Infancy
Diet and nutrition have a major impact on a child’s development from infancy into the adolescent years. A healthy diet not only affects growth, but also immunity, intellectual capabilities, and emotional well-being. One of the most important jobs of parenting is making sure that children receive an adequate amount of needed nutrients to provide a strong foundation for the rest of their lives.
The choice to breastfeed is one that all new mothers face. Support from family members, friends, employers, and others can greatly help with both the decision-making process during pregnancy and the practice of breastfeeding after the baby’s birth. In the United States, about 75 percent of babies start out being breastfed. Yet by the age of six months, when solid foods should begin to be introduced into a child’s diet along with breast milk, only 15 percent of infants in the United States were still breastfed exclusively, according to the Centers for Disease Control and Prevention (CDC).[1]
However, the approval and assistance of family members, friends, employers, health-care providers, and policymakers can make an enormous difference and provide the needed promotion and support for mothers who wish to breastfeed their children. Education about breastfeeding typically begins with health-care providers. During prenatal care and often soon after a woman has given birth, doctors, nurses, and other clinicians can explain the benefits of breastfeeding and describe the proper technique. Nearly all births in the United States and Canada occur in hospital settings, and hospital practices in labor, delivery, postpartum care, and discharge planning can inform and support women who want to breastfeed. Once a new mother has left the hospital for home, she needs access to a trained individual who can provide consistent information. International Board Certified Lactation Consultants (IBCLCs) are health-care professionals (often a registered nurse or registered dietitian) certified in breastfeeding management that work with new mothers to solve problems and educate families about the benefits of this practice. Research shows that breastfeeding rates are higher among women who had infants in hospitals that make IBCLCs available to new mothers, rather than those who gave birth in institutions without these professionals on staff.[2]
In addition, spouses, partners, and other family members can play critical roles in helping a pregnant woman make the decision to breastfeed and assisting with feeding after the baby is born. Employment can also factor into a woman’s decision to breastfeed or her ability to maintain the practice. Employed mothers have been less likely to initiate breastfeeding and tend to breastfeed for a shorter period of time than new mothers who are not employed or who have lengthy maternity leaves. In 2010 in the United States, the passage of the Affordable Care Act (ACA) called for employers to provide accommodations within the workplace for new mothers to pump breast milk. This law requires a private and clean space within the workplace, other than a restroom, along with adequate break time for a woman to express milk.[3]
Everyday Connection
In the Pacific, the state of Hawai‘i and and the territory of Guam are mandated to provide several accommodations within the workplace for new mothers. All employers are to required to allow breastfeeding mothers adequate break time to pump or nurse in location other than a bathroom. To learn more about Hawai‘i’s laws visit http://health.hawaii.gov/wic/files/2013/04/WorkplaceBreastfeeding_02_2014.pdf and for Guam’s laws visit http://www.guamcourts.org/CompilerofLaws/GCA/10gca/10gc092A.pdf.
Members of a community can also promote and support breastfeeding. New mothers can join peer counseling groups or turn to other women within their community who have previous experience with breastfeeding. In addition, community-based programs can provide education and support. The US Department of Agriculture’s Women, Infants, and Children program provides information on breastfeeding for low-income families. Launched in 2004, the Loving Support program combines peer counseling with breastfeeding promotion efforts to increase duration rates across the United States. La Leche League is an international program that provides mother-to-mother support, encouragement, and education about breastfeeding for women around the world. For more information on La Leche League, visit http://www.llli.org.
Although breastfeeding should be recommended and encouraged for almost all new mothers, it is important to remember that the decision to breastfeed is a personal choice and women should not be made to feel guilty if they cannot, or choose not, to breastfeed their infants. In some rare cases, a woman is unable to breastfeed or it is not in the baby’s best interest.
Nutritional choices that parents make, such as the decision to breastfeed or bottle-feed, not only affect early childhood development, but also a child’s health and wellness later in life. Therefore, it is imperative to promote and support the best practices for the well-being of infants and mothers alike.
