6.4 Administering Medications Rectally and Vaginally
Medication Administered Rectally
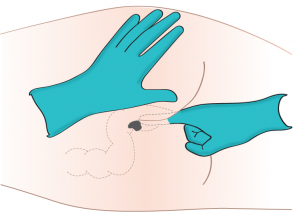
The rectal route (see Figure 6.1) is not as reliable in absorption and distribution as oral and parenteral routes. The rectal route is, however, relatively safe because there is less potential for adverse effects (Perry et al., 2014). Rectal medications are given for their local effects in the gastrointestinal system (e.g., laxatives) or their systemic effects (e.g., analgesics when oral route is contraindicated). Rectal medications are contraindicated after rectal or bowel surgery, with rectal bleeding or prolapse, and with low platelet counts. Checklist 46 outlines the procedure for administering rectal suppositories or enemas.
Checklist 46: Medication Administered RectallyDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
|||
Safety considerations:
|
|||
| Steps | Additional Information | ||
|---|---|---|---|
| 1. Check MAR against doctor’s orders. |
Check that MAR and doctor’s orders are consistent.  Night staff usually complete and verify this check as well. |
||
2. Perform the SEVEN RIGHTS x 3 (must be done with each individual medication):
Medication calculation: D/H x S = A (D or desired dosage/H or have available x S or stock = A or amount prepared) |
The right patient: check that you have the correct patient using two patient identifiers (e.g., name and date of birth).
 The right medication (drug): check that you have the correct medication and that it is appropriate for the patient in the current context. The right dose: check that the dose makes sense for the age, size, and condition of the patient. Different dosages may be indicated for different conditions. The right route: check that the route is appropriate for the patient’s current condition. The right time: adhere to the prescribed dose and schedule. The right reason: check that the patient is receiving the medication for the appropriate reason. The right documentation: always verify any unclear or inaccurate documentation prior to administering medications.  NEVER document that you have given a medication until you have actually administered it. |
||
3. The label on the medication must be checked for name, dose, and route, and compared with the MAR at three different times:
|
 These checks are done before administering the medication to your patient. If taking drug to bedside (e.g., eye drops), do third check at bedside. |
||
| 4. If possible, have patient defecate prior to rectal medication administration. | Medication should not be inserted into feces. | ||
| 5. Ensure that you have water-soluble lubricant available for medication administration. | Lubricant reduces friction as suppository enters rectal canal. | ||
| 6. Explain the procedure to the patient. If patient prefers to self-administer the suppository/enema, give specific instructions to patient on correct procedure. | Patient may feel more comfortable self-administering suppository. | ||
| NOTE: Unintended vagal stimulation may occur, resulting in bradycardia in some patients. Be aware that the rectal route may not be suitable for certain cardiac conditions. Notify physician. | |||
7. Raise bed to working height.
|
Positioning helps prevent injury to nurse administering medication. This protects patient’s privacy and facilitates relaxation.
Drape protects linens from potential fecal drainage. |
||
| 8. Apply clean non-sterile gloves. | Gloves protect the nurse from contact with mucous membranes and body fluids.
 |
||
| 9. Assess patient for diarrhea or active rectal bleeding. | Rectal medications are contraindicated in these situations. | ||
| 10. Apply clean non-sterile gloves if previous gloves were soiled. | Gloves protect the nurse from contact with mucous membranes and body fluids.
 |
||
| 11. Remove wrapper from suppository/tip of enema and lubricate rounded tip of suppository and index finger of dominant hand with lubricant.
If enema, lubricate only tip of enema. |
Lubricant reduces friction as suppository/enema enters rectal canal.
 |
||
| 12. Separate buttocks with non-dominant hand and, using gloved index finger of dominant hand, insert suppository (rounded tip toward patient) into rectum toward umbilicus while having patient take a deep breath, exhale through the mouth, and relax anal sphincter.
If enema: Expel air from enema and then insert tip of enema into rectum toward umbilicus while having patient take a deep breath, exhale through the mouth, and relax anal sphincter. |
You should feel the anal sphincter close around your finger after insertion. Forcing the suppository/enema through a clenched sphincter will cause pain and, potentially, rectal damage. | ||
| 13. With your gloved finger, insert suppository along wall of rectum about 5 cm beyond anal sphincter. Do not insert the suppository into feces.
