12 Midwives Using Research: Evidence-based Practice & Evidence-Informed Midwifery
Vicki van Wagner, RM, PhD
The chapter will review definitions of evidence-based practice (EBP) and, specifically, will explore how evidence-informed midwifery defines itself. The intertwined histories of midwifery and EBP are explored to show the meaning and importance of EBP to midwifery practice and policy.
12. 1 Introduction
It might seem obvious to the current generation of midwives and other health care providers that practice should be informed by evidence as this is now an accepted approach to health care. When the concept of evidence-based medicine (EBM) was introduced in the early 1990s however, this idea was harkened as a ‘paradigm shift’ (1, p.1) and even a “revolutionary movement.” (2) The concept of EBM evolved to EBP to be inclusive of not only other health care professions but also other professional disciplines. The need to use evidence as the basis for decision-making has become an expected, if challenging, approach to practice and policy-making in all areas.
Midwifery, particularly midwifery in Canada, has a unique relationship to EBP, and a history that provides insights into both our profession and the ongoing evolution of the application of evidence to maternity care. (3) EBP offers much to midwives and health care practice, but it is important to understand the potential limitations and unexpected effects of a naïve application of EBP. For example, in Ontario, Canada midwives have generated an integrated approach to EBP through midwifery clinical practice guidelines (CPGs) and other evidence-based resources for midwives and clients that combine a rigorous look at evidence with a values-based approach to the application of evidence. (4)
12.2 What is EBP?
EBP is commonly defined as a commitment to base health care on the best available scientific evidence. The term EBM was first used in an article in the Journal of the American Medical Association (JAMA) in 1992, and it had evolved from previous labels including, research-based practice. (5) EBP is used interchangeably with evidence-based health care and has generated labels specific to particular health professions such as evidence-based midwifery, nursing, physiotherapy. The concept is also now applied outside healthcare professions, such as evidence-based social work and teaching; and evidence-based policy and evidence-based management.
EBP uses well-defined criteria to evaluate the quality of clinical research, creating a hierarchy of evidence (Table 12-1). The most scientific and therefore highest quality research is generally considered to be the randomized controlled trial (RCT). RCTs may be blinded, such that study participants and/or health care providers and/or those evaluating the results do not know which participants received which intervention. Blinded RCTs are frequently referred to as single-, double- or triple-blind, despite these terms having been found to be used and interpreted inconsistently. (6,7) The present guidelines state that reports of blinded RCT should include explanation of who was blinded after assignment to interventions and how. (8)
| Table 12-1. Hierarchies of Evidence, after Sacket et. al (9). |
|
In clinical research, such as maternity care research, blinding of the participants and health care providers is often not possible as both the care provider and patient know the nature of the treatment being applied or not applied, such as would be the case if the intervention involves, e.g. physical therapy. However, participants should still, if at all possible, be randomly assigned to their groups and it is ‘still desirable and often possible to blind the assessor or obtain an objective source of data for evaluation of outcomes.’ (10) In maternity care, both childbearing clients and care providers involved in trials are commonly aware of the treatments, but patients are randomized in allocation to their group to either receive or not receive the treatment. The randomization process that distinguishes the evidence from RCTs from cohort or case-control studies and outcomes research, as it reduces systematic bias. What is now the Canadian Task Force on Preventive Health Care (CTFPHC) developed a system for grading the level and quality of research evidence in 1979 (revised in 2003 (11,12)), which was used in the first EBP ‘how-to’ guide in 2000. (13) This system established the RCT at the top of the research hierarchy and evolved to systematic review or meta-analysis being preferred to single RCTs.