Infancy (Birth to Age One)

A number of major physiological changes occur during infancy. The trunk of the body grows faster than the arms and legs, while the head becomes less prominent in comparison to the limbs. Organs and organ systems grow at a rapid rate. Also during this period, countless new synapses form to link brain neurons. Two soft spots on the baby’s skull, known as fontanels, allow the skull to accommodate rapid brain growth. The posterior fontanel closes first, by the age of eight weeks. The anterior fontanel closes about a year later, at eighteen months on average. Developmental milestones include sitting up without support, learning to walk, teething, and vocalizing among many, many others. All of these changes require adequate nutrition to ensure development at the appropriate rate.[4]
Healthy infants grow steadily, but not always at an even pace. For example, during the first year of life, height increases by 50 percent, while weight triples. Physicians and other health professionals can use growth charts to track a baby’s development process. Because infants cannot stand, length is used instead of height to determine the rate of a child’s growth. Other important developmental measurements include head circumference and weight. All of these must be tracked and compared against standard measurements for an infant’s age.
For infants and toddlers from birth to 24 months of age, the WHO growth charts are used to monitor growth. These standards represent optimal growth for children at this age and allow for tracking growth trends over time through percentile rankings. Growth charts may provide warnings that a child has a medical problem or is malnourished. Insufficient weight or height gain during infancy may indicate a condition known as failure-to-thrive (FTT), which is characterized by poor growth. FTT can happen at any age, but in infancy, it typically occurs after six months. Some causes include poverty, lack of enough food, feeding inappropriate foods, and excessive intake of fruit juice.
Figure 13.4 WHO Growth Chart For Boys From Birth To 24 Months

Nutritional Requirements
Requirements for macronutrients and micronutrients on a per-kilogram basis are higher during infancy than at any other stage in the human life cycle. These needs are affected by the rapid cell division that occurs during growth, which requires energy and protein, along with the nutrients that are involved in DNA synthesis. During this period, children are entirely dependent on their parents or other caregivers to meet these needs. For almost all infants six months or younger, breast milk is the best source to fulfill nutritional requirements. An infant may require feedings eight to twelve times a day or more in the beginning. After six months, infants can gradually begin to consume solid foods to help meet nutrient needs.
Energy and Macronutrients
Energy needs relative to size are much greater in an infant than an adult. A baby’s resting metabolic rate is two times that of an adult. The RDA to meet energy needs changes as an infant matures and puts on more weight. The IOM uses a set of equations to calculate the total energy expenditure and resulting energy needs. For example, the equation for the first three months of life is (89 x weight [kg] −100) + 175 kcal.
Based on these equations, the estimated energy requirement for infants from zero to six months of age is 472 to 645 kilocalories per day for boys and 438 to 593 kilocalories per day for girls. For infants ages six to twelve months, the estimated requirement is 645 to 844 kilocalories per day for boys and 593 to 768 kilocalories per day for girls. From the age one to age two, the estimated requirement rises to 844–1,050 kilocalories per day for boys and 768–997 kilocalories per day for girls.[5] How often an infant wants to eat will also change over time due to growth spurts, which typically occur at about two weeks and six weeks of age, and again at about three months and six months of age.
The dietary recommendations for infants are based on the nutritional content of human breast milk. Carbohydrates make up about 45 to 65 percent of the caloric content in breast milk, which amounts to a RDA of about 130 grams. Almost all of the carbohydrate in human milk is lactose, which infants digest and tolerate well. In fact, lactose intolerance is practically nonexistent in infants. Protein makes up about 5 to 20 percent of the caloric content of breast milk, which amounts to 13 grams per day. Infants have a high need for protein to support growth and development, though excess protein (which is only a concern with bottle-feeding) can cause dehydration, diarrhea, fever, and acidosis in premature infants. About 30 to 40 percent of the caloric content in breast milk is made up of fat. A high-fat diet is necessary to encourage the development of neural pathways in the brain and other parts of the body. However, saturated fats and trans fatty acids inhibit this growth. Infants who are over the age of six months, which means they are no longer exclusively breastfed, should not consume foods that are high in these types of fats.
Micronutrients
Almost all of the nutrients that infants require can be met if they consume an adequate amount of breast milk. There are a few exceptions, though. Human milk is low in vitamin D, which is needed for calcium absorption and building bone, among other things. Therefore, breastfed children often need to take a vitamin D supplement in the form of drops. Infants at the highest risk for vitamin D deficiency are those with darker skin and no exposure to sunlight. Breast milk is also low in vitamin K, which is required for blood clotting, and deficits could lead to bleeding or hemorrhagic disease. Babies are born with limited vitamin K, so supplementation may be needed initially and some states require a vitamin K injection after birth. Also, breast milk is not high in iron, but the iron in breast milk is well absorbed by infants. After four to six months, however, an infant needs an additional source of iron other than breast milk.
