The Skeletal System
Bone Structure and Function
Your bones are stronger than reinforced concrete. Bone tissue is a composite of fibrous strands of collagen (a type of protein) that resemble the steel rebar in concrete and a hardened mineralized matrix that contains large amounts of calcium, just like concrete. But this is where the similarities end. Bone outperforms reinforced concrete by several orders of magnitude in compression and tension strength tests. Why? The microarchitecture of bone is complex and built to withstand extreme forces. Moreover, bone is a living tissue that is continuously breaking down and forming new bone to adapt to mechanical stresses.
Why Is the Skeletal System Important?
The human skeleton consists of 206 bones and other connective tissues called ligaments, tendons, and cartilage. Ligaments connect bones to other bones, tendons connect bones to muscles, and cartilage provides bones with more flexibility and acts as a cushion in the joints between bones. The skeleton’s many bones and connective tissues allow for multiple types of movement such as typing and running. The skeleton provides structural support and protection for all the other organ systems in the body. The skull, or cranium, is like a helmet and protects the eyes, ears, and brain. The ribs form a cage that surrounds and protects the lungs and heart. In addition to aiding in movement, protecting organs, and providing structural support, red and white blood cells and platelets are synthesized in bone marrow. Another vital function of bones is that they act as a storage depot for minerals such as calcium, phosphorous, and magnesium. Although bone tissue may look inactive at first glance, at the microscopic level you will find that bones are continuously breaking down and reforming. Bones also contain a complex network of canals, blood vessels, and nerves that allow for nutrient transport and communication with other organ systems.
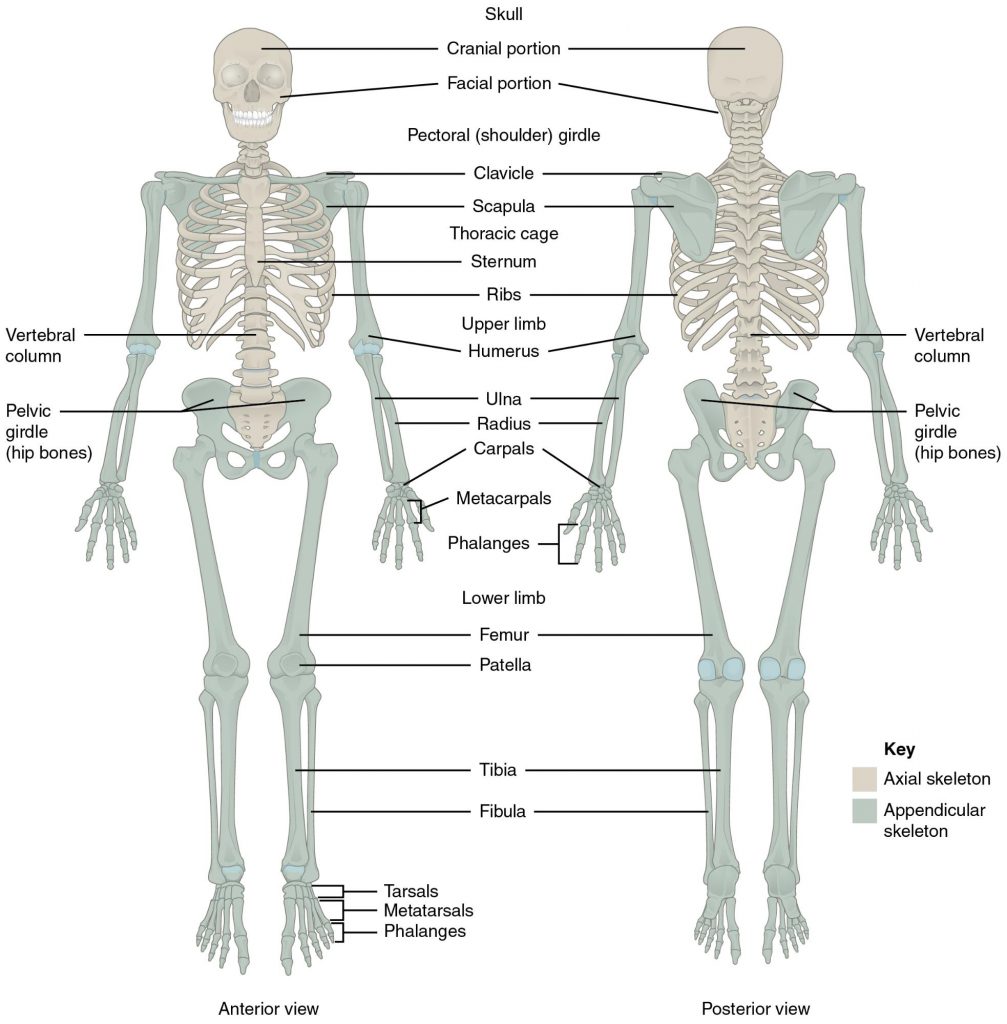
Figure 2.25 Human Skeletal Structure
Bone Anatomy and Structure
