4 Interprofessional Communication
Watch or Listen to the Following Media Clip
Learning Objectives
- Recognize the role of interprofessional communication in health care settings.
- Describe the elements and goals of interprofessional communication.
- Explore behavioural practices influencing interprofessional care teams.
- Apply strategies for managing conflict within the context of interprofessional teams.
Introduction
Interprofessional communication occurs when health professionals communicate with each other, with patients, their families, and with the community in general. Multidisciplinary or interdisciplinary are terms used to describe the makeup of health care teams. Individuals from different health care disciplines approach a patient or care of a patient from their own perspective. The primary goal of these teams is to integrate expertise from separate disciplines into a single consultation to support patient care and outcomes. This encompassing care is often referred to using the short form IPC meaning interprofessional care.
Assessing What You Already Know
Consider your pre-existing knowledge surrounding interprofessional teams as you complete this activity
Role of Interprofessional Communication in Health Care
As the nature of health care continues to evolve the more interwoven health care professionals are in coordinating care following an interprofessional-focused approach. In the past health care management was often physician or disease-focused. Recently, this foundation has since migrated to a robust team of health professionals working together for patient care and disease prevention. This seemingly harmonious approach will not occur without reflective practice, mindful effort, and understanding the importance of communication. Learning to function effectively within the interprofessional dynamic begins through the establishment of mutual respect and trust.
Establishing Trust-Interprofessional Practices
As a self-check consider the following definition as well as the reflective questions within the context of communication.
Trust (noun): Belief in the reliability, truth, ability or strength of someone or something, as in “good relationships are built on trust.”—Oxford English Dictionary
Questions for reflection:
- Does my personal competence and follow through establish trust with others?
- What experiences can I offer to support cooperation while working with others?
- How do I manage stressful communication-based situations with others?
Elements of Interprofessional Communication
Six interdependent competency domains have been identified to achieve the goal of interprofessional collaboration (Canadian Interprofessional Health Collaborative CIHC, 2010, as cited Garmaise-Yee et al., 2020) ). These are defined as the “knowledge, skills, attitudes, and values that shape the judgements essential for interprofessional practice” (Canadian Interprofessional Health Collaborative, 2010; as cited in Garmaise-Yee et al., 2020) and include:
- Interprofessional communication
- Patient/client/family/community-centred care
- Role clarification
- Team functioning
- Interprofessional conflict resolution
- Collaborative leadership
The first two competencies, interprofessional communication and patient/client/family/community-centred care have a strong influencing role in all healthcare situations, so as shown in figure 4.1, they encircle the other four competencies. The next section explores the 6 competencies further.
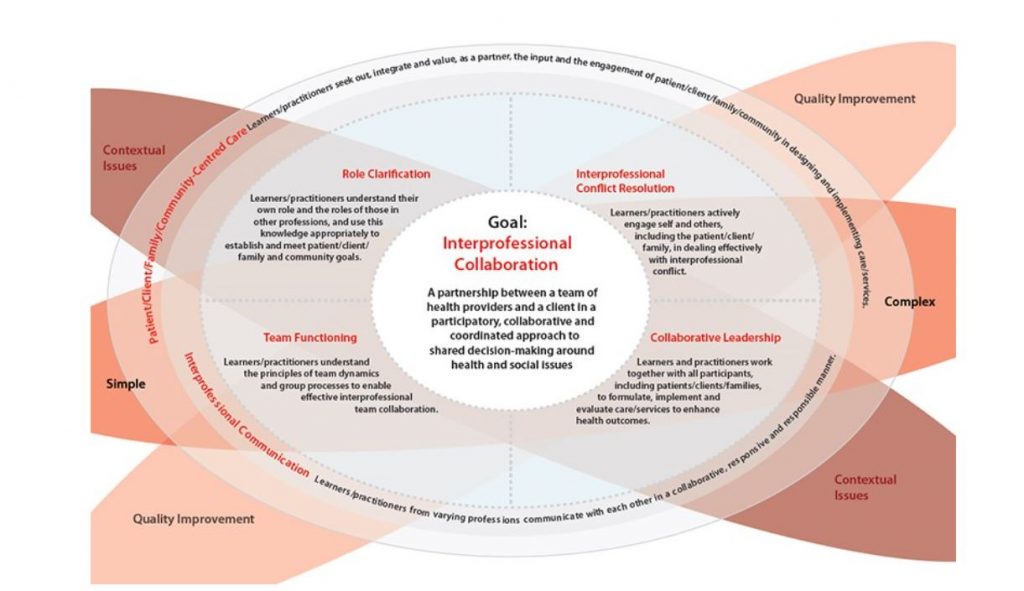
The first two competencies, interprofessional communication and patient/client/family/community-centred care have a strong influencing role in all healthcare situations, so as shown in figure 4.1, they encircle the other four competencies. According to the Centre for Interprofessional Education, Toronto Academic Health Science Centre (2017) the six competencies identified are explained further as outlined in the next section.