Fluids
Infants have a high need for fluids, 1.5 milliliters per kilocalorie consumed compared to 1.0 milliliters per kilocalorie consumed for adults. This is because children have larger body surface area per unit of body weight and a reduced capacity for perspiration. Therefore, they are at greater risk of dehydration. However, parents or other caregivers can meet an infant’s fluid needs with breast milk or formula. As solids are introduced, parents must make sure that young children continue to drink fluids throughout the day.
Breastfeeding
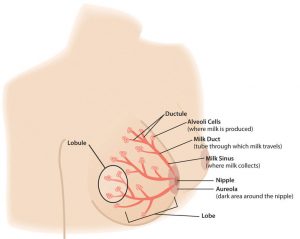
The alveoli cells produce milk. To secrete it, they contract and push milk into the ductules and the milk sinus, which collects the milk. When a nursing infant’s gums press on the areola and nipple, the sinuses squeeze the milk into the baby’s mouth. The nipple tissue becomes firmer with stimulation, which makes it more flexible and easier for the baby to grasp in the mouth. After the birth of the baby, nutritional needs must be met to ensure that an infant not only survives, but thrives from infancy into childhood. Breastfeeding provides the fuel a newborn needs for rapid growth and development. As a result, the WHO recommends that breastfeeding be done exclusively for the first six months of an infant’s life. Exclusive breastfeeding is one of the best ways a mother can support the growth and protect the health of her infant child. Breast milk contains all of the nutrients that a newborn requires and gives a child the best start to a healthy life. Many women want to breastfeed their babies. Unfortunately, a mother’s intention alone may not be enough to make this practice possible. Around the world, less than 40 percent of infants under the age of six months are breastfed exclusively.[6]
New mothers must also pay careful consideration to their own nutritional requirements to help their bodies recover in the wake of the pregnancy. This is particularly true for women who breastfeed their babies, which calls for an increased need in certain nutrients.
Lactation
Lactation is the process that makes breastfeeding possible, and is the synthesis and secretion of breast milk. Early in a woman’s pregnancy, her mammary glands begin to prepare for milk production. Hormones play a major role in this, particularly during the second and third trimesters. At that point, levels of the hormone prolactin increase to stimulate the growth of the milk duct system, which initiates and maintains milk production. Levels of the hormone oxytocin also rise to promote the release of breast milk when the infant suckles, which is known as the milk ejection reflex. However, levels of the hormone progesterone need to decrease for successful milk production, because progesterone inhibits milk secretion. Shortly after birth, the expulsion of the placenta triggers progesterone levels to fall, which activates lactation.[7]
New mothers need to adjust their caloric and fluid intake to make breastfeeding possible. The RDA is 330 additional calories during the first six months of lactation and 400 additional calories during the second six months of lactation. The energy needed to support breastfeeding comes from both increased intake and from stored fat. For example, during the first six months after her baby is born, the daily caloric cost for a lactating mother is 500 calories, with 330 calories derived from increased intake and 170 calories derived from maternal fat stores. This helps explain why breastfeeding may promote weight loss in new mothers. Lactating women should also drink 3.1 liters of liquids per day (about 13 cups) to maintain milk production, according to the IOM. As is the case during pregnancy, the RDA of nearly all vitamins and minerals increases for women who are breastfeeding their babies. The following table compares the recommended vitamins and minerals for lactating women to the levels for nonpregnant and pregnant women from Table 13.3 “Recommended Nutrient Intakes during Pregnancy”.
Table 13.3 Recommended Nutrient Intakes during Lactation
| Nutrient | Nonpregnant Women | Pregnant Women | Lactating Women |
| Vitamin A (mcg) | 700.0 | 770.0 | 1,300.0 |
| Vitamin B6 (mg) | 1.5 | 1.9 | 2.0 |
| Vitamin B12 (mcg) | 2.4 | 2.6 | 2.8 |
| Vitamin C (mg) | 75.0 | 85.0 | 120.0 |
| Vitamin D (mcg) | 5.0 | 5.0 | 5.0 |
| Vitamin E (mg) | 15.0 | 15.0 | 19.0 |
| Calcium (mg) | 1,000.0 | 1,000.0 | 1,000.0 |
| Folate (mcg) | 400.0 | 600.0 | 500.0 |
| Iron (mg) | 18.0 | 27.0 | 9.0 |
| Magnesium (mg) | 320.0 | 360.0 | 310.0 |
| Niacin (B3) (mg) | 14.0 | 18.0 | 17.0 |
| Phosphorus | 700.0 | 700.0 | 700.0 |
| Riboflavin (B2) (mg) | 1.1 | 1.4 | 1.6 |
| Thiamine (B1) (mg) | 1.1 | 1.4 | 1.4 |
| Zinc (mg) | 8.0 | 11.0 | 12.0 |
Source: Institute of Medicine. 2006. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press. https://doi.org/10.17226/11537. Accessed December 10, 2017.