To optimize bone health through nutrition, it is important to understand bone anatomy. The skeleton is composed of two main parts, the axial and the appendicular parts. The axial skeleton consists of the skull, vertebral column, and rib cage, and is composed of eighty bones. The appendicular skeleton consists of the shoulder girdle, pelvic girdle, and upper and lower extremities, and is composed of 126 bones. Bones are also categorized by size and shape. There are four types of bone: long bones, short bones, flat bones, and irregular bones. The longest bone in your body is the femur (thigh bone), which extends from your hip to your knee. It is a long bone and functions to support your weight as you stand, walk, or run. Your wrist is composed of eight irregular-shaped bones, which allow for the intricate movements of your hands. Your twelve ribs on each side of your body are curved flat bones that protect your heart and lungs. Thus, the bones’ different sizes and shapes allow for their different functions.
Bones are composed of approximately 65 percent inorganic material known as mineralized matrix. This mineralized matrix consists of mostly crystallized hydroxyapatite. The bone’s hard crystal matrix of bone tissue gives it its rigid structure. The other 35 percent of bone is organic material, most of which is the fibrous protein collagen. The collagen fibers are networked throughout bone tissue and provide it with flexibility and strength. The bones’ inorganic and organic materials are structured into two different tissue types. There is spongy bone, also called trabecular or cancellous bone, and compact bone, also called cortical bone (Figure 2.26 “The Arrangement of Bone Tissues”). The two tissue types differ in their microarchitecture and porosity. Trabecular bone is 50 to 90 percent porous and appears as a lattice-like structure under the microscope. It is found at the ends of long bones, in the cores of vertebrae, and in the pelvis. Trabecular bone tissue makes up about 20 percent of the adult skeleton. The more dense cortical bone is about 10 percent porous and it looks like many concentric circles, similar to the rings in a tree trunk, sandwiched together (Figure 2.27 “Cortical (Compact) Bone”). Cortical bone tissue makes up approximately 80 percent of the adult skeleton. It surrounds all trabecular tissue and is the only bone tissue in the shafts of long bones.