A sense of the rationale for these hierarchies of evidence is contained in the following quote from the 2004 Centre for Health Evidence User’s Guide (5):
Evidence-based medicine de-emphasizes intuition, unsystematic clinical experience, and pathophysiologic rationale as sufficient grounds for clinical decision-making, and stresses the examination of evidence from clinical research. Evidence-based medicine requires new skills of the physician, including efficient literature-searching, and the application of formal rules of evidence in evaluating the clinical literature. (p.2420)
EBP claims to be both epistemological and clinical, as it proposes optimal ways to develop knowledge and asserts that information obtained from high-quality scientific research is the foundation for effective clinical practice. (14) Some advocates of EBP argue strongly that the use of scientific research is superior to the use of other forms of knowledge, such as individual clinical experience, physiologic principles, expert opinion and understanding of patient, professional, or social values. (1,5,15,16) Hierarchies of evidence place expert opinion and individual case reports at the lowest level of quality. Others argue that scientific evidence must be part of a decision making process that integrates all of these forms of knowledge. (15) Rather than shifting away from expertise and expert opinion, the shift towards EBP is a shift towards a new kind of expertise , that of critically appraising relevant evidence and applying it to clinical practice. (17)
Practitioners engage in EBP in a series of steps. EBP demands that clinicians learn first to find, then analyze and finally to apply evidence in appropriate situations. Over time many tools for EBP have evolved, such as systematic reviews and CPGs, which can make EBP easier. Midwifery professional organizations often create their own CPGs, but midwives will often also use reviews and other evidence-based tools from other professions, such as obstetrics, pediatrics, family practice and nursing, to inform their practice.
Advocates in the early nineties posed EBP as a central paradigm shift for clinical care providers, promising not only a more systematic and scientific approach to clinical practice but also a challenge to practices based on tradition, professional opinion and authority. (1,5) Since that time, the concept that quality scientific evidence is fundamental to health care has been universally accepted, while at the same time debate about how to best produce, evaluate and apply evidence continues. Good evidence is now argued to be essential to both care providers and the recipients of care. (14,18,19)
Medical, midwifery, and nursing education have enthusiastically adopted EBP. In 2003, the journal, Evidence-Based Midwifery, began publication and there are now also many scholarly texts to guide evidence-based midwifery. (20,21) Linked with not only health care practice but also with education and with institutions that produce or support research, EBP is deeply entwined with research funding decisions and academic career paths (see Midwife as Researcher chapter). EBP has now become so ubiquitous, some worry that “evidence-based everything”, dilutes the meaning of the term. (22)
Did You Know?
An article published in the Journal of Advanced Nursing in 2002 charted the number of times EBP and its variants were used in the titles of articles or in abstracts published in the professional literature since it was first used in 1992. (23) Over its first decade EBP spawned not only thousands of articles, but many texts, several international journals and research institutions. (24)
External Link
The journal Evidence Based Midwifery from the Royal College of Midwives is available here: https://www.rcm.org.uk/access-evidence-based-midwifery-journal
12.3 The Intertwined Histories of EBP & Midwifery
Some of the early advocates for better scientific evidence were childbirth activists and feminist women’s health scholars. (25) Lack of scientific evidence for numerous routine obstetric practices was the basis for many critiques of the medical management of childbirth. These critiques helped shape both the development of the EBP paradigm and the development of midwifery in Canada. Early calls for EBP used examples of the wide variations in obstetric practice to make the case that an evidence-based approach was needed across medical professions. The differences in rates of induction and episiotomy in different hospitals in the same region and different regions in the same country were proof that a more scientific approach was needed. Welsh physician, Archie Cochrane (1909-1988), after whom the Cochrane Database of Systematic Reviews is named, is widely considered to be the founder of EBP in the UK. In 1979, Cochrane named obstetrics as one of the least evidence-based of the fields of medicine, but this was soon to change. (3)
External Link
The Cochrane Database of Systematic Review is available here: http://www.cochrane.org/
