60 Therapeutic Orientations
Original chapter by Hannah Boettcher, Stefan G. Hofmann, and Q. Jade Wu adapted by the Queen’s University Psychology Department
This Open Access chapter was originally written for the NOBA project. Information on the NOBA project can be found below.
We encourage students to use the “Three-Step Method” for support in their learning. Please find our version of the Three-Step Method, created in collaboration with Queen’s Student Academic Success Services, at the following link: https://sass.queensu.ca/psyc100/
In the past century, a number of psychotherapeutic orientations have gained popularity for treating mental illnesses. This module outlines some of the best-known therapeutic approaches and explains the history, techniques, advantages, and disadvantages associated with each. The most effective modern approach is cognitive behavioral therapy (CBT). We also discuss psychoanalytic therapy, person-centered therapy, and mindfulness-based approaches. Drug therapy and emerging new treatment strategies will also be briefly explored.
Learning Objectives
- Become familiar with the most widely practiced approaches to psychotherapy.
- For each therapeutic approach, consider: history, goals, key techniques, and empirical support.
- Consider the impact of emerging treatment strategies in mental health.
Introduction
The history of mental illness can be traced as far back as 1500 BCE, when the ancient Egyptians noted cases of “distorted concentration” and “emotional distress in the heart or mind” (Nasser, 1987). Today, nearly half of all Americans will experience mental illness at some point in their lives, and mental health problems affect more than one-quarter of the population in any given year (Kessler et al., 2005). Fortunately, a range of psychotherapies exist to treat mental illnesses. This module provides an overview of some of the best-known schools of thought in psychotherapy. Currently, the most effective approach is called Cognitive Behavioral Therapy (CBT); however, other approaches, such as psychoanalytic therapy, person-centered therapy, and mindfulness-based therapies are also used—though the effectiveness of these treatments aren’t as clear as they are for CBT. Throughout this module, note the advantages and disadvantages of each approach, paying special attention to their support by empirical research.
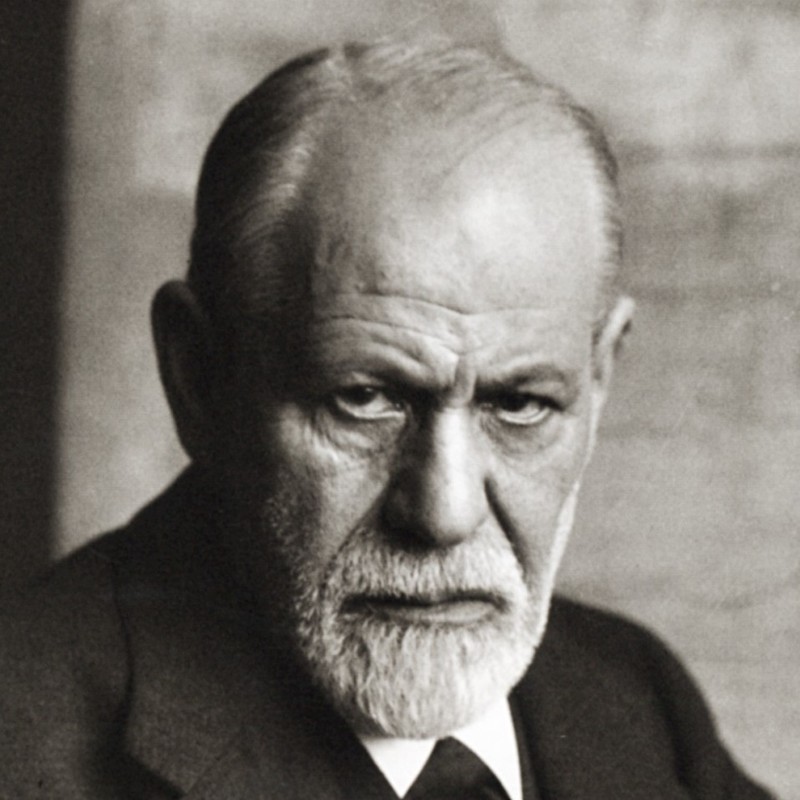
Psychoanalysis and Psychodynamic Therapy
The earliest organized therapy for mental disorders was psychoanalysis. Made famous in the early 20th century by one of the best-known clinicians of all time, Sigmund Freud, this approach stresses that mental health problems are rooted in unconscious conflicts and desires. In order to resolve the mental illness, then, these unconscious struggles must be identified and addressed. Psychoanalysis often does this through exploring one’s early childhood experiences that may have continuing repercussions on one’s mental health in the present and later in life. Psychoanalysis is an intensive, long-term approach in which patients and therapists may meet multiple times per week, often for many years.