Calcium requirements do not change during breastfeeding because of more efficient absorption, which is the case during pregnancy, too. However, the reasons for this differ. During pregnancy, there is enhanced absorption within the gastrointestinal tract. During lactation, there is enhanced retention by the kidneys. The RDA for phosphorus, fluoride, and molybdenum also remains the same.
Components of Breastmilk
Human breast milk not only provides adequate nutrition for infants, it also helps to protect newborns from disease. In addition, breast milk is rich in cholesterol, which is needed for brain development. It is helpful to know the different types and components of breastmilk, along with the nutrients they provide to enable an infant survive and thrive. Colostrum is produced immediately after birth, prior to the start of milk production, and lasts for several days after the arrival of the baby. Colostrum is thicker than breast milk, and is yellowish or creamy in color. This protein-rich liquid fulfills an infant’s nutrient needs during those early days. Although low in volume, colostrum is packed with concentrated nutrition for newborns. This special milk is high in fat-soluble vitamins, minerals, and immunoglobulins (antibodies) that pass from the mother to the baby. Immunoglobulins provide passive immunity for the newborn and protect the baby from bacterial and viral diseases.[8]
Two to four days after birth, colostrum is replaced by transitional milk. Transitional milk is a creamy liquid that lasts for approximately two weeks and includes high levels of fat, lactose, and water-soluble vitamins. It also contains more calories than colostrum. After a new mother begins to produce transitional milk, she typically notices a change in the volume and type of liquid secreted and an increase in the weight and size of her breasts.[9]
Mature milk is the final fluid that a new mother produces. In most women, it begins to secrete at the end of the second week postpartum. There are two types of mature milk that appear during a feeding. Foremilk occurs at the beginning and includes water, vitamins, and protein. Hind-milk occurs after the initial release of milk and contains higher levels of fat, which is necessary for weight gain. Combined, these two types of milk ensure that a baby receives adequate nutrients to grow and develop properly.[10]
About 90 percent of mature milk is water, which helps an infant remain hydrated. The other 10 percent contains carbohydrates, proteins, and fats, which support energy and growth. Similar to cow’s milk, the main carbohydrate of mature breast milk is lactose. Breast milk contains vital fatty acids, such as docosahexaenoic acid (DHA) and arachidonic acid (ARA). In terms of protein, breast milk contains more whey than casein (which is the reverse of cow’s milk). Whey is much easier for infants to digest than casein. Complete protein, which means all of the essential amino acids, is also present in breast milk. Complete protein includes lactoferrin, an iron-gathering compound that helps to absorb iron into an infant’s bloodstream.
In addition, breast milk provides adequate vitamins and minerals. Although absolute amounts of some micronutrients are low, they are more efficiently absorbed by infants. Other essential components include digestive enzymes that help a baby digest the breast milk. Human milk also provides the hormones and growth factors that help a newborn to develop.
Diet and Milk Quality
A mother’s diet can have a major impact on milk production and quality. As during pregnancy, lactating mothers should avoid illegal substances and cigarettes. Some legal drugs and herbal products can be harmful as well, so it is helpful to discuss them with a health-care provider. Some mothers may need to avoid certain things, such as spicy foods, that can produce gas in sensitive infants. Lactating women can drink alcohol, though they must avoid breastfeeding until the alcohol has completely cleared from their milk. Typically, this takes two to three hours for 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor, depending on a woman’s body weight.[11] Precautions are necessary because exposure to alcohol can disrupt an infant’s sleep schedule.
