15.2 – Anatomy & Physiology of the Sensory System
Audition (Hearing), Equilibrium (Balance), and Somatosensation (Touch)
Watch Hearing & Balance: Crash Course Anatomy & Physiology #17 (11 min) on YouTube
Media 15.2: CrashCourse. (2015, May 4). Hearing & balance: Crash Course anatomy & Physiology #17 [Video]. YouTube. https://youtu.be/Ie2j7GpC4JU
Audition (Hearing)
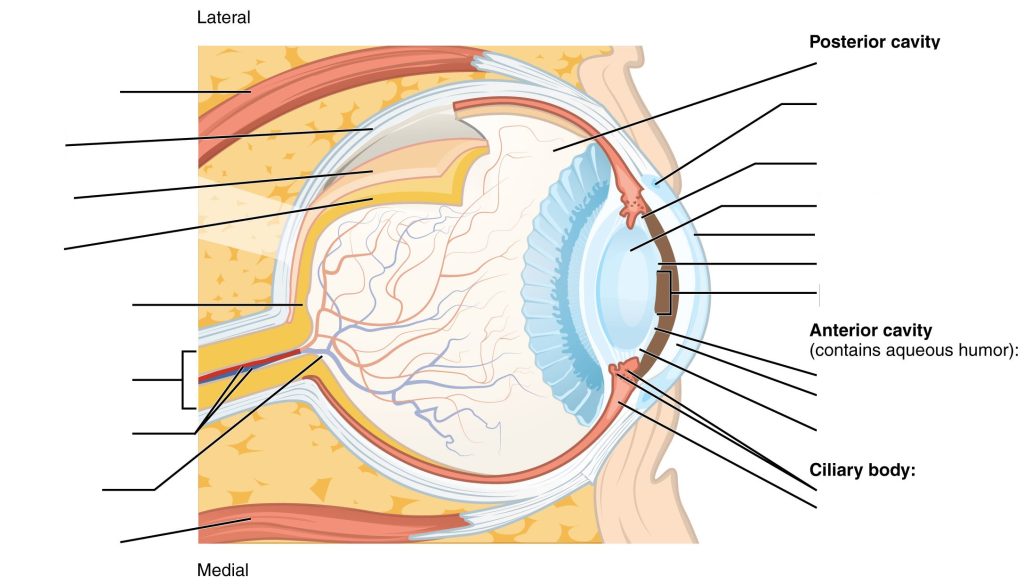
Hearing, or audition, is the transduction of sound waves into a neural signal that is made possible by the structures of the ear (see Figure 15.1).
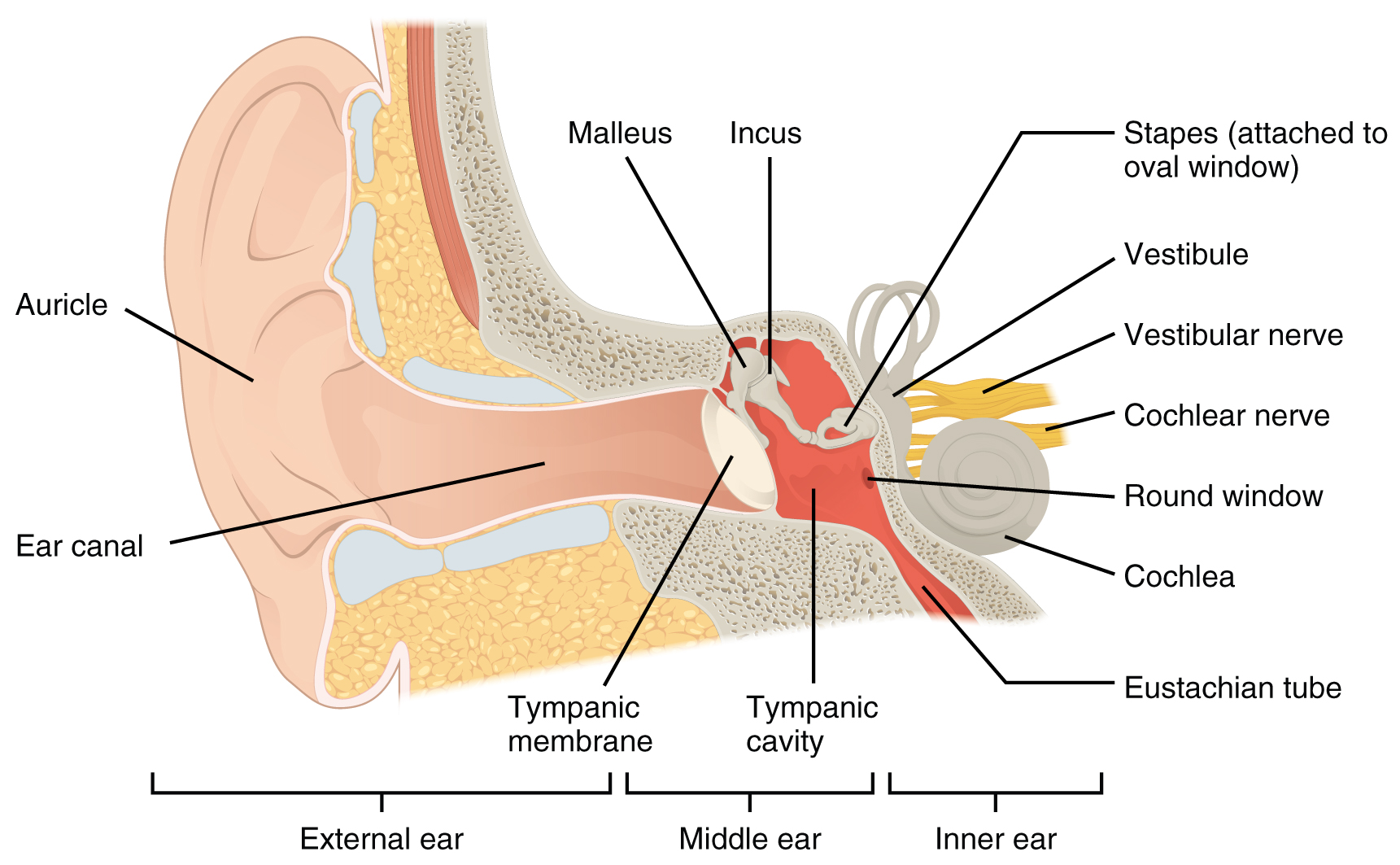
- The external ear consists of the auricle, sometimes referred to as the pinna, ear canal, and tympanic membrane.
The C-shaped curves of the auricle direct sound waves toward the auditory canal. The canal enters the skull through the external auditory meatus of the temporal bone. At the end of the auditory canal is the tympanic membrane, which vibrates after it is struck by sound waves. - The middle ear consists of the ossicles, oval window, and tympanic membrane.
The three ossicles are the malleus, incus, and stapes, which are Latin names that roughly translate to hammer, anvil, and stirrup. The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is then attached to the inner ear, where the sound waves will be transduced into a neural signal. Vibrations of the ossicles travel through the oval window, moving fluid in a wave-like motion. The frequency of the fluid waves match the frequencies of the sound waves. The middle ear is connected to the pharynx through the Eustachian tube, which helps equilibrate air pressure across the tympanic membrane. The tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning.
- The inner ear is often described as a bony labyrinth, as it is composed of a series of canals embedded within the temporal bone.
It consists of the cochlea which is responsible for hearing and the vestibule that is responsible for balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, these two distinct bundles travel together from the inner ear to the brain stem as the vestibulocochlear nerve. Sound is transduced into neural signals within the cochlear region of the inner ear, which contains the sensory neurons of the spiral ganglia. These ganglia are located within the spiral-shaped cochlea of the inner ear. The cochlea is attached to the stapes through the oval window.