Figure 2.26 The Arrangement of Bone Tissues
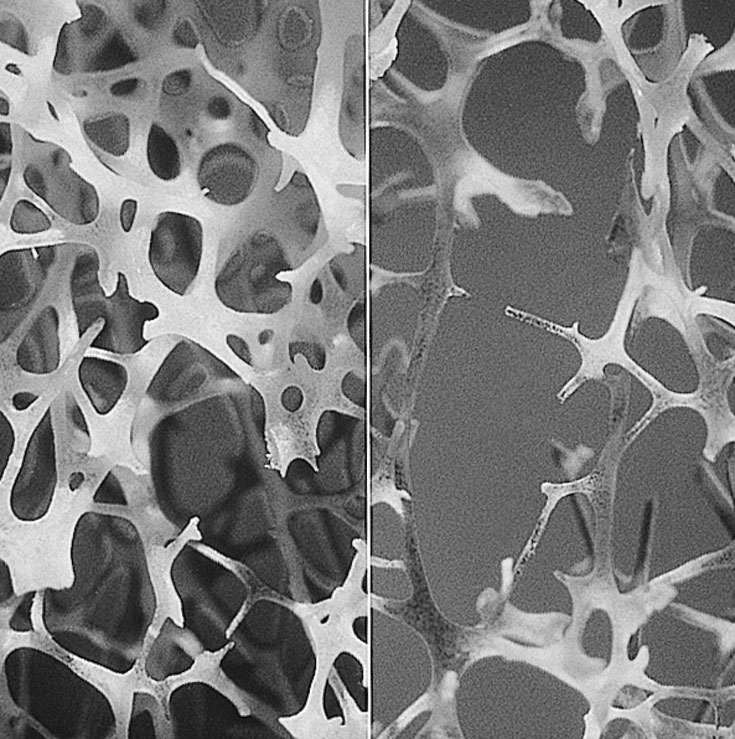
Figure 2.27 Cortical (Compact) Bone.
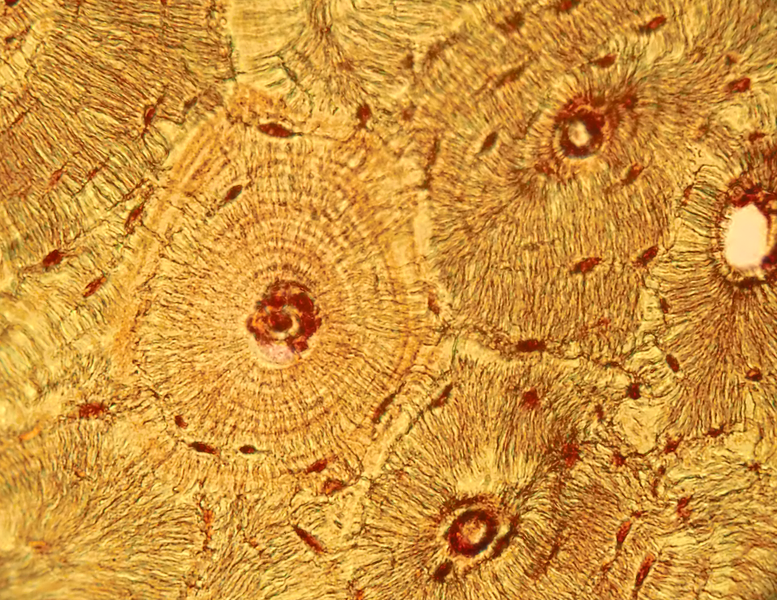
Bone tissue is arranged in an organized manner. A thin membrane, called the periosteum, surrounds the bone. It contains connective tissue with many blood vessels and nerves. Lying below the periosteum is the cortical bone. In some bones, the cortical bone surrounds the less-dense trabecular bone and the bone marrow lies within the trabecular bone, but not all bones contain trabecular tissue or marrow.
Bone Tissues and Cells, Modeling and Remodeling
Bone tissue contains many different cell types that constantly resize and reshape bones throughout growth and adulthood. Bone tissue cells include osteoprogenitor cells, osteoblasts, osteoclasts, and osteocytes. The osteoprogenitor cells are cells that have not matured yet. Once they are stimulated, some will become osteoblasts, the bone builders, and others will become osteoclasts, the cells that break bone down. Osteocytes are the most abundant cells in bone tissue. Osteocytes are star-shaped cells that are networked throughout the bone via their long cytoplasmic arms that allow for the exchange of nutrients and other factors from bones to the blood and lymph.