Benefits of Breastfeeding
Breastfeeding has a number of benefits, both for the mother and for the child. Breast milk contains immunoglobulins, enzymes, immune factors, and white blood cells. As a result, breastfeeding boosts the baby’s immune system and lowers the incidence of diarrhea, along with respiratory diseases, gastrointestinal problems, and ear infections. Breastfed babies also are less likely to develop asthma and allergies, and breastfeeding lowers the risk of sudden infant death syndrome. In addition, human milk encourages the growth of healthy bacteria in an infant’s intestinal tract. All of these benefits remain in place after an infant has been weaned from breast milk. Some studies suggest other possible long-term effects. For example, breast milk may improve an infant’s intelligence and protect against Type 1 diabetes and obesity, although research is ongoing in these areas.[12]
Breastfeeding has a number of other important benefits. It is easier for babies to digest breast milk than bottle formula, which contains proteins made from cow’s milk that require an adjustment period for infant digestive systems. Breastfed infants are sick less often than bottle-fed infants. Breastfeeding is more sustainable and results in less plastic waste and other trash. Breastfeeding can also save families money because it does not incur the same cost as purchasing formula. Other benefits include that breast milk is always ready. It does not have to be mixed, heated, or prepared. Also, breast milk is sterile and is always at the right temperature.
In addition, the skin-to-skin contact of breastfeeding promotes a close bond between mother and baby, which is an important emotional and psychological benefit. The practice also provides health benefits for the mother. Breastfeeding helps a woman’s bones stay strong, which protects against fractures later in life. Studies have also shown that breastfeeding reduces the risk of breast and ovarian cancers.[13]
The Baby-Friendly Hospital Initiative
In 1991, the WHO and UNICEF launched the Baby-Friendly Hospital Initiative (BFHI), which works to ensure that all maternities, including hospitals and free-standing facilities, become centers of breastfeeding support. A maternity can be denoted as “baby-friendly” when it does not accept substitutes to human breast milk and has implemented ten steps to support breastfeeding. These steps include having a written policy on breastfeeding communicated to health-care staff on a routine basis, informing all new mothers about the benefits and management of breastfeeding, showing new mothers how to breastfeed their infants, and how to maintain lactation, and giving newborns no food or drink other than breast milk, unless medically indicated. Since the BFHI began, more than fifteen thousand facilities in 134 countries, from Benin to Bangladesh, have been deemed “baby friendly.” As a result, more mothers are breastfeeding their newborns and infant health has improved, in both the developed world and in developing nations.[14]
Barriers to Breastfeeding
Although breast milk is ideal for almost all infants, there are some challenges that nursing mothers may face when starting and continuing to breastfeed their infants. These obstacles include painful engorgement or fullness in the breasts, sore and tender nipples, lack of comfort or confidence in public, and lack of accommodation to breastfeed or express milk in the workplace.
One of the first challenges nursing mothers face is learning the correct technique. It may take a little time for a new mother to help her baby properly latch on to her nipples. Improper latching can result in inadequate intake, which could slow growth and development. However, International Board Certified Lactation Consultants (IBCLCs), OB nurses, and registered dietitians are all trained to help new mothers learn the proper technique. Education, the length of maternity leave, and laws to protect public breastfeeding, among other measures, can all help to facilitate breastfeeding for many lactating women and their newborns.
Contraindications to Breastfeeding
Although there are numerous benefits to breastfeeding, in some cases there are also risks that must be considered. In the developed world, a new mother with HIV should not breastfeed, because the infection can be transmitted through breast milk. These women typically have access to bottle formula that is safe, and can be used as a replacement for breast milk. However, in developing nations where HIV infection rates are high and acceptable infant formula can be difficult to come by, many newborns would be deprived of the nutrients they need to develop and grow. Also, inappropriate or contaminated bottle formulas cause 1.5 million infant deaths each year. As a result, the WHO recommends that women infected with HIV in the developing world should nurse their infants while taking antiretroviral medications to lower the risk of transmission.[15]
Breastfeeding also is not recommended for women undergoing radiation or chemotherapy treatment for cancer. Additionally, if an infant is diagnosed with galactosemia, meaning an inability to process the simple sugar galactose, the child must be on a galactose-free diet, which excludes breast milk. This genetic disorder is a very rare condition, however, and only affects 1 in thirty- to sixty thousand newborns.[16] When breastfeeding is contraindicated for any reason, feeding a baby formula enables parents and caregivers to meet their newborn’s nutritional needs.
Bottle-Feeding
Most women can and should breastfeed when given sufficient education and support. However, as discussed, a small percentage of women are unable to breastfeed their infants, while others choose not to. For parents who choose to bottle-feed, infant formula provides a balance of nutrients. However, not all formulas are the same and there are important considerations that parents and caregivers must weigh. Standard formulas use cow’s milk as a base. They have 20 calories per fluid ounce, similar to breast milk, with vitamins and minerals added. Soy-based formulas are usually given to infants who develop diarrhea, constipation, vomiting, colic, or abdominal pain, or to infants with a cow’s milk protein allergy. Hypoallergenic protein hydrolysate formulas are usually given to infants who are allergic to cow’s milk and soy protein. This type of formula uses hydrolyzed protein, meaning that the protein is broken down into amino acids and small peptides, which makes it easier to digest. Preterm infant formulas are given to low birth weight infants, if breast milk is unavailable. Preterm infant formulas have 24 calories per fluid ounce and are given until the infant reaches a desired weight.