The image below is a cross-sectional view of the cochlea that shows the scala vestibuli and scala tympani run along both sides of the cochlear duct (see Figure 15.2). The cochlear duct contains several organs of Corti, which tranduce the wave motion of the two scala into neural signals. The organs of Corti lie on top of the basilar membrane, which is the side of the cochlear duct located between the organs of Corti and the scala tympani. As the fluid waves move through the scala vestibuli and scala tympani, the basilar membrane moves at a specific spot, depending on the frequency of the waves. Higher frequency waves move the region of the basilar membrane that is close to the base of the cochlea. Lower frequency waves move the region of the basilar membrane that is near the tip of the cochlea.
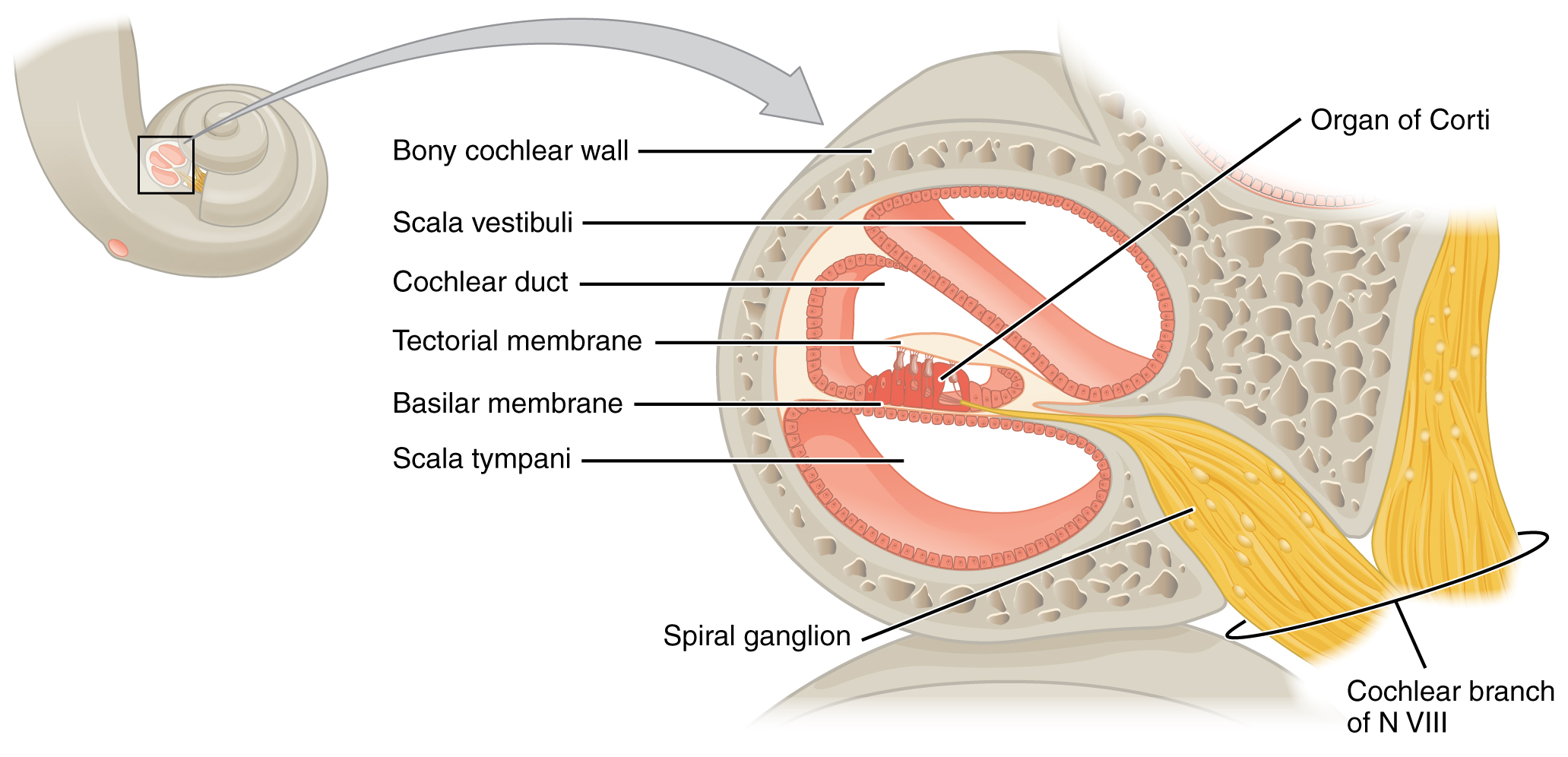
The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 Hz, which is the range of sound that human ears can detect. The unit of Hertz measures the frequency of sound waves in terms of cycles produced per second. Frequencies as low as 20 Hz are detected by hair cells at the apex, or tip, of the cochlea. Frequencies in the higher ranges of 20 KHz are encoded by hair cells at the base of the cochlea, close to the round and oval windows. Most auditory stimuli contain a mixture of sounds at a variety of frequencies and intensities (represented by the amplitude of the sound wave). The hair cells along the length of the cochlear duct, which are each sensitive to a particular frequency, allow the cochlea to separate auditory stimuli by frequency, just as a prism separates visible light into its component colours.
Did You Know?
Sound travels at speed of 1,130 feet per second.
Equilibrium (Balance)
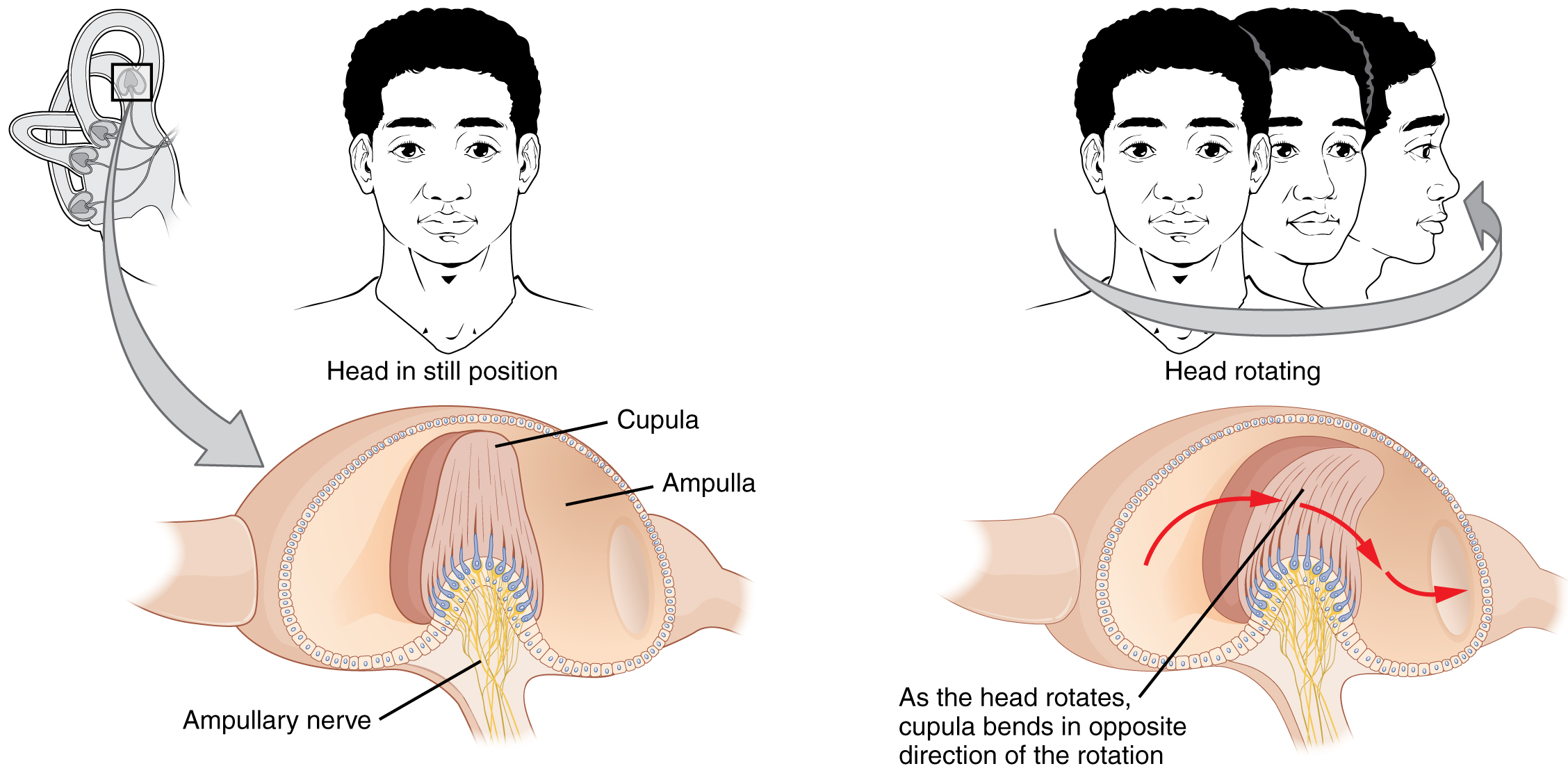
Along with audition, the inner ear is responsible for encoding information about equilibrium. The cells that sense head position, head movement, and body motion are located within the vestibule of the inner ear. Head position is sensed by otolith organs, whereas head movement is sensed by the semicircular canals (see Figure 15.3). The neural signals generated in the vestibular ganglion are transmitted through the vestibulocochlear nerve to the brain stem and cerebellum.