History of Psychoanalytic Therapy
Freud initially suggested that mental health problems arise from efforts to push inappropriate sexual urges out of conscious awareness (Freud, 1895/1955). Later, Freud suggested more generally that psychiatric problems are the result of tension between different parts of the mind: the id, the superego, and the ego. In Freud’s structural model, the id represents pleasure-driven unconscious urges (e.g., our animalistic desires for sex and aggression), while the superego is the semi-conscious part of the mind where morals and societal judgment are internalized (e.g., the part of you that automatically knows how society expects you to behave). The ego—also partly conscious—mediates between the id and superego. Freud believed that bringing unconscious struggles like these (where the id demands one thing and the superego another) into conscious awareness would relieve the stress of the conflict (Freud, 1920/1955)—which became the goal of psychoanalytic therapy.
Although psychoanalysis is still practiced today, it has largely been replaced by the more broadly defined psychodynamic therapy. This latter approach has the same basic tenets as psychoanalysis, but is briefer, makes more of an effort to put clients in their social and interpersonal context, and focuses more on relieving psychological distress than on changing the person.
Techniques in Psychoanalysis
Psychoanalysts and psychodynamic therapists employ several techniques to explore patients’ unconscious mind. One common technique is called free association. Here, the patient shares any and all thoughts that come to mind, without attempting to organize or censor them in any way. For example, if you took a pen and paper and just wrote down whatever came into your head, letting one thought lead to the next without allowing conscious criticism to shape what you were writing, you would be doing free association. The analyst then uses their expertise to discern patterns or underlying meaning in the patient’s thoughts.
Sometimes, free association exercises are applied specifically to childhood recollections. That is, psychoanalysts believe a person’s childhood relationships with caregivers often determine the way that person relates to others, and predicts later psychiatric difficulties. Thus, exploring these childhood memories, through free association or otherwise, can provide therapists with insights into a patient’s psychological makeup.
Because we don’t always have the ability to consciously recall these deep memories, psychoanalysts also discuss their patients’ dreams. In Freudian theory, dreams contain not only manifest (or literal) content, but also latent (or symbolic) content (Freud, 1900; 1955). For example, someone may have a dream that their teeth are falling out—the manifest or actual content of the dream. However, dreaming that one’s teeth are falling out could be a reflection of the person’s unconscious concern about losing their physical attractiveness—the latent or metaphorical content of the dream. It is the therapist’s job to help discover the latent content underlying one’s manifest content through dream analysis.
In psychoanalytic and psychodynamic therapy, the therapist plays a receptive role—interpreting the patient’s thoughts and behavior based on clinical experience and psychoanalytic theory. For example, if during therapy a patient begins to express unjustified anger toward the therapist, the therapist may recognize this as an act of transference. That is, the patient may be displacing feelings for people in their life (e.g., anger toward a parent) onto the therapist. At the same time, though, the therapist has to be aware of their own thoughts and emotions, for, in a related process, called countertransference, the therapist may displace their own emotions onto the patient.
The key to psychoanalytic theory is to have patients uncover the buried, conflicting content of their mind, and therapists use various tactics—such as seating patients to face away from them—to promote a freer self-disclosure. And, as a therapist spends more time with a patient, the therapist can come to view their relationship with the patient as another reflection of the patient’s mind.
Advantages and Disadvantages of Psychoanalytic Therapy
Psychoanalysis was once the only type of psychotherapy available, but presently the number of therapists practicing this approach is decreasing around the world. Psychoanalysis is not appropriate for some types of patients, including those with severe psychopathology or intellectual disability. Further, psychoanalysis is often expensive because treatment usually lasts many years. Still, some patients and therapists find the prolonged and detailed analysis very rewarding.
Perhaps the greatest disadvantage of psychoanalysis and related approaches is the lack of empirical support for their effectiveness. The limited research that has been conducted on these treatments suggests that they do not reliably lead to better mental health outcomes (e.g., Driessen et al., 2010). And, although there are some reviews that seem to indicate that long-term psychodynamic therapies might be beneficial (e.g., Leichsenring & Rabung, 2008), other researchers have questioned the validity of these reviews. Nevertheless, psychoanalytic theory was history’s first attempt at formal treatment of mental illness, setting the stage for the more modern approaches used today.
Humanistic and Person-Centered Therapy
One of the next developments in therapy for mental illness, which arrived in the mid-20th century, is called humanistic or person-centered therapy (PCT). Here, the belief is that mental health problems result from an inconsistency between patients’ behavior and their true personal identity. Thus, the goal of PCT is to create conditions under which patients can discover their self-worth, feel comfortable exploring their own identity, and alter their behavior to better reflect this identity.
History of Person-Centered Therapy

PCT was developed by a psychologist named Carl Rogers, during a time of significant growth in the movements of humanistic theory and human potential. These perspectives were based on the idea that humans have an inherent drive to realize and express their own capabilities and creativity. Rogers, in particular, believed that all people have the potential to change and improve, and that the role of therapists is to foster self-understanding in an environment where adaptive change is most likely to occur (Rogers, 1951). Rogers suggested that the therapist and patient must engage in a genuine, egalitarian relationship in which the therapist is nonjudgmental and empathetic. In PCT, the patient should experience both a vulnerability to anxiety, which motivates the desire to change, and an appreciation for the therapist’s support.