An enthusiastic and influential group of physicians, epidemiologists and teachers at McMaster University formed the Evidence-Based Medicine Working Group (EBMWG) in 1992. McMaster’s history as an innovative medical school, one that was willing to experiment with new approaches to clinical care and student admission and teaching, positioned it to be one of the birth places of the new EBP paradigm. Members included internal medicine specialists Gordon Guyatt, David Sackett and obstetrician Murray Enkin, all of whom were destined to become influential leaders of EBM, internationally. McMaster was also one of the Canadian leaders in family-centred maternity care. (26)
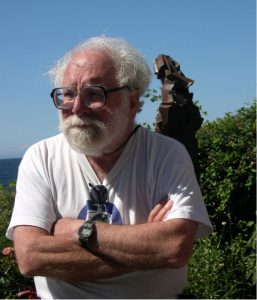
Murray Enkin (Figure 12-1) is a key figure in both the evidence and childbirth movements. As a family doctor in Saskatchewan he attended births, including those of his own children, in an environment he describes as low tech. From his earliest days as a medical student Enkin had a great respect for women during childbirth and for the process of natural birth. When the EBMWG formed, he already had a long history in working to humanize childbirth and had been frustrated by a lack of interest in family-centred approaches by other physicians and institutions. In the decades from the 1990s onwards, Enkin would emerge as an important champion of many reforms to maternity care including the legal recognition and acceptance of midwifery in Canada and for a fuller role for midwives in all jurisdictions. (3)
Enkin was a co-author of the first textbook of EBP in maternity care, Effective Care in Pregnancy and Childbirth (ECPC) (27), a large, two volume compilation of the best evidence from both clinical and social science perspectives. ECPC is remarkable in a number of ways, first in that it modelled the integration of inter-professional and inter-disciplinary perspectives (Figure 12-2). It modelled a democratization of health care practice that many EBP advocates hoped for, including as reviewers, consumer advocates, sociologists, anthropologists and basic scientists as well as family doctors, obstetricians and pediatricians. The authors also created an accessible paperback version, first published in 1989, for both professionals and the public called the Guide to Effective Care in Pregnancy and Childbirth. (27) Complied and disseminated prior to wide access to the internet, ECPC was a remarkable achievement and marked a new era in maternity care.

One powerful and controversial tool contained in ECPC was the summary list of practices that were beneficial, unknown or likely to be harmful. It also listed practices that did not have a strong enough evidence base to either encourage or discourage but which needed more evidence. The authors claimed there was evidence to encourage many practices that supported midwifery care, like one-to-one care in labour; intermittent auscultation of the fetal heart and mobility in labour; choice of birth place and care provider. Practices that they claimed should be abandoned included routine shaving; electronic fetal monitoring; arbitrary limits on the length of labour; episiotomy and separation of mother and baby. Childbirth reform movements had long expressed concern about the overuse of many of these procedures. (25,29–32) The lists in ECPC created a holistic vision of what a normal birth might look like (and what it might not). It also gave clear guidance when common interventions lacked an evidence-base (28):
First. . . the only justification for practices that restrict a woman’s autonomy, her freedom of choice and her access to her baby, would be clear evidence that these restrictive practices do more good than harm; and second, … any interference with the natural process of pregnancy and childbirth should also be shown to do more good than harm. We believe that the onus of proof rests on those who advocate any intervention that interferes with either of these principles. (p.389)
Many of the first champions of EBP in maternity care appear to have assumed that the systematic interpretation of scientific evidence would support a ‘family-centred’ or ‘woman-centered’ approach to childbirth that respected rather than pathologized the physiology of birth. (28,33) Midwife, Jilly Rosser, is one of the founders of Midwifery Information and Research Service, an evidence-based service for midwives in the UK. She spoke for many midwives in calling ECPC “a bible for midwives.” ECPC was popular with midwives, not only because it provided so much information to base practice on, but also because of the strong support it gave for normal birth. (34) Midwifery Professor and first Director of Midwifery Education at McMaster Karyn Kaufman described the reception of the midwifery community to ECPC by saying, “it felt like science was on our side.” (3) EBP seemed to support change, normal birth, choice and control, key demands of childbirth movements internationally. For Canadian midwives, not yet legally recognized in the early nineties, the EBP movement supported the central aspects of the model of care they were advocating for: continuity of care, choice of birth place and physiologic birth.
As the decade progressed EBP was swept forward by the information technology revolution and has transformed into the massive enterprise we know today. Some would say that from its origins as a new paradigm it has transformed not only into an institution but also an industry. (3) As the popularity and authority of EBP grew so did debate about it.