Somatosensation (Touch)
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs.
Did You Know?
With the aging process, humans lose sensory receptors cells including cells which detect pain and temperature changes.
The two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors.
For example, the sensation of heat associated with spicy foods involves capsaicin, the active molecule in hot peppers. Capsaicin molecules bind to a transmembrane ion channel in nociceptors that is sensitive to temperatures above 37°C. The dynamics of capsaicin binding with this transmembrane ion channel is unusual because the molecule remains bound for a long time. Because of this, it will decrease the ability of other stimuli to elicit pain sensations through the activated nociceptor. For this reason, capsaicin can be used as a topical analgesic, such as in products such as Icy Hot™.
Concept Check
- What structure exists within the ear to assist with maintaining equilibrium?
- What are the medical terms used to describe the sense of taste and touch?
Sensory System Ear Anatomy
Sensory System Ear Anatomy labeling activity (Text Version)
Label the diagram with correct words listed below:
- Parieto-occipital sulcus
- Ear canal
- Stapes (attached to oval window)
- Tympanic cavity
- Vestibule
- Cochlear nerve
- Eustachian tube
- Middle ear
- Tympanic membrane
- Malleus
- Incus
- Inner ear
- Round window
- External ear
- Cochlea
- Vestibular nerve
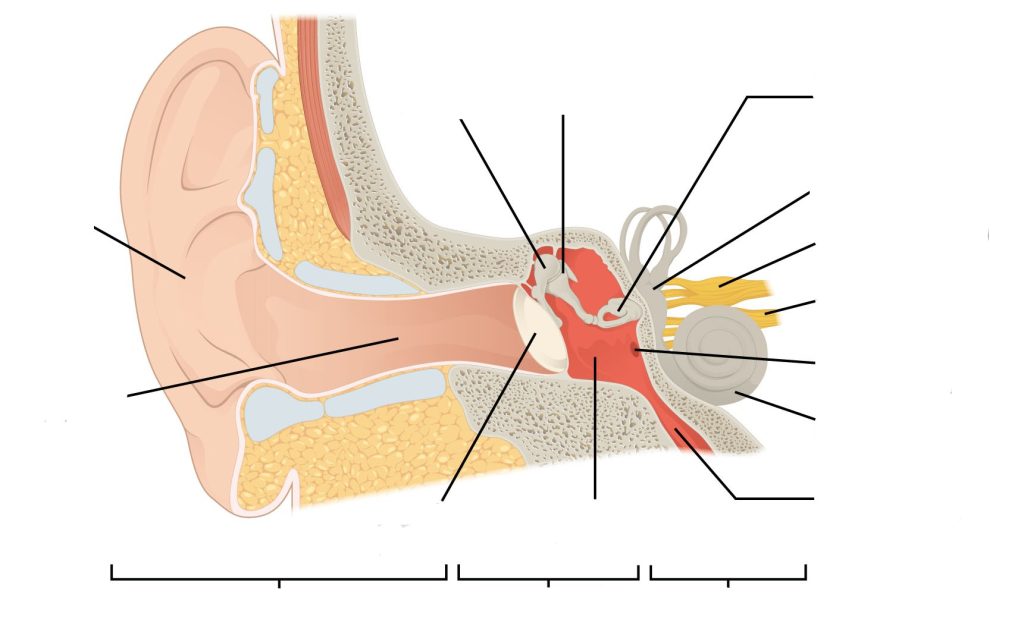
Check your answers [1]
Activity source: Sensory System Ear Anatomy by Gisele Tuzon, from Building a Medical Terminology Foundation, illustration from Anatomy and Physiology (OpenStax), licensed under CC BY 4.0./ Text version added.