Infant formula comes in three basic types:
- Powder that requires mixing with water. This is the least expensive type of formula.
- Concentrates, which are liquids that must be diluted with water. This type is slightly more expensive.
- Ready-to-use liquids that can be poured directly into bottles. This is the most expensive type of formula. However, it requires the least amount of preparation. Ready-to-use formulas are also convenient for traveling.
Most babies need about 2.5 ounces of formula per pound of body weight each day. Therefore, the average infant should consume about 24 fluid ounces of breastmilk or formula per day. When preparing formula, parents and caregivers should carefully follow the safety guidelines, since an infant has an immature immune system. All equipment used in formula preparation should be sterilized. Prepared, unused formula should be refrigerated to prevent bacterial growth. Parents should make sure not to use contaminated water to mix formula in order to prevent foodborne illnesses. Follow the instructions for powdered and concentrated formula carefully—formula that is overly diluted would not provide adequate calories and protein, while overly concentrated formula provides too much protein and too little water which can impair kidney function.
It is important to note again that both the American Academy of Pediatrics and the WHO state that breast milk is far superior to infant formula. This table compares the advantages of giving a child breast milk to the disadvantages of using bottle formula.
Table 13.4 Breast Milk versus Bottle Formula
| Breast Milk | Bottle Formula |
| Antibodies and lactoferrin in breast milk protect infants. | Formula does not contain immunoprotective factors. |
| The iron in breast milk is absorbed more easily. | Formula contains more iron than breast milk, but it is not absorbed as easily. |
| The feces that babies produce do not smell because breastfed infants have different bacteria in the gut. | The feces that bottle-fed infants produce tends to have a foul-smelling odor. |
| Breast milk is always available and is always at the correct temperature. | Formula must be prepared, refrigerated for storage, and warmed before it is given to an infant. |
| Breastfed infants are less likely to have constipation. | Bottle-fed infants are more likely to have constipation. |
| Breastfeeding ostensibly is free, though purchasing a pump and bottles to express milk does require some expense. | Formula must be purchased and is expensive. |
| Breast milk contains the fatty acids DHA and ARA, which are vital for brain and vision development. | Some formulas contain DHA and ALA. |
Source: Breastfeeding versus Bottle Feeding. American Pregnancy Association. http://www.americanpregnancy.org/firstyearoflife/breastfeedingandbottle.html. Updated May 16, 2017. Accessed December 5, 2017.
Introducing Solid Foods
Infants should be breastfed or bottle-fed exclusively for the first six months of life according to the WHO. (The American Academy of Pediatrics recommends breast milk or bottle formula exclusively for at least the first four months, but ideally for six months.) Infants should not consume solid foods prior to six months because solids do not contain the right nutrient mix that infants need. Also, eating solids may mean drinking less breast milk or bottle formula. If that occurs, an infant may not consume the right quantities of various nutrients. If parents try to feed an infant who is too young or is not ready, their tongue will push the food out, which is called an extrusion reflex. After six months, the suck-swallow reflexes are not as strong, and infants can hold up their heads and move them around, both of which make eating solid foods more feasible.
Solid baby foods can be bought commercially or prepared from regular food using a food processor, blender, food mill, or grinder at home. By nine months to a year, infants are able to chew soft foods and can eat solids that are well chopped or mashed. Infants who are fed solid foods too soon are susceptible to developing food allergies. Therefore, as parents and caregivers introduce solids, they should feed their child only one new food at a time, to help identify allergic responses or food intolerances. An iron supplement is also recommended at this time.
Everyday Connection
Different cultures have specific food customs. In ancient Hawai‘i, poi (pounded taro) was a staple food in the diet and is still popular today due to it’s nutrient-dense structure.

Poi is high in easily digestible calories, a good source of calcium and iron along with a number of other essential vitamins and minerals. Poi also has many gastrointestinal tract health benefits due to its fiber and probiotic content. With it’s viscous texture, poi is an excellent first food for infants to consume.