If enema: roll plastic bottle from bottom to tip until all solution has entered rectum and colon. |
Suppository should be against rectal mucosa for absorption and therapeutic action. Inserting suppository into feces will decrease its effectiveness. | ||
| 14. Option: A suppository may be given through a colostomy (not ileostomy) if prescribed. | The patient should lie supine and a small amount of lubricant should be used. | ||
| 15. Remove finger and wipe patient’s anal area. | Wiping removes excess lubricant and provides comfort to the patient. | ||
| 16. Ask patient to remain on side for 5 to 10 minutes. | This position helps prevent the expulsion of suppository. | ||
| 17. Discard gloves by turning them inside out and disposing of them and any used supplies as per agency policy. Perform hand hygiene. | Using gloves reduces transfer of microorganisms.
  |
||
| 18. Ensure call bell is nearby and bedpan/commode is available and close by. | If suppository is a laxative or stool softener, patient will require a bedpan/commode or close proximity to toilet.
 |
||
| 19. Document procedure as per agency policy and include patient’s tolerance of administration. | Timely and accurate documentation promotes patient safety. | ||
| Data source: BCIT, 2015; Lilley et al., 2011; Perry et al., 2014 | |||
Medication Administered Vaginally
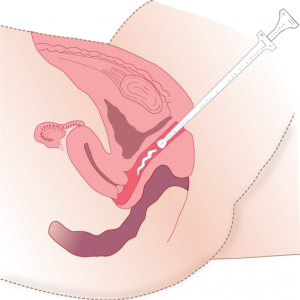
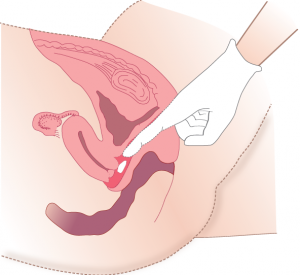
Female patients may require vaginal suppositories to treat vaginal infections. Vaginal suppositories are larger and more oval than rectal suppositories, and are inserted with an applicator (see Figure 6.2) or by hand (see Figure 6.3). Checklist 47 outlines the procedure for administering vaginal suppositories or medications.
Checklist 47: Medication Administered VaginallyDisclaimer: Always review and follow your hospital policy regarding this specific skill. |
||||
Safety considerations:
|
||||
| Steps | Additional Information | |||
|---|---|---|---|---|
| 1. Check MAR against doctor’s orders. | Students must check that MAR and doctor’s orders are consistent.
 Night staff usually complete and verify this check as well. |
|||
2. Perform the SEVEN RIGHTS x 3 (must be done with each individual medication):
Medication calculation: D/H x S = A (D or desired dosage/H or have available x S or stock = A or amount prepared) |
The right patient: check that you have the correct patient using two patient identifiers (e.g., name and date of birth).
 The right medication (drug): check that you have the correct medication and that it is appropriate for the patient in the current context. The right dose: check that the dose makes sense for the age, size, and condition of the patient. Different dosages may be indicated for different conditions. The right route: check that the route is appropriate for the patient’s current condition. The right time: adhere to the prescribed dose and schedule. The right reason: check that the patient is receiving the medication for the appropriate reason. The right documentation: always verify any unclear or inaccurate documentation prior to administering medications.  NEVER document that you have given a medication until you have actually administered it. |
|||
3. The label on the medication must be checked for name, dose, and route, and compared with the MAR at three different times:
|
 These checks are done before administering the medication to your patient. If taking drug to bedside (e.g., eye drops), do third check at bedside. |
|||
| 4. Before inserting the medication vaginally, explain the procedure to the patient. If patient prefers to self-administer the vaginal medication, give specific instructions to patient on correct procedure. | Patient may feel more comfortable self-administering vaginal medication. | |||
| 5. Ensure that you have water-soluble lubricant available for medication administration. | Lubricant reduces friction against vaginal mucosa as medication is inserted. | |||
| 6. Have patient void prior to procedure. | Voiding prevents passing of urine during procedure. | |||
7. Raise bed to working height.
|
Position helps prevent injury to nurse administering medication.
Draping protects patient’s privacy and facilitates relaxation. |
|||
| 8. Apply clean non-sterile gloves. | Gloves protect the nurse from contact with mucous membranes and body fluids.
 |
|||
| 9. Remove suppository from wrapper and apply a liberal amount of water-soluble lubricant to suppository and index finger of dominant hand. Suppository should be at room temperature. | Lubricant reduces friction against vaginal mucosa as medication is inserted.
 |
|||
| 10. With non-dominant hand, gently separate labial folds. With gloved index finger of dominant hand, insert lubricated suppository about 8 to 10 cm along posterior vagina wall. | Exposes vaginal orifice and helps to ensure equal distribution of medication. | |||
| 11. Withdraw finger and wipe away excess lubricant. | Wiping maintains patient comfort. | |||
| NOTE: An applicator may be used to insert vaginal medication. Follow procedure above and specific manufacturer directions. | ||||
| 12. Discard gloves by turning them inside out and disposing of them and any used supplies as per agency policy. Perform hand hygiene. | Using gloves reduces transfer of microorganisms.
  |
|||
| 13. Document procedure as per agency policy, and include patient’s tolerance of administration. | Timely and accurate documentation promotes patient safety. | |||
| Data source: Lilley et al., 2011; Perry et al., 2014 | ||||
Critical Thinking Exercises
- Your patient has a colostomy, and a laxative has been prescribed. Discuss the procedure for administering a laxative in this situation.
- Your patient prefers to self-administer her vaginal suppository. Outline the steps you would explain for safe and appropriate administration of a vaginal medication.

