Profit
In contrast to the non-profit endeavors described above, two U.S. companies buy human milk, process it into human milk fortifiers, then sell if for a profit. Both were founded by entrepreneur Elena Medo. Her first was Prolacta® Bioscience, which began in 1999 and sold its first 100% human milk products to hospitals in 2006. The California-based company pays women US$1.00 per ounce for their milk, processes it into a variety of 100% human milk forms, and sells it to hospital NICUs around the world.[34] In 2009, Medo left Prolacta® to form a new company Medolac® that follows a similar model.[35]
The Future of “Human Milk”
The future of commercial ventures for human milk appears to be endless. In 2020, two visionary entrepreneurs introduced “mammary biotechnology” at their North Carolina-based Biomilq™. Their company is developing a process to grow human milk in the lab. The four-step process will include: collecting a woman’s mammary cells; culturing the cells in a lab; collecting the milk made by these cells; and shipping the milk to hungry babies.[36] Their current research focuses on the protein and carbohydrate content of human milk. It will be easy to add the needed vitamins and minerals following the Codex Alimentarius infant formula standards. However, the seemingly unlimited variety of bioactive substances provided in the “liquid gold” secreted from a woman’s real breasts will be more complex, if not impossible, to replicate.
Will the public accept this lab-grown substance as a new form of human breast milk, or will they consider it an artificial substitute? Will the WHO add this type milk to their hierarchy for infant feeding? Will this milk be superior to commercial infant formula or just another expensive alternative? Only time will tell.
Conclusion
Human milk is the sustenance that has allowed civilization to continue; it is considered the gold standard for feeding babies. Originally, infants received the life-saving substance directly from breasts of the birthmother. Today, natural secretion serves as a source of income for some parents and a profitable venture for private industry. It is well known that processing and pasteurizing milk results in losses of many of the beneficial bioactive substances in human milk, yet pasteurization is recommended by all health organizations. Pre-term infants, at high risk of life threatening NEC, depend on the pasteurized human donor milk for survival. Wet-nursing, a practical profession and a major source of income for women in the past, has become taboo (or secretive) in many developed cultures. Is cross-nursing or milk-sharing any different? Would society be healthier if wet nurses became a new and recognized profession or should we wait until biotechnology allows growing “human milk” in a lab to replace human breasts? Although, the future of infant feeding holds many uncertainties, the one universal truth is, infants must be fed to survive.
Discussion Questions
- Breastfeeding mothers of today often produce more milk than is needed to feed one infant, resulting in a surplus of stored milk. Describe three ways a mother with excess expressed breast milk can use the milk, and the protocol she needs to follow in handling the milk.
- Tiny Treasures Milk Bank is Prolacta Bioscience’s route for women to donate (at US$1 per ounce) expressed breast milk. Using their Frequently Asked Questions, answer the following:
- What are the steps a parent must take to donate milk to Tiny Treasures?
- In you were lactating and had a surplus of milk, would you consider “donating” to Tiny Treasures or to your local HMBANA milk bank? Explain your decision.
- In the early 2000s, commercial infant formula in China was found to be adulterated with melamine, resulting in several infant deaths. New working mothers resorted to hiring wet nurses to feed their infants. Image that you were one of these working mothers looking for someone to wet-nurse your infant. Write a posting for the internet, specifying your requirements and the salary you would pay to the wet nurse.
- You adopt a newborn and are told about ways to induce lactation through the use of hormones. Because you work full time, you decide against it. You still want your baby to have the best nutrition possible. Discuss the pros and cons of feeding your infant by the following methods:
- commercial infant formula
- asking a friend who is lactating a 10-month-old to give you breast milk
- buying breast milk from a stranger on the internet
- buying pasteurized 100% human milk from Prolacta
- hiring a wet nurse
Exercise
Breastfeeding and paid maternity/paternity laws vary by country. Select two countries and compare their laws to those of your own country.
- Explain the food system associated with human milk that is being prepared to be sold to a hospital neonatal intensive care unit.
References
“Breastfeeding Moms Unite.” Accessed February 20, 2021.
“Only the Breast.” Accessed February 20, 2021.
Baumgartel, K., L. Sneeringer, and S. Cohen. 2016. “From Royal Wet Nurses to Facebook: The Evolution of Breast Milk Sharing.” Breastfeeding Review: Professional Publication of the Nursing Mothers' Association Of Australia 24 (3): 25–32.
BIOMIQ. 2021. “Unlocking Human Potential with Breakthrough Mammary Biotechnology.” BIOMIQ™ Human Milk for Babies. Accessed May 10, 2021.
Bologna, C. 2020. “200 Years of Breast Pumps: In 18 Images.” Huffington Post. Updated July 30.
Centers for Disease Control and Prevention. 2020. “Breastfeeding: Frequently Asked Questions.” Reviewed May 28, 2020.
Critch, J.N. 2014. Canadian Pediatric Society. Nutrition and Gastroenterology Committee. “Nutrition for Healthy Term Infants, Six to 24 Months: An Overview.” Paediatrics & Child Health 19 (10): 547–52.
Exodus 2:1-9
Food and Agriculture Organization of the United Nations, World Health Organization. 2007. “Standard for Infant Formula and Formulas for Special Medical Purposes Intended for Infants.” Adopted 1981, Amended 1983, 1985, 1987, 2011, 2015, 2016, and 2020. Revised 2007.