Table 13.5 Appropriate Foods for Complementary Feeding
| WHAT FOODS TO GIVE AND WHY | HOW TO GIVE THE FOODS |
BREAST MILK: continues to provide energy and high quality nutrients up to 23 monthsSTAPLE FOODS: provide energy, some protein (cereals only) and vitamins
ANIMAL-SOURCE FOODS: provide high quality protein, haem iron, zinc and vitamins
MILK PRODUCTS: provide protein, energy, most vitamins (especially vitamin A and folate), calcium
GREEN LEAFY AND ORANGE-COLOURED VEGETABLES: provide vitamins A, C, folate
PULSES: provide protein (of medium quality), energy, iron (not well absorbed)
OILS AND FATS: provide energy and essential fatty acids
SEEDS: provide energy
|
Infants 6–11 months
|
Children 12–23 months
|
| REMINDER: |
Foods rich in iron
Foods rich in Vitamin A
Foods rich in zinc
Foods rich in calcium
Foods rich in Vitamin C
|
Source: Table 3.5 Appropriate Foods For Complementary Foods. National Institute of Health. https://www.ncbi.nlm.nih.gov/books/NBK148957/table/session3.t3/?report=objectonly. Accessed February 19, 2018.
Learning to Self-Feed
With the introduction of solid foods, young children begin to learn how to handle food and how to feed themselves. At six to seven months, infants can use their whole hand to pick up items (this is known as the palmer grasp). They can lift larger items, but picking up smaller pieces of food is difficult. At eight months, a child might be able to use a pincer grasp, which uses fingers to pick up objects. After the age of one, children slowly begin to use utensils to handle their food. Unbreakable dishes and cups are essential, since very young children may play with them or throw them when they become bored with their food.
Food Allergies
Food allergies impact four to six percent of young children in America. Common food allergens include peanuts, eggs, shellfish, wheat, and cow’s milk. However, lactating women should not make any changes to their diets. Research shows that nursing mothers who attempt to ward off allergies in their infants by eliminating certain foods may do more harm than good. According to the American Academy of Allergy, Asthma, and Immunology, mothers who avoided certain dairy products showed decreased levels in their breast milk of an immunoglobulin specific to cow’s milk. This antibody is thought to protect against the development of allergies in children. Even when an infant is at higher risk for food allergies, there is no evidence that alterations in a mother’s diet make a difference. And, it is possible that continuing breastfeeding when introducing solid foods in the infant diet may be preventative. There is currently no scientific evidence indicating that delayed (after six months of age) or early (before four months of age) introduction of solid foods is preventative. However, there is evidence that introduction of solid foods after 17 weeks of age is associated with decreased risk of developing food allergies.[17][18]
Early Childhood Caries
Primary teeth are at risk for a disorder known as early childhood caries from breast milk, formula, juice, or other drinks fed through a bottle. Liquids can build up in a baby’s mouth, and the natural or added sugars lead to decay. Early childhood caries is caused not only by the kinds of liquids given to an infant, but also by the frequency and length of time that fluids are given. Giving a child a bottle of juice or other sweet liquids several times each day, or letting a baby suck on a bottle longer than a mealtime, either when awake or asleep, can also cause early childhood caries. In addition, this practice affects the development and position of the teeth and the jaw. The risk of early childhood caries continues into the toddler years as children begin to consume more foods with a high sugar content. Therefore, parents should avoid giving their children sugary snacks and beverages.
Newborn Jaundice
Newborn jaundice is another potential problem during infancy. This condition can occur within a few days of birth and is characterized by yellowed skin or yellowing in the whites of the eyes, which can be harder to detect in dark-skinned babies. Jaundice typically appears on the face first, followed by the chest, abdomen, arms, and legs. This disorder is caused by elevated levels of bilirubin in a baby’s bloodstream. Bilirubin is a substance created by the breakdown of red blood cells and is removed by the liver. Jaundice develops when a newborn’s liver does not efficiently remove bilirubin from the blood. There are several types of jaundice associated with newborns:
- Physiologic jaundice. The most common type of newborn jaundice and can affect up to 60 percent of full-term babies in the first week of life.
- Breast-milk jaundice. The name for a condition that persists after physiologic jaundice subsides in otherwise healthy babies and can last for three to twelve weeks after birth. Breast-milk jaundice tends to be genetic and there is no known cause, although it may be linked to a substance in the breast milk that blocks the breakdown of bilirubin. However, that does not mean breastfeeding should be stopped. As long as bilirubin levels are monitored, the disorder rarely leads to serious complications.