Techniques in Person-Centered Therapy
Humanistic and person-centered therapy, like psychoanalysis, involves a largely unstructured conversation between the therapist and the patient. Unlike psychoanalysis, though, a therapist using PCT takes a passive role, guiding the patient toward their own self-discovery. Rogers’s original name for PCT was non-directive therapy, and this notion is reflected in the flexibility found in PCT. Therapists do not try to change patients’ thoughts or behaviors directly. Rather, their role is to provide the therapeutic relationship as a platform for personal growth. In these kinds of sessions, the therapist tends only to ask questions and doesn’t provide any judgment or interpretation of what the patient says. Instead, the therapist is present to provide a safe and encouraging environment for the person to explore these issues for themself.
An important aspect of the PCT relationship is the therapist’s unconditional positive regard for the patient’s feelings and behaviors. That is, the therapist is never to condemn or criticize the patient for what s/he has done or thought; the therapist is only to express warmth and empathy. This creates an environment free of approval or disapproval, where patients come to appreciate their value and to behave in ways that are congruent with their own identity.
Advantages and Disadvantages of Person-Centered Therapy
One key advantage of person-centered therapy is that it is highly acceptable to patients. In other words, people tend to find the supportive, flexible environment of this approach very rewarding. Furthermore, some of the themes of PCT translate well to other therapeutic approaches. For example, most therapists of any orientation find that clients respond well to being treated with nonjudgmental empathy. The main disadvantage to PCT, however, is that findings about its effectiveness are mixed. One possibility for this could be that the treatment is primarily based on unspecific treatment factors. That is, rather than using therapeutic techniques that are specific to the patient and the mental problem (i.e., specific treatment factors), the therapy focuses on techniques that can be applied to anyone (e.g., establishing a good relationship with the patient) (Cuijpers et al., 2012; Friedli, King, Lloyd, & Horder, 1997). Similar to how “one-size-fits-all” doesn’t really fit every person, PCT uses the same practices for everyone, which may work for some people but not others. Further research is necessary to evaluate its utility as a therapeutic approach.
Cognitive Behavioral Therapy
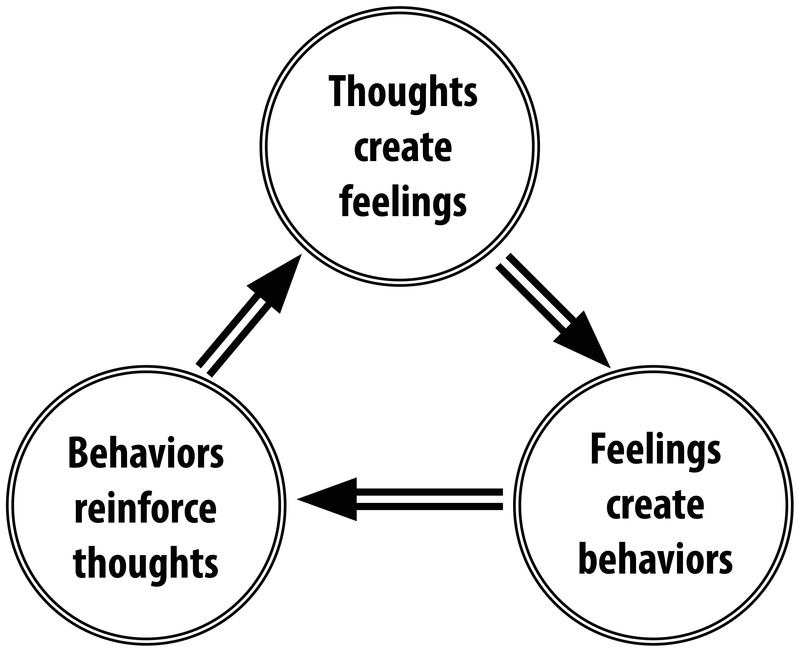
Although both psychoanalysis and PCT are still used today, another therapy, cognitive-behavioral therapy (CBT), has gained more widespread support and practice. CBT refers to a family of therapeutic approaches whose goal is to alleviate psychological symptoms by changing their underlying cognitions and behaviors. The premise of CBT is that thoughts, behaviors, and emotions interact and contribute to various mental disorders. For example, let’s consider how a CBT therapist would view a patient who compulsively washes their hands for hours every day. First, the therapist would identify the patient’s maladaptive thought: “If I don’t wash my hands like this, I will get a disease and die.” The therapist then identifies how this maladaptive thought leads to a maladaptive emotion: the feeling of anxiety when their hands aren’t being washed. And finally, this maladaptive emotion leads to the maladaptive behavior: the patient washing their hands for hours every day.