Gribble, K. 2018. “'Someone's generosity has formed a bond between us': Interpersonal relationships in Internet-facilitated peer-to-peer milk sharing.” Maternal & child nutrition 14 (Suppl 6): e12575. https://doi.org/10.1111/mcn.12575
Human Milk Bank Association of North America. 2021. Accessed February 20, 2021.
Kapinos, K., L. Bullinger, and T. Gurley-Calvez. 2017 “Lactation Support Services and Breastfeeding Initiation: Evidence from the Affordable Care Act.” Health Services Research ˆ (6): 2175–2196. https://doi.org/10.1111/1475-6773.12598
Keim, S., J. Hogan, K. McNamara, V. Gudimetla, C. Dillon, J. Kwiek, and S. Geraghty. 2013. “Microbial contamination of human milk purchased via the Internet.” Pediatrics 132 (5): e1227-35. https://doi.org/10.1542/peds.2013-1687
Keim, S., M. Kulkarni, K. McNamara, R. Billock, R. Ronau, J. Hogan, and J. Kwiek. 2015 “Cow's Milk Contamination of Human Milk Purchased via the Internet.” Pediatrics 135 (5): e1157-62. https://doi.org/10.1542/peds.2014-3554
Martin, J.A. 2021. “Births: Final Data for 2019.” National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 70 (2): 1–51.
Medolac. 2021. “Human Based Milk for Hospitals.” Medolac® A Public Benefit Corporation. Accessed May 10, 2021.
Moore, R., L. Xu, and S. Townsend. 2021. “Prospecting Human Milk Oligosaccharides as a Defense against Viral Infections.” ACS Infectious Diseases 7 (2): 254–263.
Paynter, M., and K. Hayward. 2018. “Medicine, Body Fluid and Food: The Regulation of Human Donor Milk in Canada.” Healthcare policy = Politiques de santé 13 (3): 20–26. https://doi.org/10.12927/hcpol.2018.25400
Peila, C., G. Moro, E. Bertino, L. Cavallarin, M. Giribaldi, F. Giuliani, F. Cresi, and A. Coscia. 2016.“The Effect of Holder Pasteurization on Nutrients and Biologically-Active Components in Donor Human Milk: A Review.” Nutrients 8 (8): 477. https://doi.org/10.3390/nu8080477
Petherick, A. 2015. “Milk Banks Around the World.”
Prolacta. 2021. “Leader in Human Nutrition.” Prolacta® Bioscience. Accessed February 22, 2021.
Quigley, M., and W. McGuire. 2014. “Formula versus donor breast milk for feeding preterm or low birth weight infants.” The Cochrane Database of Systematic Reviews 4. CD002971. https://doi.org/10.1002/14651858.CD002971.pub3
Slavery Facts. 2019. “Breastfeeding Masters’ Babies: The Wet-Nurse Slave.”
United States Department of Agriculture. 2019. Agriculture Research Service. “Food Data Central.” April 1, 2019.
Utah Dept. of Health. 2021. “Fetal Growth Chart.” Accessed February 20, 2021
World Health Organization. 1981. “International Code of Marketing of Breast-milk Substitutes.” January 28, 1981.
World Health Organization. 2021. “Clinical Management of COVID-19.” Accessed May 10, 2021.
- CCD 2020 ↵
- Exodus 2:1-9. ↵
- WHO 2021. ↵
- WHO 2021. ↵
- WHO 2021. ↵
- WHO 1981. ↵
- WHO 1981. ↵
- FAO 2007. ↵
- FAO 2007. ↵
- CDC 2020. ↵
- WHO 2021. ↵
- Critch 2014. ↵
- USDA 2019. ↵
- Utah Dept. of Health 2021 ↵
- Martin 2021. ↵
- Utah Dept. of Health 2021. ↵
- Quigley 2014. ↵
- Moore et al. 2021. ↵
- Baumgartel et al. 2016. ↵
- Slavery Facts 2019. ↵
- Only the Breast 2021. ↵
- Breastfeeding Moms Unite 2021. ↵
- Bologna 2020. ↵
- Kapinos et al. 2017. ↵
- Only the Breast 2021. ↵
- Gribble 2018. ↵
- Keim et al. 2015. ↵
- Keim et al. 2014. ↵
- Peila et al. 2016. ↵
- Paynter & Hayward 2018. ↵
- Human Milk Bank Assoc. 2021. ↵
- Human Milk Bank Assoc. 2021. ↵
- Petherick 2015. ↵
- Prolacta 2021. ↵
- Medolac 2021. ↵
- BIOMIQ 2021. ↵
(verb) to breastfeed another woman’s infant for pay; (noun) a woman paid to nurse an infant who is not her own.
a depository that collects surplus breast milk from nursing mothers with the intent to pasteurize it and feed it to infants in need.
the practice of donors giving expressed human milk to an unrelated infant.
expressed human milk given to milk banks, who then pasteurize and bottle it.
a prepared food (often in powder or concentrate form), made to resemble human milk, and which is marketed for the feeding of infants.
the international standards, guidelines, and codes of practice regarding food, established by the United Nations.
the practice of breastfeeding other women’s children without pay.