Vision (Sight)
Watch Vision: Crash Course Anatomy & Physiology #18 (10 min) on YouTube
Media 15.3: CrashCourse. (2015, May 11). Vision: Crash Course Anatomy & Physiology #18 [Video]. YouTube. https://youtu.be/o0DYP-u1rNM
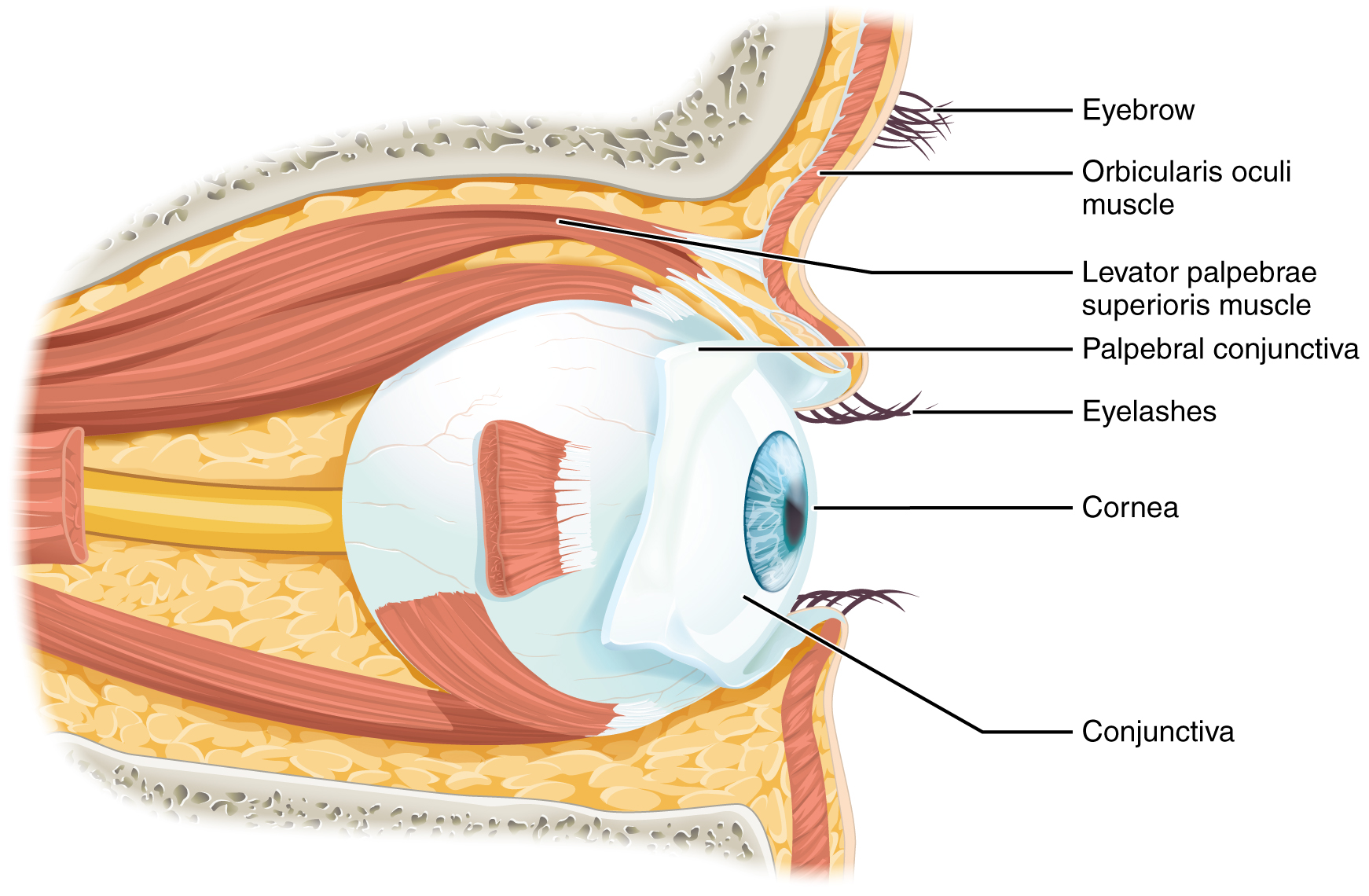
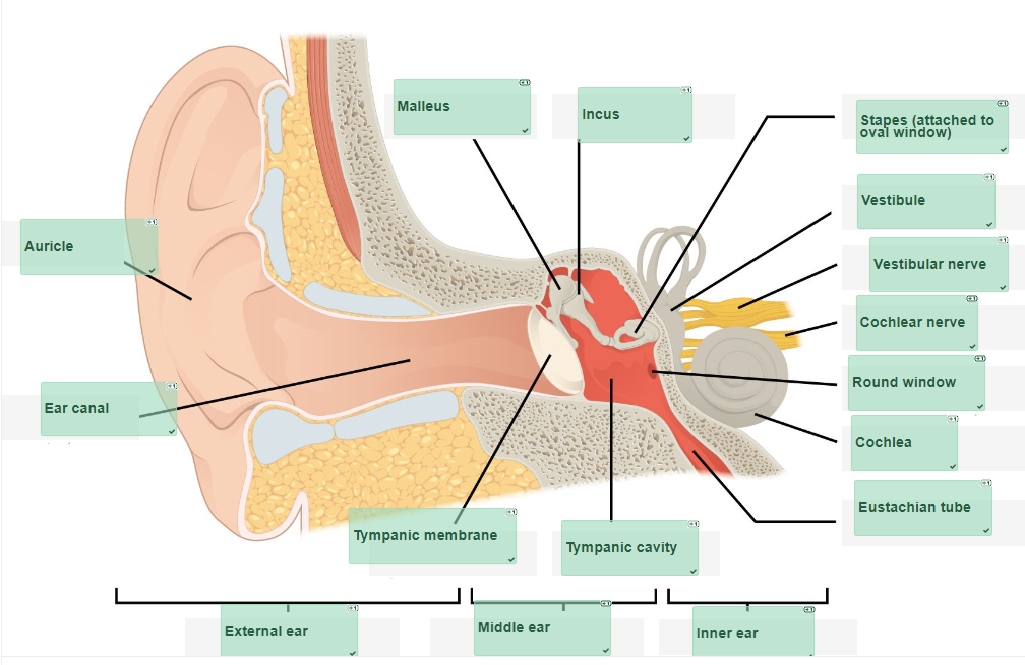
Vision is the special sense of sight that is based on the transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. The bony orbits surround the eyeballs, protecting them and anchoring the soft tissues of the eye (see Figure 15.4). The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye.
The inner surface of each lid is a thin membrane known as the palpebral conjunctiva. The conjunctiva extends over the sclera, connecting the eyelids to the eyeball. Tears are produced by the lacrimal gland, located beneath the lateral edges of the nose. Tears produced by this gland flow through the lacrimal duct to the medial corner of the eye, where the tears flow over the conjunctiva, washing away foreign particles.
Movement of the eye within the orbit is accomplished by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. Four of the muscles are arranged at the cardinal points around the eye and are named for those locations. They are the:
- superior rectus
- medial rectus
- inferior rectus
- lateral rectus
When each of these muscles contract, the eye moves toward the contracting muscle. For example, when the superior rectus contracts, the eye rotates to look up.
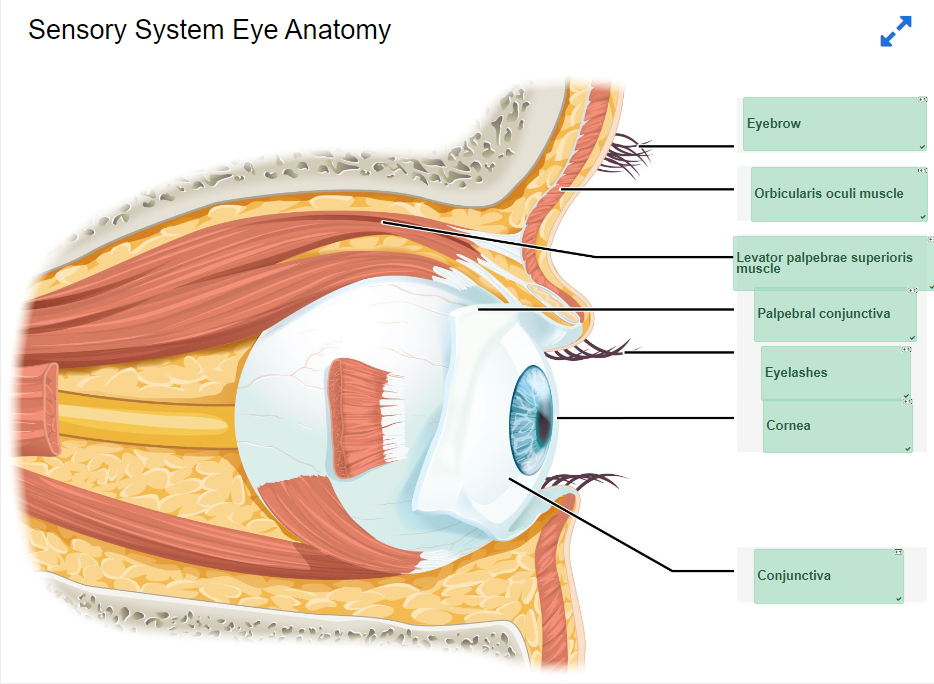
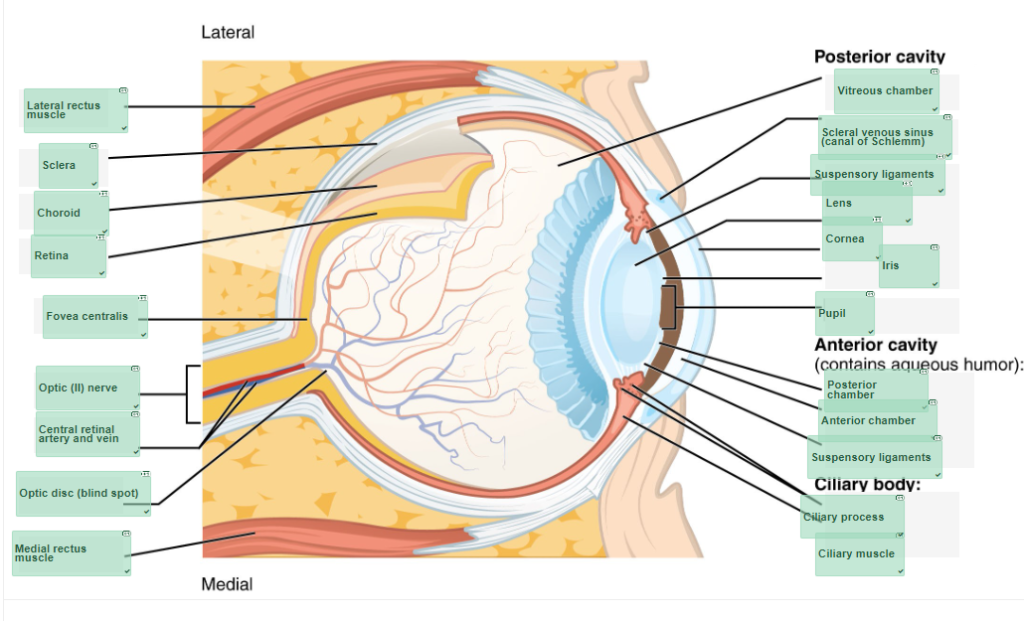
The eye itself is a hollow sphere composed of three layers of tissue.