12.4 The Evidence Debates
In the first decades of EBP there has been a flurry of debate about its claim to be the new paradigm for health care. Some claimed that medicine has always based its work on research and that there was nothing really new about it. Others turned EBP’s own argument against it stating that there is no evidence for EBP. Some authors pushed against its growing authority worrying that it had become impossible to be against anything that claimed to be based on evidence, thus silencing the rebuttal and debate that is an important part of the scientific process. Advocates claimed that EBP breaks down hierarchies both within and between professions as well a with users of care and that it promotes dialogue. (5) Skeptics warned that despite good intentions on the part of the early EBP advocates, that the use of evidence for fiscal restraint and rationing of care rather than for good patient care would be worrisome (35), while others argued that allocation of limited funding should be based on evidence. (36) Another critique focused on the fact that EBP seemed to provide one right answer and to be a grand narrative that seemed reductionist and positivist. (15) This appeared to be out of step with postmodernist scholarship at a time when many disciplines were rejecting modernist notions and emphasizing concepts like partiality, situatedness, hybridity, ecology, and complexity. (3) EBP has also generated terms with more nuanced meaning such as evidence-informed practice (37), and labels with counter meanings such as practice-based evidence (38), or person-based evidence, (39) which reflect some of the debates about EBP.
These debates led evidence experts to clarify and defend EBP, to define what evidence is and what it is not (40) and to soften the hierarchy to be more inclusive of patient preference and other knowledge such as skill and judgement.
12.5 What EBP Can & Can’t Do
Despite the debates, the hopes and expectations for EBP in maternity care were high. As noted above, some hoped that EBP would help humanize childbirth and counted on it to bring change and choice. (3) Others hoped that if practice was based on best evidence it would bring clarity and take some of the uncertainty out of clinical practice. However, although scientific evidence can determine which test or treatment may work best over a population it does not eliminate the need for clinician skills, judgment and decision-making on the scale of individuals. One of the early goals was to eliminate the need to rely on expert opinion, yet EBP has increasingly demanded a new kind of expertise. Clinicians are now required to provide guidance through the lens of both scientific evidence and judgement based on experience. Advocates embraced the idea that EBP challenges authoritarian approaches to health care and demands life-long reflective practice from all practitioners. Despite these hopes, some worried that strong pressures in the system would lead to the use of evidence to support a pre-existing belief or practice. (3)
The law and ethics of health care demand that people are informed about and participate in decisions about their care. ECPC concisely states that the goal of scientific evaluation of health care is to determine the “most effective means to achieve” the objectives of care, but cannot set the objectives. (28) EBP does not eliminate the need to need to explore goals and objectives, client values and preferences to inform how evidence is applied to individuals. ECPC challenges the health care system to look at goals and objectives at an institutional level and for the system as a whole.
It is increasingly clear that some important questions cannot be addressed with RCTs and that the hierarchy of evidence does not apply to all questions about childbirth. (41,42) Pregnancy and birth are complex phenomena with many interdependent factors that may confound results of RCTs when results are applied in a real life setting. (41,42) As the evidence movement has matured, the value of different kinds of knowledge to answer many questions in maternity care has become clear, including observational studies, findings based on the analysis of large data sets, practice audits, and qualitative research and mixed methods approaches.
Many hoped that evidence would settle the debates about appropriate rates of intervention in childbirth. After more than two decades of EBP variations in rates of induction and cesarean remain problematic all over the world. The application of evidence sometimes leads to unexpected effects, such as the recommendation for induction of labour between 41-42 weeks appearing to increase the rate of induction prior to 41 weeks. (43) Both the research process itself and the application of the evidence it provides involve interpretation. It is clear that personal beliefs and values and institutional norms can influence how evidence is interpreted. Some evidence is taken up very readily and other evidence seems almost impossible to implement widely. An example is intermittent auscultation of the fetal heart (IA) in a low risk pregnancy. Despite national obstetric guidelines (44) advocating IA for low risk pregnancy, high rates of routine electronic fetal heart rate monitoring are difficult to change. (3) Many factors far beyond evidence have an impact on how and if evidence is applied. (3) Societies in the developed world seem to have a tendency to default towards technology, and evidence that advocates for more technology seems to be taken up more easily than evidence that advocates less technology. (3) Workplace demands for efficiency and staffing pressures can influence what evidence is applied and what evidence is not. Evidence that provides multiple interpretations should facilitate client choices, however health systems commonly aim to standardize rather than individualize care and implement singular understandings and routine practice rather than client choice. Clearly, the debates about EBP will continue to evolve and change.
External Link
The Society of Obstetricians and Gynaecologists of Canada obstetric guidelines can be found here: http://sogc.org/wp-content/uploads/2013/01/gui197CPG0709r.pdf
12.6 Evidence-Informed Midwifery
Midwives around the world enthusiastically support EBP and there is extensive literature and many resources to support evidence-based midwifery. Most midwifery education programs are built around enabling students to acquire and use the skills required for EBP, such as how to search the research literature and how to critically appraise research articles. Many midwifery education programs are designed to expose students to both science and social science knowledge and expect them to use both to inform practice.