Interprofessional Communication Competency
Explored in the Professional Communication chapter elements of effective communication apply relative to interprofessional communication.
Behavioural examples to strengthen interprofessional communication include the following:
- communicate clearly using terminology understood by the collaborative team, patients, and family
- ensure complete information is provided as directed
- be responsive to changing needs and circumstances
- provide information in a timely manner, avoid withholding sensitive information
- use recognized and accepted communication channels (checklists and templates are helpful)
- review updated information when it is available
- demonstrate respect with all members of the interprofessional team
- model and create an environment of mutual trust, respect for privacy and confidentiality, while maintaining patient dignity
Patient/Client/Family/Community-Centred Care Competency
Patient-centred care encircles the foundational belief clients/patients and their families are partners in the design and development of care plans, all functioning as members of one team. Input is gathered collaboratively from team members to support engagement through each stage and process of care plan implementation.
Behavioural examples of patient-centred care involve:
- actively seeking clarification from patients, their families, and the interprofessional team when involved with the planning, coordination, and implementation of patient care plans
- support and encourage access to community resources and involvement
- promote access to preventive care measures by applying therapeutic communication strategies and information sharing
Role Clarification Competency
This involves developing an understanding of your role and the role of all collaborative professionals on the team. The ability to apply this knowledge correctly achieves care goals for patients and supports the health of the community within the bigger picture. This understanding helps to identify gaps in care, addresses duplication of resources, and enhances the implementation of care plans. The HCA can model a variety of behaviours to support this.
Behavioural examples of role clarification include:
- demonstrate an understanding of your own role as well as the roles of each member of the team
- consider the roles of members while respecting the diversity of the team members as they relate to patient care and team dynamics
- utilize professional development opportunities to expand knowledge of interprofessional educational practices
- practice self-awareness in view of one’s own limitations and the need for consultation with other members of the healthcare team based on roles and professional scope
Team Functioning Competency
When interprofessional health care teams form it is common practice to establish ground rules of how the team will work together.
Behavioural examples of team functioning include:
- Recognize and share with the interprofessional team individual and systemic power discrepancies and gaps expressed by patients and their families.
- Participate in the development of team values and goals.
- Support team psychological safety to establish a sense of confidence that the team will not embarrass, reject or punish someone for speaking up.
- Advocate against and avoid harmful behaviour to a team i.e. gossip, destructive comments rumours that impact team morale and development.
Interprofessional Conflict Competency
Conflict is a natural event occurring when groups or teams are working together. Joan Wagner provided this insight from the publication Leadership and Influencing Change in Nursing, for centuries, people accepted adversarial disputes and harsh conflict as a by-product of human nature. This acceptance caused people to analyze only how conflict could be resolved, that is, how they could make it go away (Wagner, 2018).
Conflicts and disagreements are inevitable with interpersonal communication. Several factors that influence conflict can include, role boundary concerns, accountability and the scope of practice of those involved in the communication stream. Recognizing and managing conflict effectively supports therapeutic communication goals.
Types of Conflict
Categorizing and understanding the types of conflict arising assists with framing resolutions. Here are four types of common conflict occurring within interprofessional teams (Wagner. J. 2018).
- Data/Information. These encompass elements inclusive of, lack of information, interpretation of information, incomplete information, and differing assessment procedures.
- Values. Conflicts related to day-to-day values and self-definition.
- Relationship. These conflicts stem from stereotypes, misperceptions, and poor communication efforts.
- Structural. Conflicts relate to how a situation occurs, who is involved in the decision-making, and unequal power and authority (Wagner. J. 2018).