- The outermost layer is the fibrous tunic, which includes the white sclera and clear cornea. The sclera accounts for five-sixths of the surface of the eye, most of which is not visible, though humans are unique compared with many other species in having so much of the “white of the eye” visible (see Figure 15.5). The transparent cornea covers the anterior tip of the eye and allows light to enter the eye.
- The middle layer of the eye is the vascular tunic, which is mostly composed of the choroid, ciliary body, and iris. The choroid is a layer of highly vascularized connective tissue that provides a blood supply to the eyeball. The choroid is posterior to the ciliary body, a muscular structure that is attached to the lens by zonule fibers. These two structures bend the lens, allowing it to focus light on the back of the eye. Overlaying the ciliary body, and visible in the anterior eye, is the iris—the coloured part of the eye. The iris is a smooth muscle that opens or closes the pupil, which is the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light.
- The innermost layer of the eye is the neural tunic, or retina, which contains the nervous tissue responsible for photoreception.
The eye is also divided into two cavities:
- The anterior cavity
- The anterior cavity is the space between the cornea and lens, including the iris and ciliary body. It is filled with a watery fluid called the aqueous humor.
- The posterior cavity
- The posterior cavity is the space behind the lens that extends to the posterior side of the interior eyeball, where the retina is located. The posterior cavity is filled with a more viscous fluid called the vitreous humor.
The retina is composed of several layers and contains specialized cells for the initial processing of visual stimuli. The photoreceptors (rods and cones) change their membrane potential when stimulated by light energy. The change in membrane potential alters the amount of neurotransmitter that the photoreceptor cells release onto bipolar cells in the outer synaptic layer. It is the bipolar cell in the retina that connects a photoreceptor to a retinal ganglion cell (RGC) in the inner synaptic layer. There, amacrine cells additionally contribute to retinal processing before an action potential is produced by the RGC. The axons of RGCs, which lie at the innermost layer of the retina, collect at the optic disc and leave the eye at the optic nerve (see Figure 15.5). Because these axons pass through the retina, there are no photoreceptors at the very back of the eye, where the optic nerve begins. This creates a “blind spot” in the retina, and a corresponding blind spot in our visual field.
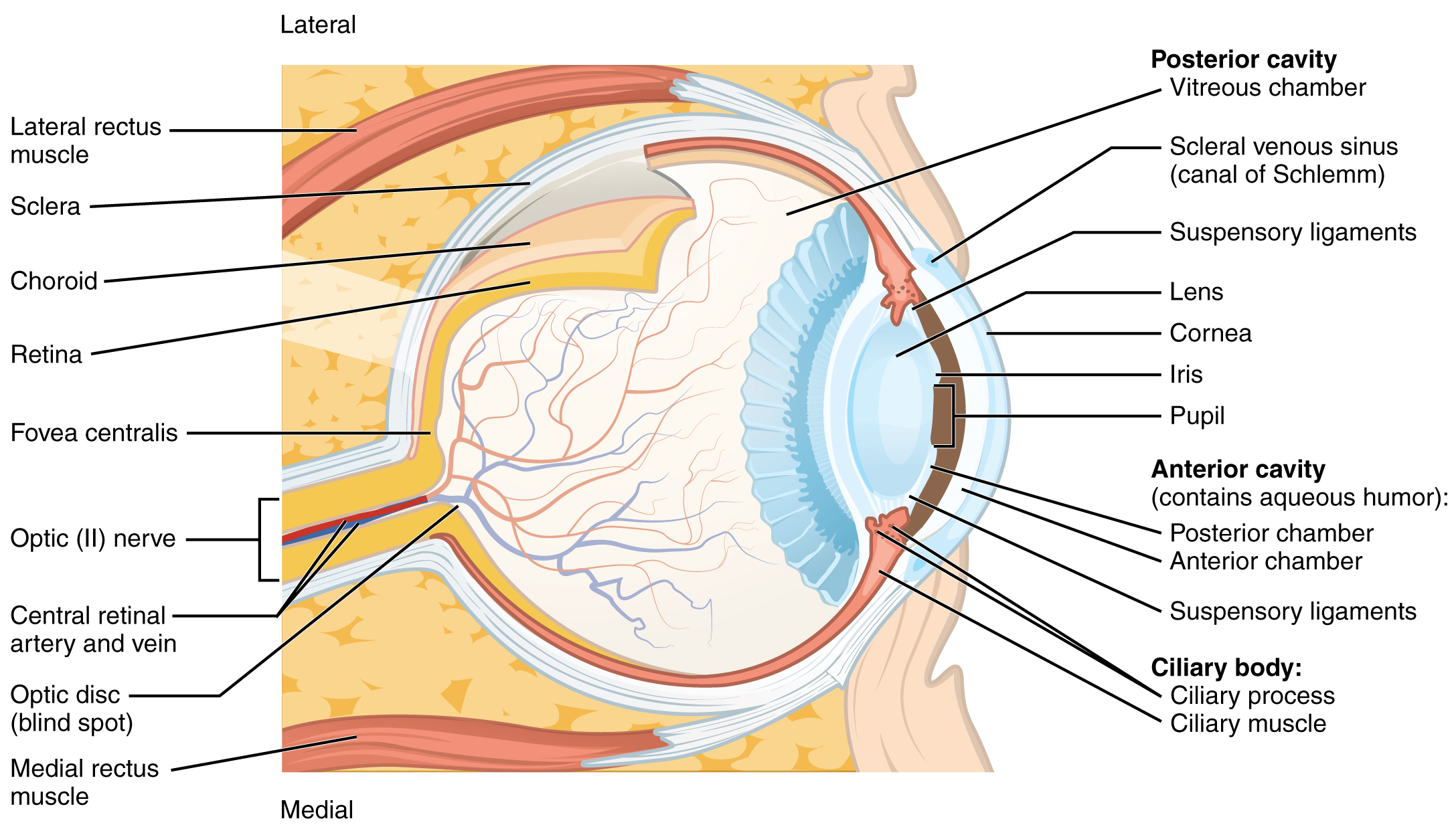
Photoreceptors in the retina (rods and cones) are located behind the axons, RGCs, bipolar cells, and retinal blood vessels. A significant amount of light is absorbed by these structures before the light reaches the photoreceptor cells. At the exact center of the retina is a small area known as the fovea. At the fovea, the retina lacks the supporting cells and blood vessels, and only contains photoreceptors. Therefore, visual acuity, is greatest at the fovea. This is because the fovea is where the least amount of incoming light is absorbed by other retinal structures (see Figure 15.5). As one moves in either direction from this central point of the retina, visual acuity drops significantly.