CBT is a present-focused therapy (i.e., focused on the “now” rather than causes from the past, such as childhood relationships) that uses behavioral goals to improve one’s mental illness. Often, these behavioral goals involve between-session homework assignments. For example, the therapist may give the hand-washing patient a worksheet to take home; on this worksheet, the patient is to write down every time they feel the urge to wash their hands, how they deal with the urge, and what behavior they replace that urge with. When the patient has their next therapy session, the patient and the therapist review the patient’s “homework” together. CBT is a relatively brief intervention of 12 to 16 weekly sessions, closely tailored to the nature of the psychopathology and treatment of the specific mental disorder. And, as the empirical data shows, CBT has proven to be highly efficacious for virtually all psychiatric illnesses (Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012).
History of Cognitive Behavioral Therapy
CBT developed from clinical work conducted in the mid-20th century by Dr. Aaron T. Beck, a psychiatrist, and Albert Ellis, a psychologist. Beck used the term automatic thoughts to refer to the thoughts depressed patients report experiencing spontaneously. He observed that these thoughts arise from three belief systems, or schemas: beliefs about the self, beliefs about the world, and beliefs about the future. In treatment, therapy initially focuses on identifying automatic thoughts (e.g., “If I don’t wash my hands constantly, I’ll get a disease”), testing their validity, and replacing maladaptive thoughts with more adaptive thoughts (e.g., “Washing my hands three times a day is sufficient to prevent a disease”). In later stages of treatment, the patient’s maladaptive schemas are examined and modified. Ellis (1957) took a comparable approach, in what he called rational-emotive-behavioral therapy (REBT), which also encourages patients to evaluate their own thoughts about situations.
Techniques in CBT
Beck and Ellis strove to help patients identify maladaptive appraisals, or the untrue judgments and evaluations of certain thoughts. For example, if it’s your first time meeting new people, you may have the automatic thought, “These people won’t like me because I have nothing interesting to share.” That thought itself is not what’s troublesome; the appraisal (or evaluation) that it might have merit is what’s troublesome. The goal of CBT is to help people make adaptive, instead of maladaptive, appraisals (e.g., “I do know interesting things!”). This technique of reappraisal, or cognitive restructuring, is a fundamental aspect of CBT. With cognitive restructuring, it is the therapist’s job to help point out when a person has an inaccurate or maladaptive thought, so that the patient can either eliminate it or modify it to be more adaptive.
In addition to thoughts, though, another important treatment target of CBT is maladaptive behavior. Every time a person engages in maladaptive behavior (e.g., never speaking to someone in new situations), he or she reinforces the validity of the maladaptive thought, thus maintaining or perpetuating the psychological illness. In treatment, the therapist and patient work together to develop healthy behavioral habits (often tracked with worksheet-like homework), so that the patient can break this cycle of maladaptive thoughts and behaviors.
For many mental health problems, especially anxiety disorders, CBT incorporates what is known as exposure therapy. During exposure therapy, a patient confronts a problematic situation and fully engages in the experience instead of avoiding it. For example, imagine a person who is terrified of spiders. Whenever they encounter one, they immediately scream and panic. In exposure therapy, the patient would be forced to confront and interact with spiders, rather than simply avoiding them as they usually do. The goal is to reduce the fear associated with the situation through extinction learning, a neurobiological and cognitive process by which the patient “unlearns” the irrational fear. For example, exposure therapy for someone terrified of spiders might begin with them looking at a cartoon of a spider, followed by looking at pictures of real spiders, and later, the patient handling a plastic spider. After weeks of this incremental exposure, the patient may even be able to hold a live spider. After repeated exposure (starting small and building one’s way up), the patient experiences less physiological fear and maladaptive thoughts about spiders, breaking their tendency for anxiety and subsequent avoidance.
Advantages and Disadvantages of CBT
CBT interventions tend to be relatively brief, making them cost-effective for the average consumer. In addition, CBT is an intuitive treatment that makes logical sense to patients. It can also be adapted to suit the needs of many different populations. One disadvantage, however, is that CBT does involve significant effort on the patient’s part, because the patient is an active participant in treatment. Therapists often assign “homework” (e.g., worksheets for recording one’s thoughts and behaviors) between sessions to maintain the cognitive and behavioral habits the patient is working on. The greatest strength of CBT is the abundance of empirical support for its effectiveness. Studies have consistently found CBT to be equally or more effective than other forms of treatment, including medication and other therapies (Butler, Chapman, Forman, & Beck, 2006; Hofmann et al., 2012). For this reason, CBT is considered a first-line treatment for many mental disorders.