Many midwives feel most comfortable using the label, evidence-informed midwifery. The term integrates the concept of informed choice and EBP. It acknowledges the need for midwives to explore the values and preferences of their clients. It fits well with the midwifery philosophy in which clients are the primary decision makers, working in partnership with midwives to determine the best course of care. The term also acknowledges that midwifery decisions will include contextual factors. The midwifery model of care is an ideal model for what could be called the integrative approach to EBP, one that uses clinical research evidence as one of the many sources of knowledge that are essential to consider in assisting clients to make decisions.
12.6.1 For Normal Birth
Much midwifery work on EBP looks at the evidence through the lens of normal birth. Many midwifery researchers actively focus their research on topics relevant to normal birth, including how to preserve as much normalcy as possible even in complex situations. There are many evidence-based tools produced by midwives to support normal birth such as the Royal College of Midwives’ Campaign for Normal Birth in the UK and the American College of Nurse Midwives’ Normal Birth: Pearls in your pocket or the Wales Normal Birth Pathway. Midwifery research supporting the safety of out of hospital birth has been integrated into national guidelines in the UK (45) through the advocacy of midwives working on inter-professional guidelines committees.
External Links
Information on the Royal College of Midwives’ Campaign for Normal Birth in the UK can be found here: http://www.rcmnormalbirth.org.uk/
The American College of Nurse Midwives’ presentation of Normal Birth: Pearls in your Pocket can be found here:
http://www.midwife.org/Evidence-Based-Practice-Pearls-of-Midwifery
Documents related to the Wales National Birth Pathway can be found here: http://www.wales.nhs.uk/sites3/page.cfm?orgid=327&pid=5786
12.6.2 For Advocacy
Many midwives find EBP a powerful tool for advocacy and actively use evidence both in day-to-day practice and in policy making at every level from practice to institution to broad health system forums. Midwives have described carrying a file of important studies, reviews and CPGs with them, so that if other care providers questioned the care they were providing they could produce the evidence and have a more informed discussion with their colleagues. (3) International work studying the implementation of evidence-based midwifery reveals that midwives often face barriers in the hospital setting, including particularly lack of autonomy. (46) Some jurisdictions have created midwifery staff positions (47) and research networks (48), to promote and support EBP. Research in New Zealand shows higher rates of EBP at home births than hospital births even when the same midwives have been in attendance, which may support the case that autonomous midwifery practice is an ideal setting for EBP. (49)
12.6.3 For Evaluation
Midwives also contribute to evidence-informed midwifery by critically appraising research done by others. The midwifery model supports spending enough time with clients to explore multiple interpretations of the evidence. Much of the important RCT evidence about childbirth that has emerged over the past two decades, for example from RCTs about post-term pregnancy or pre-labour rupture of membranes at term, is open to multiple interpretations and approaches, with risks and benefits to either a decision to intervene or take an expectant management approach. The differences in outcomes between alternate approaches may be similar or small; therefore, the importance of discussion and choice rather than routine care is heightened. The midwifery model, with its commitment to informing clients of risks, benefits and alternatives and exploring the client’s goals and values, is ideal for exploring multiple options rather than one right way.