- Breastfeeding jaundice. Occurs when an infant does not get enough milk. This may happen because a newborn does not get a good start breastfeeding, does not latch on to the mother’s breast properly, or is given other substances that interfere with breastfeeding (such as juice). Treatment includes increased feedings, with help from a lactation consultant to ensure that the baby takes in adequate amounts.
Newborn jaundice is more common in a breastfed baby and tends to last a bit longer. If jaundice is suspected, a pediatrician will run blood tests to measure the amount of bilirubin in an infant’s blood. Treatment often involves increasing the number of feedings to increase bowel movements, which helps to excrete bilirubin. Within a few weeks, as the baby begins to mature and red blood cell levels diminish, jaundice typically subsides with no lingering effects.[19]
- Breastfeeding: Promotion and Support. Centers for Disease Control and Prevention. http://www.cdc.gov/breastfeeding/promotion/index.htm. Updated August 4, 2017. Accessed November 29, 2017. ↵
- Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding. US Department of Health and Human Services, Office of the Surgeon General. http://www.surgeongeneral.gov/topics/breastfeeding/executivesummary.pdf. Updated August 12, 2014. Accessed December 2, 2017. ↵
- Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding. US Department of Health and Human Services, Office of the Surgeon General. http://www.surgeongeneral.gov/topics/breastfeeding/executivesummary.pdf. Updated August 12, 2014. Accessed DEcember 8, 2017. ↵
- McMillan B. Illustrated Atlas of the Human Body. Sydney, Australia: Weldon Owen. 2008, 248. ↵
- Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids.Food and Nutrition Board, Institute of Medicine. Washington, D.C.: The National Academies Press. 2005, 169–70. ↵
- 10 Facts on Breastfeeding. World Health Organization. http://www.who.int/features/factfiles/breastfeeding/en/. Updated August 2017. Accessed December 2, 2017. ↵
- King J. Contraception and Lactation: Physiology of Lactation. Journal of Midwifery and Women’s Health. 2007; 52(6), 614–20. ↵
- Breastfeeding: Overview. American Pregnancy Association. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm.Updated May 16, 2017. Accessed November 29, 2017. ↵
- Breastfeeding: Overview. American Pregnancy Association. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm. Updated May 16, 2017. Accessed November 29, 2017. ↵
- Breastfeeding: Overview. American Pregnancy Association. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm. Updated May 16, 2017. Accessed November 29, 2017. ↵
- Harms R. Breast-Feeding and Alcohol: Is It Okay to Drink?. Mayo Foundation for Medical Education and Research. Accessed February 21, 2012. http://www.mayoclinic.com/health/breast-feeding-and-alcohol/AN02131. Updated March 11, 2016. Accessed November 28, 2017. ↵
- Breastfeeding Benefits Your Baby’s Immune System. Healthy Children.org. American Academy of Pediatrics. http://www.healthychildren.org/English/ages-stages/baby/breastfeeding/pages/Breastfeeding-Benefits-Your-Baby%27s-Immune-System.aspx. Updated January 1, 2006. Accessed November 28, 2017. ↵
- Reproductive History and Breast Cancer Risk. National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/Risk/reproductive-history. Updated November 9, 2016. Accessed November 28, 2017. ↵
- The Baby-Friendly Hospital Initiative. United Nations Children’s Fund. http://www.unicef.org/programme/breastfeeding/baby.htm. Updated December 18, 2017. Accessed December 18, 2017. ↵
- Infant and Young Child Feeding. World Health Organization. http://www.who.int/mediacentre/factsheets/fs342/en/index.html. Updated July 2017. Accessed December 5, 2017. ↵
- Galactosemia. Genetics Home Reference, a service of the US National Library of Medicine. http://ghr.nlm.nih.gov/condition/galactosemia. Published December 12, 2017. Accessed December 14, 2017. ↵
- Alvisi P, Brusa S, Alboresi S. Recommendations on Complementary Feeding for Healthy, Full-term Infants. Italian Journal of Pediatrics. 2015; 41(36) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464122/. Accessed November 22, 2017. ↵
- Gever J. Nursing Mom’s Diet No Guard Against Baby Allergies. Medpage Today. Everyday Health, Inc. March 7, 2012. http://www.medpagetoday.com/MeetingCoverage/AAAAIMeeting/31527. Accessed November 22, 2017. ↵
- Breastfeeding and Jaundice. American Pregnancy Association. http://www.americanpregnancy.org/firstyearoflife/breastfeedingandjaundice.htm. Updated August 2015. Accessed December 5, 2017. ↵