The central notion of CBT is the idea that a person’s behavioral and emotional responses are causally influenced by one’s thinking. The stoic Greek philosopher Epictetus is quoted as saying, “men are not moved by things, but by the view they take of them.” Meaning, it is not the event per se, but rather one’s assumptions (including interpretations and perceptions) of the event that are responsible for one’s emotional response to it. Beck calls these assumptions about events and situations automatic thoughts (Beck, 1979), whereas Ellis (1962) refers to these assumptions as self-statements. The cognitive model assumes that these cognitive processes cause the emotional and behavioral responses to events or stimuli. This causal chain is illustrated in Ellis’s ABC model, in which A stands for the antecedent event, B stands for belief, and C stands for consequence. During CBT, the person is encouraged to carefully observe the sequence of events and the response to them, and then explore the validity of the underlying beliefs through behavioral experiments and reasoning, much like a detective or scientist.
Acceptance and Mindfulness-Based Approaches
Unlike the preceding therapies, which were developed in the 20th century, this next one was born out of age-old Buddhist and yoga practices. Mindfulness, or a process that tries to cultivate a nonjudgmental, yet attentive, mental state, is a therapy that focuses on one’s awareness of bodily sensations, thoughts, and the outside environment. Whereas other therapies work to modify or eliminate these sensations and thoughts, mindfulness focuses on nonjudgmentally accepting them (Kabat-Zinn, 2003; Baer, 2003). For example, whereas CBT may actively confront and work to change a maladaptive thought, mindfulness therapy works to acknowledge and accept the thought, understanding that the thought is spontaneous and not what the person truly believes. There are two important components of mindfulness: (1) self-regulation of attention, and (2) orientation toward the present moment (Bishop et al., 2004). Mindfulness is thought to improve mental health because it draws attention away from past and future stressors, encourages acceptance of troubling thoughts and feelings, and promotes physical relaxation.
Techniques in Mindfulness-Based Therapy
Psychologists have adapted the practice of mindfulness as a form of psychotherapy, generally called mindfulness-based therapy (MBT). Several types of MBT have become popular in recent years, including mindfulness-based stress reduction (MBSR) (e.g., Kabat-Zinn, 1982) and mindfulness-based cognitive therapy (MBCT) (e.g., Segal, Williams, & Teasdale, 2002).

MBSR uses meditation, yoga, and attention to physical experiences to reduce stress. The hope is that reducing a person’s overall stress will allow that person to more objectively evaluate their thoughts. In MBCT, rather than reducing one’s general stress to address a specific problem, attention is focused on one’s thoughts and their associated emotions. For example, MBCT helps prevent relapses in depression by encouraging patients to evaluate their own thoughts objectively and without value judgment (Baer, 2003). Although cognitive behavioral therapy (CBT) may seem similar to this, it focuses on “pushing out” the maladaptive thought, whereas mindfulness-based cognitive therapy focuses on “not getting caught up” in it. The treatments used in MBCT have been used to address a wide range of illnesses, including depression, anxiety, chronic pain, coronary artery disease, and fibromyalgia (Hofmann, Sawyer, Witt & Oh, 2010).
Mindfulness and acceptance—in addition to being therapies in their own right—have also been used as “tools” in other cognitive-behavioral therapies, particularly in dialectical behavior therapy (DBT) (e.g., Linehan, Amstrong, Suarez, Allmon, & Heard, 1991). DBT, often used in the treatment of borderline personality disorder, focuses on skills training. That is, it often employs mindfulness and cognitive behavioral therapy practices, but it also works to teach its patients “skills” they can use to correct maladaptive tendencies. For example, one skill DBT teaches patients is called distress tolerance—or, ways to cope with maladaptive thoughts and emotions in the moment. For example, people who feel an urge to cut themselves may be taught to snap their arm with a rubber band instead. The primary difference between DBT and CBT is that DBT employs techniques that address the symptoms of the problem (e.g., cutting oneself) rather than the problem itself (e.g., understanding the psychological motivation to cut oneself). CBT does not teach such skills training because of the concern that the skills—even though they may help in the short-term—may be harmful in the long-term, by maintaining maladaptive thoughts and behaviors.
DBT is founded on the perspective of a dialectical worldview. That is, rather than thinking of the world as “black and white,” or “only good and only bad,” it focuses on accepting that some things can have characteristics of both “good” and “bad.” So, in a case involving maladaptive thoughts, instead of teaching that a thought is entirely bad, DBT tries to help patients be less judgmental of their thoughts (as with mindfulness-based therapy) and encourages change through therapeutic progress, using cognitive-behavioral techniques as well as mindfulness exercises.
Another form of treatment that also uses mindfulness techniques is acceptance and commitment therapy (ACT) (Hayes, Strosahl, & Wilson, 1999). In this treatment, patients are taught to observe their thoughts from a detached perspective (Hayes et al., 1999). ACT encourages patients not to attempt to change or avoid thoughts and emotions they observe in themselves, but to recognize which are beneficial and which are harmful. However, the differences among ACT, CBT, and other mindfulness-based treatments are a topic of controversy in the current literature.