Midwifery professional associations, such as the Association of Ontario Midwives (AOM), have produced an impressive set of CPGs formed through a values based approach. These values include providing guidance to midwives hoping to support normal birth and informed choice. They prioritize areas of practice where midwifery interpretations of the evidence differ from current medical guidelines and look at multiple rather than singular interpretations of evidence. They create companion resources and cell phone apps for clients to use. The following example is of a recommendation from a midwifery CPG on post-term pregnancy. Note that it integrates information, critical appraisal, choice and support for normal birth, and uses the evidence grading system of the CTFPHC (4):
Inform clients that the absolute risk of perinatal death from 40+0 weeks to 41+0 weeks to 42+0 weeks’ gestational age changes from 2.72/1000 to 1.18/1000 to 5.23/1000; currently available research is not of high quality and has not established an optimal time for induction. Therefore, women with uncomplicated postdates pregnancies should be offered full support in choices that will allow them to enter spontaneous labour. A policy of expectant management to 42+0 weeks following an informed choice discussion is the most appropriate strategy for women who wish to maximize their chance of normal birth. (p. 19)
External Link
The full Clinical Practice Guideline No. 10: Management of the Uncomplicated Pregnancy beyond 41+0 Weeks’ Gestation is available here: http://www.aom.on.ca/files/Health_Care_Professionals/Clinical_Practice_Guidelines/CPG_beyond_41_FINAL.pdf
12.7 Clinical Applications
What would an evidence-informed midwifery practice look like? It would mean that as a midwife you listen to the clients and families you work with and find out what is important to them. You continually update your knowledge of the evidence. To do this you use relevant guidelines such as the AOM, Society of Obstetricians and Gynaecologists of Canada (SOGC), or National Institute for Health and Care Excellence (NICE) guidelines and other evidence-based resources. You know how to search the web to find high-quality systematic reviews and use the Cochrane database. You get alerts to your preferred journals to keep abreast of new findings. In clinical practice you ask yourself key questions, including:
- What is the clinical situation and the specific findings for this client?
- What does your client say? What do other family members think? What is important to them?
- What is the evidence? How is it relevant to the general clinical situation? To the individual?
- What does your experience tell you?
- How can you best communicate the risks, benefits and the alternatives?
You use evidence to inform and support choice and actively give permission for reasonable alternatives. You develop your skills of critical appraisal and clinical reasoning and you become a skilled advocate for your clients and the profession, using evidence. By actively interpreting evidence to support normal birth you help lower rates of intervention in your practice settings. You let evidence challenge you and your worldview. You try to be open about your biases and engage in open dialogue about philosophies of birth and childbirth care. You respect evidence but know there is more to good practice than good evidence.
12.8 Conclusion
Midwives have an enthusiastic and critically aware engagement with EBP. Midwives have an ideal model of practice to implement evidence-informed care, with the benefits of autonomy and continuity of care. A commitment to EBP and participating in the creation of evidence-based tools provides an important common ground for midwives and other health professionals. Internationally, midwives recognize that evidence is an essential part of providing good care. Midwives contribute to the development of EBP by advocating for evidence-based approaches to care in their practice settings and at higher policy levels. While midwives want to contribute to the research, which creates better evidence and want to use evidence to inform their practice, they recognize that evidence alone cannot determine individual values and objectives of care. Midwives can and are playing a valuable role in the scholarship of EBP and in the integration of evidence with client choices and values.
Acknowledgements
Much of this chapter is based on my PhD dissertation Reconsidering Evidence: Evidence-based practice in maternity care in Canada
References
- Evidence C for H. Evidence-based medicine: a new approach to teaching the practice of medicine. Users’ guide to evidence-based practice. [Internet]. McGraw-Hill Education; 2001. Available from: http://jamaevidence.mhmedical.com/content.aspx?bookid=847§ionid=69030714%0D
- Page LA. Evidence-based practice in midwifery: a virtual revolution? J Clin Eff. 1997;2(1):10–3.
- Van Wagner V. Reconsidering Evidence: Evidence-based Practice and Maternity Care in Canada. PhD Dissertation [Internet]. York University; 2013. Available from: http://yorkspace.library.yorku.ca/xmlui/handle/10315/31318
- Association of Ontario Midwives. Clinical Practice Guidelines [Internet]. Available from: http://www.aom.on.ca/Health_Care_Professionals/Clinical_Practice_Guidelines/
- Evidence-Based Medicine Working Group. Evidence-based medicine: A new approach to teaching the practice of medicine. JAMA [Internet]. 1992;268(17):2420–5. Available from: http://dx.doi.org/10.1001/jama.1992.03490170092032
- Devereaux PJ, Manns BJ, Ghali WA, Quan H, Lacchetti C, Montori VM, et al. Physician interpretations and textbook definitions of blinding terminology in randomized controlled trials. JAMA [Internet]. 2001;285(15):2000–3. Available from: http://dx.doi.org/10.1002/9780470691922.ch3%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/11308438
- Haahr MT, Hróbjartsson A. Who is blinded in randomized clinical trials? A study of 200 trials and a survey of authors. Clin Trials [Internet]. 2006;3(4):360–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17060210
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ [Internet]. 2010 [cited 2017 Jul 31];340. Available from: http://www.bmj.com/content/340/bmj.c869
- Sackett DL, Strauss SE, Richardson WC, Rosenberg W, Haynes RM. Evidence-based medicine: How to practice and teach EBM. New York, NY: Churchill Livingstone; 2000.
- Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ [Internet]. 2008 [cited 2017 Jul 31];337. Available from: http://www.bmj.com/content/337/bmj.a2390
- CANADIAN TASK FORCE ON THE PERIODIC HEALTH EXAMINATION. The period health examination. CMA [Internet]. 1979;121:1193–254. Available from: http://www.cmaj.ca/content/169/3/207.full
- Canadian Task Force on Preventive Health Care CTF on PH. New grades for recommendations from the Canadian Task Force on Preventive Health Care [Internet]. CMAJ. Canadian Medical Association; 2003 [cited 2017 Jul 28]. p. 207–8. Available from: http://www.cmaj.ca/content/169/3/207.full
- Sackett DL, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. 1st ed. New York: Churchill Livingstone; 1997. 250 p.
- Sackett DL, Rosenberg WM. The need for evidence-based medicine. J R Soc Med. 1995;88:620–4.
- Tonelli MR. The philosophical limits of evidence-based medicine. Academic Medicine. 1998. p. 1234–40.
- Grimes DA, Schulz KF. Clinical research in obstetrics and gynecology: a Baedeker for busy clinicians. Obstet Gynecol Surv [Internet]. 2002 Sep [cited 2017 Jul 28];57(9 Suppl 3):S35-53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12479352
- Rees C. An introduction to research for midwives. Churchill Livingstone/Elsevier; 2012. 264 p.
- Sackett DL, Rosenberg WMC. On the need for evidence‐based medicine. Health Economics. 1995;4(4):249–54.
- Hannah ME. Good Evidence Is Necessary for Good Patient Care. J SOGC [Internet]. 2001 Dec [cited 2017 Jul 28];23(12):1190–3. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0849583116309661
- Spiby H, Munro J. Evidence based midwifery : applications in context. Wiley-Blackwell; 2010. 203 p.
- Brayford D, Chambers R, Boath E, Rogers D. Evidence-based care for midwives : clinical effectiveness made easy. Staffordshire University; 2008. 155 p.
- Ciliska D, Strauss SE, Richardson WS, Rosenberg WMC, Haynes RB. Educating for evidence-based practice. J Prof Nurs [Internet]. Churchill-Livingstone, London; 2005 Nov 1 [cited 2017 Jul 28];21(6):345–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16311229
- French P. What is the evidence on evidence-based nursing? An epistemological concern. J Adv Nurs [Internet]. Blackwell Science Ltd.; 2002 Feb 1 [cited 2017 Jul 31];37(3):250–7. Available from: http://doi.wiley.com/10.1046/j.1365-2648.2002.02065.x
- French P. What is the evidence on evidence-based nursing? An epistemological concern. J Adv Nurs [Internet]. 2002 Feb [cited 2017 Jul 28];37(3):250–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11851795
- Shearer M. Maternity patient movements in the United States 1820-1985. In: Chalmers I, Enkin M, Keirse M, editors. Effective care in pregnancy and childbirth. Oxford: Oxford University Press; 1989.
- Mykhalovskiy E, Weir L. The problem of evidence-based medicine: directions for social science. Soc Sci Med [Internet]. 2004 Sep [cited 2017 Jul 31];59(5):1059–69. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15186905
- Chalmers I, Enkin M, Keirse MJNC. Effective care in pregnancy and childbirth. Oxford: Oxford University Press; 1989. 1545 p.
- Enkin M, Keirse MJNC, Chalmers I. Guide to effective care in pregnancy and childbirth. 1st ed. Toronto: Oxford University Press; 1989.
- Ruzek SB. The women’s health movement. New York: Praeger Publishers; 1978. 351 p.