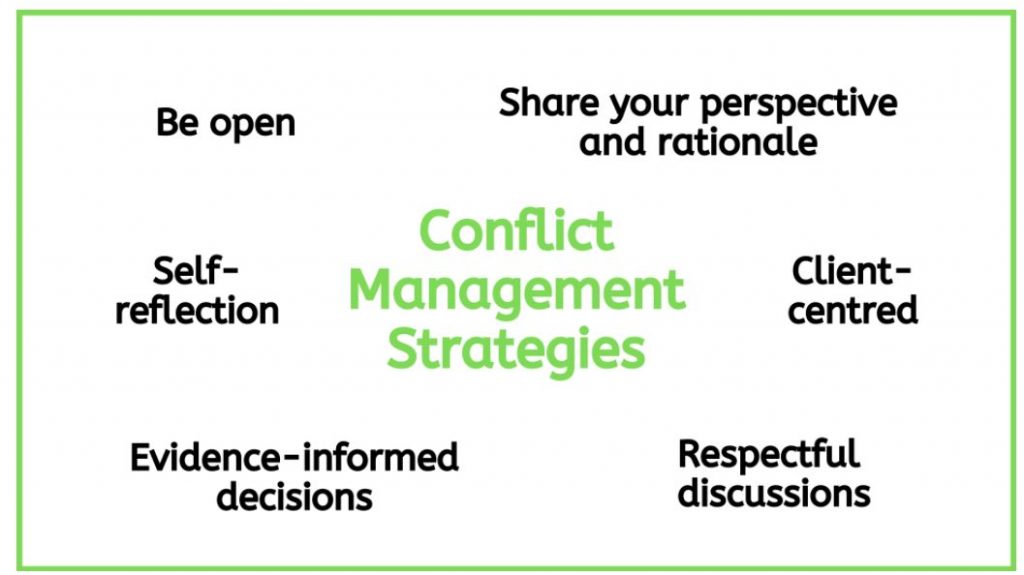
Behaviour examples of interprofessional conflict resolution and management include:
- Constructively address potential areas for conflict arising.
- Seek out solutions to support the resolution or to prevent conflicts.
- Support mutually agreed solutions in an appreciative manner
- Keep an open mind with differing views.
- Avoid blaming, and judging for optimal patient outcomes.
- Communicate with empathy
- Listen without interrupting
- Be available for communication opportunities
- Demonstrate support
- Use a client-centred approach to frame discussions.
- Use an evidence-informed approach to make decisions.
- Be open to hearing varying disciplinary perspectives.
- Engage in self-reflection.
- Engage in respectful discussions.
- Reflect on the perspectives of all team members.
- Share your perspective and rationale (Garmaise-Yee et al., 2020)
Figure 4.2 shows a graphical representation of conflict resolutions strategies
Collaborative Leadership
Collaborative leadership transpires when interprofessionals work together with patients, families, to provide as well as assess the care and the services provided. Each professional understands their role and accountability all with the goal of promoting healthy outcomes.
Behavioural examples of collaborative leadership include:
- Encourage participation in the coordination of planning care to achieve care goals.
- Designate accountability, recognize and address role overlap.
- Respectfully acknowledge appropriate expertise when needed in order to help guide patient/client needs.
- Advocate for patients, clients, and their families to facilitate the integration of care.
Collaborating with Interprofessional Teams to Support Patient Outcomes
Collaboration is especially significant in the healthcare environment to meet the increasingly complex demands of patients with multiple comorbidities. Collaboration pools resources to facilitate improvements in cost, availability, and quality of care (Tsakitzidis et al, 2016).
Scenario
Social media can be used to create virtual communities in health care environments. Many individuals also engage in social media outside of their professional practice. Typically, you do not have members of your organization on your personal social media platforms. Today, a friend of yours mentioned she saw a personal post by a member of your team which stated: “I have never met a more difficult group of HCA’s in our organization”
Reflecting on this. Consider these questions:
- What would you do?
- How can this be effectively handled? Should it be handled?
Check Your Understanding
Apply your knowledge from the chapter as you complete this review activity
Summary
In this chapter you have:
- Explored the elements involved in interprofessional communication.
- Reviewed the six domains of interprofessional competency framework as applied within the health care environment.
- Highlighted the behaviours to support conflict resolution when arises within the team and focused on areas of collaborative opportunities to improve care outcomes richly available through interprofessional teams.
Key Terms
Accountability: Accepting responsibility for one’s actions.
Adversarial: Involves two opposing sides.
Advocate: A person who will support and ask questions for those in a position that is unable to.
Appreciative: Showing gratitude.
Competency: Having acquired sufficient knowledge for their scope of practice.
Comorbidities: Two or more diseases present in a patient.
Constructively: In a way for a beneficial purpose.
Disciplines: Subject area or field of study.
Discrepancies: A variance or disagreement.
Domain: The area in which one’s scope of practice resides.
Encompassing: Everyone in the circle of care has complete knowledge of the situation at hand.
Harmonious: Everyone involved in reaching an agreement.
Interprofessional Communication: Communication taking place between health care professionals with clients/patients, families, and the community in general.
Interwoven: To mix or blend knowledge in relation to a person’s circle of care.
Migration (migrated): Moving from one location to another.
Misperceptions: Inaccurate or false information (Merriam Webster, n.d).
Multidisciplinary: Combining or involving more than one professional area of practice (Merriam Webster, n.d).
Preventive: Able to be avoided.