Bone Modeling and Remodeling
During infancy, childhood, and adolescence, bones are continuously growing and changing shape through two processes called growth (ossification) and modeling. In fact, in the first year of life, almost 100 percent of the bone tissue in the skeleton is replaced. In the process of modeling, bone tissue is dismantled at one site and built up at a different site. In adulthood, our bones stop growing and modeling, but continue to go through a process of bone remodeling. In the process of remodeling, bone tissue is degraded and built up at the same location. About 10 percent of bone tissue is remodeled each year in adults. Bones adapt their structure to the forces acting upon them, even in adulthood. This phenomenon is called Wolff’s law, which states that bones will develop a structure that is best able to resist the forces acting upon them. This is why exercising, especially when it involves weight-bearing activities, increases bone strength.
The first step in bone remodeling is osteocyte activation. Osteocytes detect changes in mechanical forces, calcium homeostasis, or hormone levels. In the second step, osteoclasts are recruited to the site of the degradation. Osteoclasts are large cells with a highly irregular ruffled membrane. These cells fuse tightly to the bone and secrete hydrogen ions, which acidify the local environment and dissolve the minerals in the bone tissue matrix. This process is called bone resorption and resembles pit excavation. Our bodies excavate pits in our bone tissue because bones act as storehouses for calcium and other minerals. Bones supply these minerals to other body tissues as the demand arises. Bone tissue also remodels when it breaks so that it can repair itself. Moreover, if you decide to train to run a marathon your bones will restructure themselves by remodeling to be better able to sustain the forces of their new function.
After a certain amount of bone is excavated, the osteoclasts begin to die and bone resorption stops. In the third step of bone remodeling, the site is prepared for building. In this stage, sugars and proteins accumulate along the bone’s surface, forming a cement line which acts to form a strong bond between the old bone and the new bone that will be made. These first three steps take approximately two to three weeks to complete. In the last step of bone remodeling, osteoblasts lay down new osteoid tissue that fills up the cavities that were excavated during the resorption process. Osteoid is bone matrix tissue that is composed of proteins such as collagen and is not mineralized yet. To make collagen, vitamin C is required. A symptom of vitamin C deficiency (known as scurvy) is bone pain, which is caused by diminished bone remodeling. After the osteoid tissue is built up, the bone tissue begins to mineralize. The last step of bone remodeling continues for months, and for a much longer time afterward the mineralized bone is continuously packed in a more dense fashion.
Thus, we can say that bone is a living tissue that continually adapts itself to mechanical stress through the process of remodeling. For bone tissue to remodel certain nutrients such as calcium, phosphorus, magnesium, fluoride, vitamin D, and vitamin K are required.
Bone Mineral Density Is an Indicator of Bone Health
Bone mineral density (BMD) is a measurement of the amount of calcified tissue in grams per centimeter squared of bone tissue. BMD can be thought of as the total amount of bone mass in a defined area. When BMD is high, bone strength will be great. Similar to measuring blood pressure to predict the risk of stroke, a BMD measurement can help predict the risk of bone fracture. The most common tool used to measure BMD is called dual energy X-ray absorptiometry (DEXA). During this procedure, a person lies on their back and a DEXA scanner passes two X-ray beams through their body. The amount of X-ray energy that passes through the bone is measured for both beams. The total amount of the X-ray energy that passes through a person varies depending on their bone thickness. Using this information and a defined area of bone, the amount of calcified tissue in grams per unit area (cm2) is calculated. Most often the DEXA scan focuses on measuring BMD in the hip and the spine. These measurements are then used as indicators of overall bone strength and health. DEXA is the cheapest and most accurate way to measure BMD. It also uses the lowest dose of radiation. Other methods of measuring BMD include quantitative computed tomography (QCT) and radiographic absorptiometry. People at risk for developing bone disease are advised to have a DEXA scan. We will discuss the many risk factors linked to an increased incidence of osteoporosis and the steps a person can take to prevent the disease from developing.