- Reiger KM, Kitzinger S. Our bodies, our babies : the forgotten women’s movement [Internet]. 1st ed. Melbourne University; 2001 [cited 2017 Jul 31]. 335 p. Available from: https://www.mup.com.au/books/9780522849820-our-bodies-our-babies
- Haire D. The cultural warping of childbirth. Icea News [Internet]. 1972 [cited 2017 Jul 31];11(1):5–35. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12261812
- Oakley A. Women Confined: Towards a Sociology of Childbirth. New York: Schocken Books; 1988. 334 p.
- Chard T, Richards M. Benefits and Hazards of the New Obstetrics. 1st ed. Philadelphia: J. B. Lippincott;
- Rosser J. Book review: Effective care in pregnancy and childbirth and A guide to effective care in pregnancy and childbirth. MEDIRS Midwifery Digest. 1989 Dec;
- Kleinert S. Rationing of health care—how should it be done? Lancet [Internet]. 1998 Oct 17 [cited 2017 Jul 31];352(9136):1244. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9788452
- Sackett DL. Evidence-based medicine and treatment choices. Lancet (London, England) [Internet]. Churchill-Livingstone, London; 1997 Feb 22 [cited 2017 Jul 31];349(9051):570; author reply 572-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9048806
- Wickham S. Evidence-informed midwifery. 1. What is evidence-informed midwifery? Midwifery Today Int Midwife [Internet]. 1999 [cited 2017 Jul 31];(51):42–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10808876
- Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Fam Pract [Internet]. 2008 Dec 1 [cited 2017 Jul 31];25(Supplement 1):i20–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18794201
- Yardley L, Morrison L, Bradbury K, Muller I. The Person-Based Approach to Intervention Development: Application to Digital Health-Related Behavior Change Interventions. J Med Internet Res [Internet]. 2015 Jan 30 [cited 2017 Jul 31];17(1):e30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25639757
- Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ [Internet]. 1996 [cited 2017 Jul 31];312(7023). Available from: http://www.bmj.com/content/312/7023/71
- Kotaska A. Inappropriate use of randomised trials to evaluate complex phenomena: case study of vaginal breech delivery. BMJ [Internet]. 2004 [cited 2017 Jul 31];329(7473). Available from: http://www.bmj.com/content/329/7473/1039
- Jadad AR, Enkin M. Randomized controlled trials : questions, answers, and musings. London: BMJ Books/Blackwell Publishing; 2007. 136 p.
- Harris S, Buchinski B, Grzybowski S, Janssen P, Mitchell GW, Farquharson D, et al. Induction of labour: a continuous quality improvement and peer review program to improve the quality of care. CMAJ [Internet]. Canadian Medical Association; 2000 Oct 31 [cited 2017 Jul 31];163(9):1163–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11079064
- Liston R, Sawchuck D, Young D, Society of Obstetrics and Gynaecologists of Canada, British Columbia Perinatal Health Program. Fetal health surveillance: antepartum and intrapartum consensus guideline. J Obstet Gynaecol Can [Internet]. 2007 Sep [cited 2017 Jul 31];29(9 Suppl 4):S3-56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17845745
- National Institute for Health and Care Excellence. Intrapartum care for healthy women and babies [Internet]. NICE; 2014 [cited 2017 Jul 31]. Available from: https://www.nice.org.uk/guidance/cg190
- Bick D, Dowswell T, Ismail KMK, al. et, Hills RK, Ismail KI. Evidence based midwifery practice: Take care to “mind the gap.” Midwifery [Internet]. STTI/Wiley-Blackwell Science; 2011 Oct 1 [cited 2017 Jul 31];27(5):569–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21907879
- Kennedy HP, Doig E, Hackley B, Leslie MS, Tillman S. “The Midwifery Two-Step”: A Study on Evidence-Based Midwifery Practice. J Midwifery Womens Health [Internet]. 2012 Sep [cited 2017 Jul 31];57(5):454–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22845643
- Fahy K. Evidence-based midwifery and power/knowledge (editorial). Women and Birth [Internet]. 2008 Mar [cited 2017 Jul 31];21(1):1–2. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1871519207001230
- Miller S, Skinner J. Are First-Time Mothers Who Plan Home Birth More Likely to Receive Evidence-Based Care? A Comparative Study of Home and Hospital Care Provided by the Same Midwives. Birth [Internet]. 2012 Jun 1 [cited 2017 Jul 31];39(2):135–44. Available from: http://doi.wiley.com/10.1111/j.1523-536X.2012.00534.x