Advantages and Disadvantages of Mindfulness-Based Therapy
Two key advantages of mindfulness-based therapies are their acceptability and accessibility to patients. Because yoga and meditation are already widely known in popular culture, consumers of mental healthcare are often interested in trying related psychological therapies. Currently, psychologists have not come to a consensus on the efficacy of MBT, though growing evidence supports its effectiveness for treating mood and anxiety disorders. For example, one review of MBT studies for anxiety and depression found that mindfulness-based interventions generally led to moderate symptom improvement (Hofmann et al., 2010).
Emerging Treatment Strategies

With growth in research and technology, psychologists have been able to develop new treatment strategies in recent years. Often, these approaches focus on enhancing existing treatments, such as cognitive-behavioral therapies, through the use of technological advances. For example, internet-and mobile-delivered therapies make psychological treatments more available, through smartphones and online access. Clinician-supervised online CBT modules allow patients to access treatment from home on their own schedule—an opportunity particularly important for patients with less geographic or socioeconomic access to traditional treatments. Furthermore, smartphones help extend therapy to patients’ daily lives, allowing for symptom tracking, homework reminders, and more frequent therapist contact.
Another benefit of technology is cognitive bias modification. Here, patients are given exercises, often through the use of video games, aimed at changing their problematic thought processes. For example, researchers might use a mobile app to train alcohol abusers to avoid stimuli related to alcohol. One version of this game flashes four pictures on the screen—three alcohol cues (e.g., a can of beer, the front of a bar) and one health-related image (e.g., someone drinking water). The goal is for the patient to tap the healthy picture as fast as s/he can. Games like these aim to target patients’ automatic, subconscious thoughts that may be difficult to direct through conscious effort. That is, by repeatedly tapping the healthy image, the patient learns to “ignore” the alcohol cues, so when those cues are encountered in the environment, they will be less likely to trigger the urge to drink. Approaches like these are promising because of their accessibility, however they require further research to establish their effectiveness.
Yet another emerging treatment employs CBT-enhancing pharmaceutical agents. These are drugs used to improve the effects of therapeutic interventions. Based on research from animal experiments, researchers have found that certain drugs influence the biological processes known to be involved in learning. Thus, if people take these drugs while going through psychotherapy, they are better able to “learn” the techniques for improvement. For example, the antibiotic d-cycloserine improves treatment for anxiety disorders by facilitating the learning processes that occur during exposure therapy. Ongoing research in this exciting area may prove to be quite fruitful.
Pharmacological Treatments
Up until this point, all the therapies we have discussed have been talk-based or meditative practices. However, psychiatric medications are also frequently used to treat mental disorders, including schizophrenia, bipolar disorder, depression, and anxiety disorders. Psychiatric drugs are commonly used, in part, because they can be prescribed by general medical practitioners, whereas only trained psychologists are qualified to deliver effective psychotherapy. While drugs and CBT therapies tend to be almost equally effective, choosing the best intervention depends on the disorder and individual being treated, as well as other factors—such as treatment availability and comorbidity (i.e., having multiple mental or physical disorders at once). Although many new drugs have been introduced in recent decades, there is still much we do not understand about their mechanism in the brain. Further research is needed to refine our understanding of both pharmacological and behavioral treatments before we can make firm claims about their effectiveness.
Integrative and Eclectic Psychotherapy
In discussing therapeutic orientations, it is important to note that some clinicians incorporate techniques from multiple approaches, a practice known as integrative or eclectic psychotherapy. For example, a therapist may employ distress tolerance skills from DBT (to resolve short-term problems), cognitive reappraisal from CBT (to address long-standing issues), and mindfulness-based meditation from MBCT (to reduce overall stress). And, in fact, between 13% and 42% of therapists have identified their own approaches as integrative or eclectic (Norcross & Goldfried, 2005).
Conclusion
Throughout human history we have had to deal with mental illness in one form or another. Over time, several schools of thought have emerged for treating these problems. Although various therapies have been shown to work for specific individuals, cognitive behavioral therapy is currently the treatment most widely supported by empirical research. Still, practices like psychodynamic therapies, person-centered therapy, mindfulness-based treatments, and acceptance and commitment therapy have also shown success. And, with recent advances in research and technology, clinicians are able to enhance these and other therapies to treat more patients more effectively than ever before. However, what is important in the end is that people actually seek out mental health specialists to help them with their problems. One of the biggest deterrents to doing so is that people don’t understand what psychotherapy really entails. Through understanding how current practices work, not only can we better educate people about how to get the help they need, but we can continue to advance our treatments to be more effective in the future.
Check Your Knowledge
To help you with your studying, we’ve included some practice questions for this module. These questions do not necessarily address all content in this module. They are intended as practice, and you are responsible for all of the content in this module even if there is no associated practice question. To promote deeper engagement with the material, we encourage you to create some questions of your own for your practice. You can then also return to these self-generated questions later in the course to test yourself.