Example: Visual Acuity (VA) between the fovea and peripheral retina
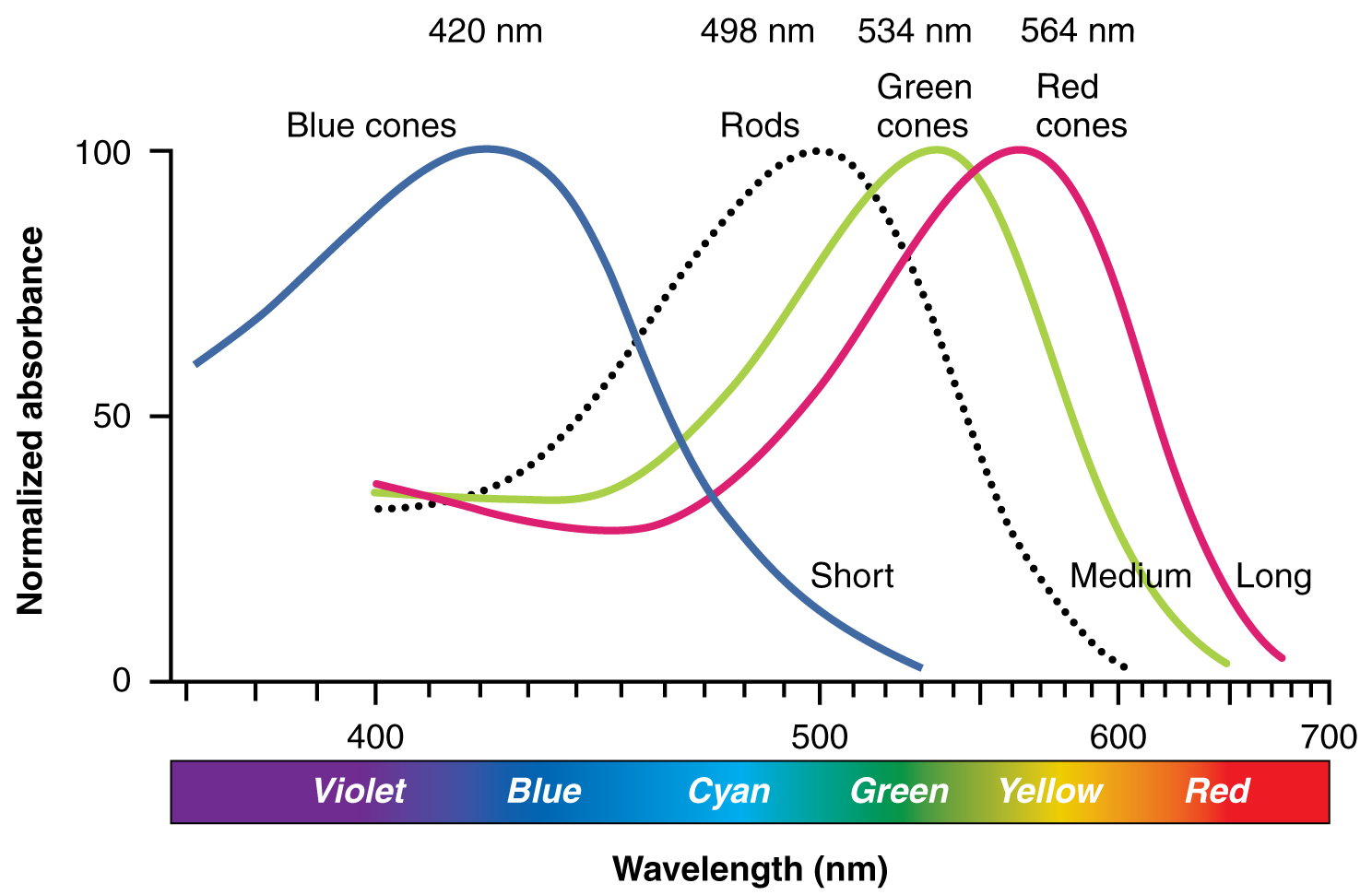
There are three types of cone opsins, that are sensitive to different wavelengths of light and provide us with colour vision. By comparing the activity of the three different cones, the brain can extract colour information from visual stimuli (see Figure 15.6). For example, a bright blue light that has a wavelength of approximately 450 nm would activate the “red” cones minimally, the “green” cones marginally, and the “blue” cones predominantly. The relative activation of the three different cones is calculated by the brain, which perceives the colour as blue. However, cones cannot react to low-intensity light, and rods do not sense the colour of light. Therefore, our low-light vision is, in essence, in grayscale. In other words, in a dark room, everything appears as a shade of gray. If you think that you can see colours in the dark, it is most likely because your brain knows what colour something is and is relying on that memory.
Sensory Systems Medical Terms, Abbreviations and Anatomy
Sensory System Medical Terms
Sensory System Medical Terms (Text Version)
Practice the following sensory system words by breaking into word parts and pronouncing.
- anisocoria (an-ī-sō-KŌR-ē-ă)
- condition of absence of equal pupil (size)
- aphakia (ă-FĀ-kē-ă)
- condition of no lens
- audiogram (OD-ē-ō-gram)
- graphic record (radiographic image) of hearing
- audiologist (od-ē-OL-ŏ-jĭst)
- specialist who studies and treats the hearing
- audiology (od-ē-OL-ŏ-jē)
- study of the hearing
- audiometer (od-ē-OM-ĕt-ĕr)
- instrument used to measure hearing
- audiometry (od-ē-OM-ĕ-trē)
- measuring hearing
- aural (OR-ăl)
- pertaining to the ear
- binocular (bĭn-ŎK-ū-lăr)
- pertaining to both eyes
- blepharitis (blĕf-ăr-Ī-tĭs)
- inflammation of the eyelid
- blepharoplasty (BLĔF-ă-rō-plăs-tē)
- surgical repair of the eyelid
- blepharoptosis (BLĔF-ă-rōp-TŌ-sĭs)
- condition of drooping of the eyelid
- cochlear (KOK-lē-ăr)
- pertaining to the cochlea
- cochlear implant (KOK-lē-ă IM-plant)
- pertaining to the cochlear implant
- conjunctivitis (kŏn-jŭnk-tĭ-VĪT-ĭs)
- inflammation of the conjunctiva
- corneal (KOR-nē-ă)
- pertaining to the cornea
- cryoretinopexy (krī-ō-RET-in-ō-pek-sē)
- surgical fixation of the retina using extreme cold
- dacrocystitis (dak-rē-ŏ-sis-TĪT-ĭs)
- inflammation of the tear (lacrimal) sac
- dacryocystorhinostomy (dak-rē-ŏ-sis-tŏ-rī-NOS-tŏ-mē)
- creation of an artificial opening between the lacrimal sac and the nose
- diplopia (dip-LŌ-pē-ă)
- condition of double vision
- electrocochleography (ē-lek-trō-kok-lē-OG-ră-fē)
- process of recording the electrical activity in the cochlea
- endophthalmitis (ĕn-dŏf-thăl-MĪ-tĭs)
- inflammation within the eye
- intraocular (in-tră-OK-yŭ-lăr)
- pertaining to within the eye
- iridectomy (ir-ĭ-DEK-tŏ-mē)
- excision of (part of) the iris
- iridoplegia (ir-ĭ-dō-PLĒ-j(ē-)ă, īr)
- condition of paralysis of the iris
- iridotomy (ĭr-ĭ-DŎT-ō-mē)
- incision into the iris
- iritis (ī-RĪT-ĭs)
- inflammation of the iris
- isocoria (ī-sō-KŌ-rē-ă)
- condition of equal pupils
- keratitis (ker-ă-TĪT-ĭs)
- inflammation of the cornea
- keratomalacia (kĕr-ă-tō-mă-LĀ-shē-ă)
- softening of the cornea
- keratometer (kĕr-ă-TŎM-ĕ-ter)
- instrument used to measure (the curvature) of the eye
- keratoplasty (KER-ăt-ō-plas-tē)
- surgical repair of the cornea
- labyrinthectomy (lab-ĭ-rin-THEK-tŏ-mē)
- excision of the inner ear (labyrinth)
- labyrinthitis (lab-ĭ-rin-THĪT-ĭs)
- inflammation of the inner ear (labyrinth)
- lacrimal (LAK-rĭ-măl)
- pertaining to the tear duct
- leukocoria (loo-kō-KŎR-ē-ă)
- condition of a white pupil
- mastoidectomy (măs-tŏy-d-ĔK-tō-mē)
- excision of the mastoid bone
- mastoiditis (mas-toyd-ĪT-ĭs)
- inflammation of the mastoid bone
- mastoidotomy (măs-toyd-ŎT-ō-mē)
- incision into the mastoid bone
- myringitis (mĭr-ĭn-JĪ-tĭs)
- inflammation of the tympanic membrane