Rationale: Explanation of controlling principles, such as practice, belief, opinion, or phenomena (Merriam Webster, n.d).
Self-aware (self-awareness): A person being aware of their own individuality or personality.
Sensitive: Aware of the feelings and attitudes of those around you.
Systemic: Integral to a predominant economic, political practice, or social.
References
Garmaise-Yee. J., Hughes,M., Lapusm, J., & St-Amant, O. (2020). Introduction to communication in nursing. https://openlibrary.ecampusontario.ca/catalogue/item/?id=04e7dd2-8ba)-4be5-87c8-8cda40433a8
Toronto Academic Health Science Network & University of Toronto Centre for Interprofessional Education. (2017). Interprofessional care competency framework and team assessment toolkit. [PDF]. Ontario Dental Hygiene Association. https://odha.on.ca/wp-content/uploads/2017/05/IPC-Framework-and-Toolkit-Web.pdf [opens a PDF file]
Tsakitzidis, G., Timmermans, O., Callewaert, N., Verhoeven, V., Lopez-Hartmann, M., Truijen, S., Meulemans, H., & Van Royen, P. (2016) Outcome indicators on interprofessional collaboration interventions for elderly. International Journal of Integrated Care, 16(2): 5. doi: 10.5334/ijic.2017
Wagner. J. (2018). Leadership and influencing change in nursing. https://openlibrary.ecampusontario.ca/catalogue/item/?id=00e26b2d-3c99-4955-9173-fe6dee00a840
Image Descriptions
Figure 4.1: An image showing the six domains and goals of interprofessional communication in a circle detailing the connection of all six domains. [Return To Figure]
Figure 4.2: An image demonstrating strategies for managing conflict for interprofessional health care teams. [Return To Figure]
Assessing What You Already Know (Text-based Activity)
Question 1
Recall the recorded scenario at the start of the chapter with a new member joining a health centre and assess the communication by selecting one of the following statements:
- The exchange was appropriate and the HCA was friendly and supportive for the new team member.
- It did not start off ideal, however, the HCA was able to bring the conversation back to assist the new member.
- Nothing was resolved in this scenario.
Solution: Option 2 is correct. Both the players in this scenario did not immediately introduce themselves and this led to an initial misunderstanding of why the new team member was here.
Question 2
Consider this statement: Sharing relevant information and expertise is an important part of effective interprofessional health care teams, but it is not the only element which enable health care teams to work well. Select from the statement below, what may also help.
- Team members aim to be responsive to hearing the perspectives of other team members.
- Collaborative decisions can be made independently to reflect the specialized information.
- Team member must be willing to not be influenced by the information shared by other team members.
Solution: Option 1 is correct. Interprofessional teams bring a variety of insights and perspectives to support and address patient needs in a collaborative format. Continue exploring this chapter to learn more about interprofessional communication.
Question 3
Listen the following statement and choose true or false. Communication is not always the best process through with team roles are expressed and team goals are achieved.
- True.
- False.
Solution: The statement is false. There are a variety of important behavioral roles performed by different members of interprofessional health care teams. Communication is the process through with team roles are expressed and team goals are achieved. Return to Activity
Check your Understanding (Text-based Activity)
Question 1
Interprofessional teams will experience conflict. Conflict can encompass which of the following, select all which apply:
- Clear expectations.
- Lack of or incomplete information.
- Lack of shared team values.
- Communication disruptions due to misconceptions or stereotyping.
Solution: Options 2, 3 and 4 are correct. Clear expectations will avoid conflict not create it. When expectations are clearly defined it supports movement forward within the team.
Question 2
In a clinic or hospital setting you want a professional team that will advocate.
- True.
- False.
Solution: The statement is true. A professional team should support and advocate all of the members. Return to Activity
Communication taking place between health care professionals with clients/patients, families, and the community in general.
Combining or involving more than one professional area of practice (Merriam Webster, n.d).
subject area or field of study
able to be avoided
in a way for a beneficial purpose
showing gratitude
two or more diseases present in a patient
the act of being responsible for an action
Involves two opposing sides.
A person who will support and ask questions for those in a position that are unable to.
Having acquired sufficient knowledge for their scope of practice.
A variance or disagreement.
The area in which one's scope of practice resides.
Everyone in the circle of care has complete knowledge of the situation at hand.
Everyone involved in reaching an agreement.
To mix or blend knowledge in relation to a person's circle of care.
Moving from one location to another.
Inaccurate or false information (Merriam Webster, n.d).
Explanation of controlling principles, such as practice, belief, opinion, or phenomena (Merriam Webster, n.d).
A person being aware of their own individuality or personality.
Aware of the feelings and attitudes of those around you.
Integral to a predominant economic, political practice, or social.