Vocabulary
- Acceptance and commitment therapy
- A therapeutic approach designed to foster nonjudgmental observation of one’s own mental processes.
- Automatic thoughts
- Thoughts that occur spontaneously; often used to describe problematic thoughts that maintain mental disorders.
- Cognitive bias modification
- Using exercises (e.g., computer games) to change problematic thinking habits.
- Cognitive-behavioral therapy (CBT)
- A family of approaches with the goal of changing the thoughts and behaviors that influence psychopathology.
- Comorbidity
- Describes a state of having more than one psychological or physical disorder at a given time.
- Dialectical behavior therapy (DBT)
- A treatment often used for borderline personality disorder that incorporates both cognitive-behavioral and mindfulness elements.
- Dialectical worldview
- A perspective in DBT that emphasizes the joint importance of change and acceptance.
- Exposure therapy
- A form of intervention in which the patient engages with a problematic (usually feared) situation without avoidance or escape.
- Free association
- In psychodynamic therapy, a process in which the patient reports all thoughts that come to mind without censorship, and these thoughts are interpreted by the therapist.
- Integrative or eclectic psychotherapy
- Also called integrative psychotherapy, this term refers to approaches combining multiple orientations (e.g., CBT with psychoanalytic elements).
- Integrative or eclectic psychotherapy
- Also called integrative psychotherapy, this term refers to approaches combining multiple orientations (e.g., CBT with psychoanalytic elements).
- Mindfulness
- A process that reflects a nonjudgmental, yet attentive, mental state.
- Mindfulness-based therapy
- A form of psychotherapy grounded in mindfulness theory and practice, often involving meditation, yoga, body scan, and other features of mindfulness exercises.
- Person-centered therapy
- A therapeutic approach focused on creating a supportive environment for self-discovery.
- Psychoanalytic therapy
- Sigmund Freud’s therapeutic approach focusing on resolving unconscious conflicts.
- Psychodynamic therapy
- Treatment applying psychoanalytic principles in a briefer, more individualized format.
- Reappraisal, or Cognitive restructuring
- The process of identifying, evaluating, and changing maladaptive thoughts in psychotherapy.
- Schema
- A mental representation or set of beliefs about something.
- Unconditional positive regard
- In person-centered therapy, an attitude of warmth, empathy and acceptance adopted by the therapist in order to foster feelings of inherent worth in the patient.
References
- Baer, R. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143.
- Beck, A. T. (1979). Cognitive therapy and the emotional disorders. New York, NY: New American Library/Meridian.
- Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241.
- Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26, 17–31.
- Cuijpers, P., Driessen, E., Hollon, S.D., van Oppen, P., Barth, J., & Andersson, G. (2012). The efficacy of non-directive supportive therapy for adult depression: A meta-analysis. Clinical Psychology Review, 32, 280–291.
- Driessen, E., Cuijpers, P., de Maat, S. C. M., Abbass, A. A., de Jonghe, F., & Dekker, J. J. M. (2010). The efficacy of short-term psychodynamic psychotherapy for depression: A meta-analysis. Clinical Psychology Review, 30, 25–36.
- Ellis, A. (1962). Reason and emotion in psychotherapy. New York, NY: Lyle Stuart.
- Ellis, A. (1957). Rational psychotherapy and individual psychology. Journal of Individual Psychology, 13, 38–44.
- Freud, S. (1955). The interpretation of dreams. London, UK: Hogarth Press (Original work published 1900).
- Freud, S. (1955). Studies on hysteria. London, UK: Hogarth Press (Original work published 1895).
- Freud. S. (1955). Beyond the pleasure principle. H London, UK: Hogarth Press (Original work published 1920).
- Friedli, K., King, M. B., Lloyd, M., & Horder, J. (1997). Randomized controlled assessment of non-directive psychotherapy versus routine general-practitioner care. Lancet, 350,\\n1662–1665.
- Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and Commitment Therapy. New\\nYork, NY: Guilford Press.
- Hofmann, S. G., Asnaani, A., Vonk, J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36, 427–440.
- Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183
- Kabat-Zinn J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156.
- Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients\\nbased on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47.
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age of onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602.
- Leichsenring, F., & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. Journal of the American Medical Association, 300,1551–1565.
- Linehan, M. M., Amstrong, H.-E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically suicidal borderline patients. Archives of General Psychiatry, 48, 1060–1064.
- Nasser, M. (1987). Psychiatry in ancient Egypt. Bulletin of the Royal College of Psychiatrists, 11, 420-422.
- Norcross, J. C. & Goldfried, M. R. (2005). Handbook of Psychotherapy Integration. New York, NY: Oxford University Press.
- Rogers, C. (1951). Client-Centered Therapy. Cambridge, MA: Riverside Press.
- Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-Based Cognitive Therapy\\nfor Depression: A New Approach to Preventing Relapse. New York, NY: Guilford Press.