- myringoplasty (mĭr-ĬN-gō-plăst-ē)
- surgical repair of the tympanic membrane
- myringotomy (mĭr-ĭn-GŎT-ō-mē)
- incision into the tympanic membrane
- nasolacrimal (nā-zō-LAK-rĭ-măl)
- pertaining to the nose and the tear duct
- nasopharyngeal (nā-zō-FAR-in-gēl)
- pertaining to the nose and pharynx (throat)
- oculomycosis (ŏk-ū-lō-mī-KŌ-sĭs)
- abnormal condition of the eye caused by a fungus
- ophthalmalgia (ŏf-thăl-MĂL-jē-ă)
- condition of pain in the eye
- ophthalmic (of-THAL-mik)
- pertaining to the eye
- ophthalmologist (ŏf-thăl-MŎL-ō-jĭst)
- specialist of the eye
- ophthalmology (Ophth) (ŏf-thăl-MŎL-ō-jē)
- study of the eye
- ophthalmopathy (ŏf-thăl-MŎP-ă-thē)
- disease of the eye
- ophthalmoplegia (of-thal-mō-PLĒ-j(ē-)ă)
- condition of paralysis of the eye
- ophthalmoscope (of-THAL-mŏ-skōp)
- instrument used to view the eye
- ophthalmoscopy (of-thal-MOS-kŏ-pē)
- process of viewing the eye
- optic (OP-tik)
- pertaining to vision
- optometry (op-TOM-ĕ-trē)
- measuring vision
- otalgia (ō-TĂL-jē-ă)
- condition of pain in the ear
- otologist ( ō-TŎL-ō-jĭst)
- specialist who studies and treats disorders and diseases of the ear
- otology (ō-TŎL-ō-jē)
- study of the ear
- otomastoiditis (ō-tō-mas-toyd-ĪT-ĭs)
- inflammation of the ear and mastoid bone
- otomycosis (ō-tō-mī-KŌ-sĭs)
- abnormal condition of fungus in the ear
- otopyorrhea (ō-tō-pī-ō-RĒ-ă)
- discharge of pus from the ear
- otorhinolaryngologist (ō-tō-RĪ-nō-lăr-ĭn-GŎL-ō-jĭst)
- specialist or physician who studies and treats disease and disorder of the ears,
- otorrhea (ō-tō-RĒ-ă)
- discharge from the ear
- otosclerosis (ō-tō-sklē-RŌ-sĭs)
- condition of hardening of the ear
- otoscope(Ō-tō-skōp)
- instrument used to view the ear
- otoscopy (ō-TŎS-kō-pē)
- process of viewing the ear
- phacomalacia (făk-ō-mă-LĀ-shē-ă)
- condition of softening of the lens
- photophobia (fō-tō-FŌ-bē-ă)
- condition of sensitivity to light
- pseudophakia (SOOD-ō-FĀ-kē-a)
- condition of fake lens
- pupillary (PŪ-pĭ-lĕr-ē)
- pertaining to pupil
- pupillometer (pū-pĭl-ŎM-ĕ-tĕr)
- instrument used to measure the pupil
- pupilloscope (pū-pĭl-ŎS-kōp)
- instrument used to view the pupil
- retinal (RĔT-ĭ-năl)
- pertaining to the retina
- retinoblastoma (ret-ĭn-ō-blas-TŌ-mă)
- tumour arising from a developing retinal cell
- retinopathy (ret-ĭn-OP-ă-thē)
- disease of the retina
- retinoscopy (ret-ĭn-OS-kŏ-pē)
- process of viewing the retina
- sclerokeratitis (sklĕr-ō-kĕr-ă-TĪ-tĭs)
- inflammation of the sclera and cornea
- scleromalacia (sklĕ-rō-mā-LĀ-sē-ă)
- condition of softening of the sclera
- sclerotomy (sklĕ-ROT-ŏ-mē)
- incision into the sclera
- stapedectomy (stā-pĕ-DEK-tŏ-mē)
- excision of the stapes
- tonometer (tō-NOM-ĕt-ĕr)
- instrument used to measure pressure (within the eye)
- tonometry (tō-NOM-ĕ-trē)
- process of measuring pressure
- tympanometer (tĭm-pă-NŎM-ĕ-tēr)
- instrument used to measure the middle ear
- tympanometry (tĭm-pă-NŎM-ĕ-trē)
- measurement of the tympanic membrane
- tympanoplasty (tĭm-păn-ō-PLĂS-tē)
- membranesurgical repair of the tympanic
- vestibular (ves-TIB-yŭ-lăr)
- pertaining to the vestibule
- vestibulocochlear (ves-tĭ-būl-ō-KŌ-klē-ar)
- vestibul/o/cochle/ar
- pertaining to the vestibule and cochlea
- xerophthalmia (zer-of-THAL-mē-ă)
- xer/ophthalm/ia
- condition of dry eye
Activity source: Sensory System Medical Terms by Kimberlee Carter, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. /Text version added.
Anatomy Labeling Activity
Sensory System Eye Anatomy (Text Version)
Label the diagram with correct words listed below:
- Eyebrow
- Conjunctiva
- Levator palpebrae superioris muscle
- Palpebral conjunctiva
- Cornea
- Eyelashes
- Orbicularis oculi muscle
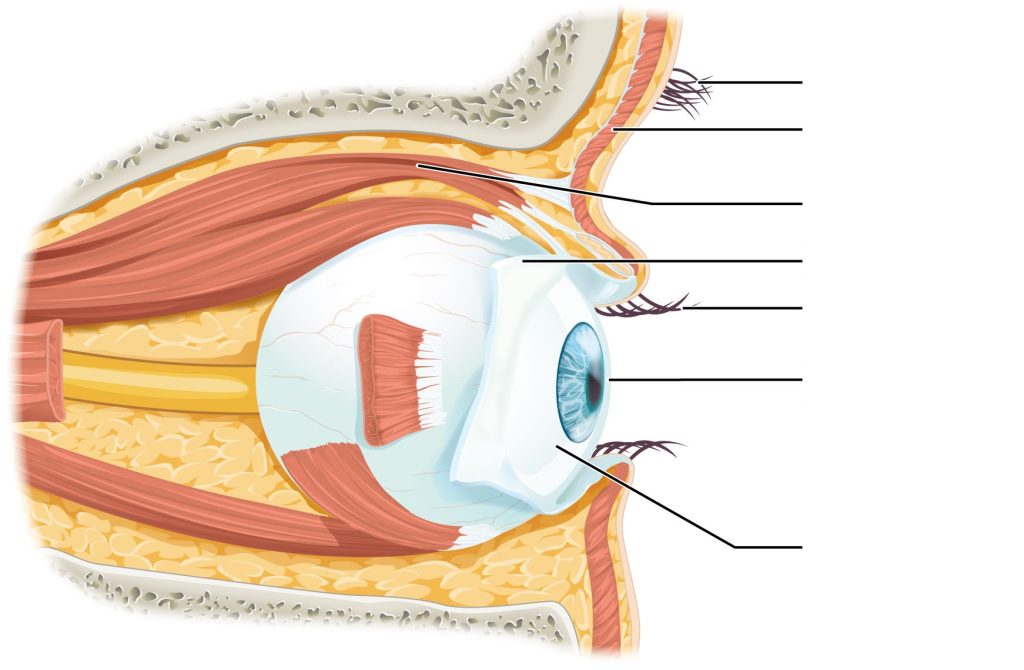
Check your answers [2]
Activity source: Sensory System Eye Anatomy by Gisele Tuzon, from Building a Medical Terminology Foundation, illustration from Anatomy and Physiology (OpenStax), licensed under CC BY 4.0./ Text version added.