How to cite this Chapter using APA Style:
Boettcher, H., Hofmann, S. G., & Wu, Q. J. (2019). Therapeutic orientations. Adapted for use by Queen’s University. Original chapter in R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Retrieved from http://noba.to/fjtnpwsk
Copyright and Acknowledgment:
This material is licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. To view a copy of this license, visit: http://creativecommons.org/licenses/by-nc-sa/4.0/deed.en_US.
This material is attributed to the Diener Education Fund (copyright © 2018) and can be accessed via this link: http://noba.to/fjtnpwsk.
Additional information about the Diener Education Fund (DEF) can be accessed here.
Nasser, M. (1987). Psychiatry in ancient Egypt. Bulletin of the Royal College of Psychiatrists, 11, 420-422.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age of onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602.
Freud, S. (1955). Studies on hysteria. London, UK: Hogarth Press (Original work published 1895).
Freud. S. (1955). Beyond the pleasure principle. H London, UK: Hogarth Press (Original work published 1920).
Sigmund Freud’s therapeutic approach focusing on resolving unconscious conflicts.
Treatment applying psychoanalytic principles in a briefer, more individualized format.
In psychodynamic therapy, a process in which the patient reports all thoughts that come to mind without censorship, and these thoughts are interpreted by the therapist.
Freud, S. (1955). The interpretation of dreams. London, UK: Hogarth Press (Original work published 1900).
Driessen, E., Cuijpers, P., de Maat, S. C. M., Abbass, A. A., de Jonghe, F., & Dekker, J. J. M. (2010). The efficacy of short-term psychodynamic psychotherapy for depression: A meta-analysis. Clinical Psychology Review, 30, 25–36.
Leichsenring, F., & Rabung, S. (2008). Effectiveness of long-term psychodynamic psychotherapy: A meta-analysis. Journal of the American Medical Association, 300,1551–1565.
A therapeutic approach focused on creating a supportive environment for self-discovery.
Rogers, C. (1951). Client-Centered Therapy. Cambridge, MA: Riverside Press.
In person-centered therapy, an attitude of warmth, empathy and acceptance adopted by the therapist in order to foster feelings of inherent worth in the patient.
Cuijpers, P., Driessen, E., Hollon, S.D., van Oppen, P., Barth, J., & Andersson, G. (2012). The efficacy of non-directive supportive therapy for adult depression: A meta-analysis. Clinical Psychology Review, 32, 280–291.
Friedli, K., King, M. B., Lloyd, M., & Horder, J. (1997). Randomized controlled assessment of non-directive psychotherapy versus routine general-practitioner care. Lancet, 350,\\n1662–1665.
A family of approaches with the goal of changing the thoughts and behaviors that influence psychopathology.
Hofmann, S. G., Asnaani, A., Vonk, J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36, 427–440.
Thoughts that occur spontaneously; often used to describe problematic thoughts that maintain mental disorders.
A mental representation or set of beliefs about something.
Ellis, A. (1957). Rational psychotherapy and individual psychology. Journal of Individual Psychology, 13, 38–44.
The process of identifying, evaluating, and changing maladaptive thoughts in psychotherapy.
A form of intervention in which the patient engages with a problematic (usually feared) situation without avoidance or escape.
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26, 17–31.
Hofmann, S. G., Asnaani, A., Vonk, J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36, 427–440.
Beck, A. T. (1979). Cognitive therapy and the emotional disorders. New York, NY: New American Library/Meridian.
Ellis, A. (1962). Reason and emotion in psychotherapy. New York, NY: Lyle Stuart.
A process that reflects a nonjudgmental, yet attentive, mental state.
Kabat-Zinn J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156.
Baer, R. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143.
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241.
A form of psychotherapy grounded in mindfulness theory and practice, often involving meditation, yoga, body scan, and other features of mindfulness exercises.
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients\\nbased on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-Based Cognitive Therapy\\nfor Depression: A New Approach to Preventing Relapse. New York, NY: Guilford Press.
Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183
A treatment often used for borderline personality disorder that incorporates both cognitive-behavioral and mindfulness elements.
Linehan, M. M., Amstrong, H.-E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically suicidal borderline patients. Archives of General Psychiatry, 48, 1060–1064.
A perspective in DBT that emphasizes the joint importance of change and acceptance.
A therapeutic approach designed to foster nonjudgmental observation of one’s own mental processes.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and Commitment Therapy. New\\nYork, NY: Guilford Press.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and Commitment Therapy. New\\nYork, NY: Guilford Press.
Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183
Using exercises (e.g., computer games) to change problematic thinking habits.
Describes a state of having more than one psychological or physical disorder at a given time.
Also called integrative psychotherapy, this term refers to approaches combining multiple orientations (e.g., CBT with psychoanalytic elements).
Norcross, J. C. & Goldfried, M. R. (2005). Handbook of Psychotherapy Integration. New York, NY: Oxford University Press.