Sensory System Eye Anatomy
Sensory System Eye Anatomy (Text Version)
Label the diagram with correct words listed below:
- Fovea centralis
- Suspensory ligaments
- Ciliary muscle
- Retina
- Posterior chamber
- Iris
- Vitreous chamber
- Anterior chamber
- Choroid
- Ciliary process
- Optic disc (blind spot)
- Lens
- Central retinal artery and vein
- Suspensory ligaments
- Lateral rectus muscle
- Optic (II) nerve
- Sclera
- Medial rectus muscle
- Scleral venous sinus (canal of Schlemm)
- Cornea
- Pupil
Sensory System Eye Anatomy Diagram (Text Version)
This diagram shows a lateral and medial view of the eyeball. The major parts are labelled. Labels read from top, clockwise: showing the posterior cavity including the following structures: ______[Blank 1], ______[Blank 2] (canal of Schlemm), ______[Blank 3], _____[Blank 4], ______[Blank 5], _____[Blank 6], and ____[Blank 7]. Next is the anterior cavity (contains aqueous humor), ______[Blank 8], _____[Blank 9], and ______[Blank 10]. The Ciliary body ________[Blank 11] and ________[Blank 12], ______[Blank 13], _____[Blank 14] (blind spot of the eye), ______[Blank 15], _____[Blank 16], _______[Blank 17], ______[Blank 18], ________[Blank 19], and ________[Blank 20].
Check your answers [3]
Activity source: Sensory System Eye Anatomy by Gisele Tuzon, from Building a Medical Terminology Foundation, illustration from Anatomy and Physiology (OpenStax), licensed under CC BY 4.0./ Text version added.
Sensory System Terms Not Easily Broken into Word Parts
Sensory System not easily broken into word parts (Text Version)
- astigmatism (Ast)
- blurry vision due to irregular curvature of the cornea or lens
- Optician
- specialist who fills prescriptions for lenses but cannot prescribe
- anosmia
- condition of being without smell/inability to smell
- stye
- infection of an oil gland of the eyelid (hordeolum)
- amblyopia
- reduced vision in one eye
- associated with strabismus (lazy eye)
- Optometrist
- specialist who diagnoses, treats, and manages diseases and disorders of the eye
- Doctor of Optometry
- visual acuity (VA)
- sharpness or clearness of vision
- cataract
- abnormal progressive disease of lens characterized by lack of transparency or cloudiness
Activity source: Sensory System Terms Not Easily Broken into Word Parts by Kimberlee Carter, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. /Text version added.
Common Abbreviations for the Sensory System
Sensory System Abbreviations
- ARMD (age-related macular degeneration)
- Ast (astigmatism)
- Em (emmetropia)
- IOL (intraocular lens)
- IOP (intraocular pressure)
- LASIK (laser-assisted in situ keratomileusis)
- Ophth (ophthalmology)
- PHACO (phacoemulsification)
- PRK (photorefractive keratectomy)
- VA (visual acuity)
- AOM (acute otitis media)
- ENT (ears, nose, throat)
- EENT (eyes, ears, nose, and throat)
- HOH (hard of hearing)
- OM (otitis media)
Activity source: Sensory System Abbreviation by Kimberlee Carter, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. / Text version.
Image Descriptions
Figure 15.1 image description: This image shows the structure of the ear with the major parts labeled. The ear is divided into 3 parts from left to right: external ear, middle ear, and inner ear. Labels for each part read: external ear (auricle, ear canal), middle ear (tympanic membrane, malleus, incus, tympanic cavity), inner ear (stapes, vestibule, vestibular nerve, cochlear nerve, cochlea, round window, eustachian tube). [Return to Figure 15.1].
Figure 15.2 image description: This diagram shows the structure of the cochlea in the inner ear. Labels read (from top, counterclockwise): bony cochlear wall, scala vestibuli, cochlear duct, tectorial membrane, basilar membrane, scala tympani, spiral ganglion, cochlear branch of N VIII, organ of Corti. [Return to Figure 15.2].
Figure 15.3 image description: The left panel of this image shows a person’s head in a still position. Underneath this, the ampullary nerve is shown. Labels read: cupula, ampulla, ampullary nerve). The right panel shows a person rotating his head, and the below that, the direction of movement of the cupula is shown. Label reads: as the head rotates, cupula bends in opposite direction of the rotation. [Return to Figure 15.3].
Figure 15.4 image description: This diagram shows the lateral view of the eye. The major parts are labeled. Labels read (from top): eyebrow, orbicularis oculi muscle, levator palpebrae superioris muscle, palpebral conjunctiva, eyelashes, cornea, conjunctiva. [Return to Figure 15.4].
Figure 15.5 image description: This diagram shows a lateral and medial view of the eyeball. The major parts are labelled. Labels read (from top, clockwise): posterior cavity (vitreous chamber, scleral venous sinus (canal of Schlemm), suspensory ligaments, lens, cornea, iris, pupil); anterior cavity (contains aqueous humor, posterior chamber, anterior chamber, suspensory ligaments); Ciliary body (ciliary process and muscle), medial rectus muscle, optic disc (blind spot), central retinal artery and vein, foveal centralis, retina, choroid, sclera, lateral rectus muscle. [Return to Figure 15.5].
Figure 15.6 image description: This graph shows the normalized absorbance versus wavelength for different cell types in the eye. The Y-axis is normalized absorbance, and the X axis is wavelength (nm) with the colours violet, blue, cyan, green, yellow, and red across the bottom. The lines in the graph indicate blue cones which peak at 420 nm; rods which peak at 498 nm; green cones, which peak at 534 nm, and red cones which peak at 564 nm. Blue cones line is labelled as short, green cones as medium, and red cones as long. [Return to Figure 15.6].
Attribution
Except where otherwise noted, this chapter is adapted from “Sensory Systems” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Sensory Systems chapter content into sub-chapters.
-
↵
Check your answers: Sensory System Ear Anatomy labeling activity (Text Version)
text -
 ↵
↵ -
↵
Check your answers: Sensory System Eye Anatomy Diagram (Text Version)
This diagram shows a lateral and medial view of the eyeball. The major parts are labelled. Labels read from top, clockwise: showing the posterior cavity including the following structures: vitreous chamber, scleral venous sinus (canal of Schlemm), suspensory ligaments, lens, cornea, iris, and pupil. Next is the anterior cavity (contains aqueous humor), posterior chamber, anterior chamber, and suspensory ligaments. The Ciliary body ciliary process and ciliary muscle, medial rectus muscle, optic disc (blind spot of the eye), central retinal artery and vein, foveal centralis, optic nerve, retina, choroid, sclera, and lateral rectus muscle.
ear drum
balance
body movement
the white of the eye
sharpness of vision

