
In Connection 3, you will learn about cultural safety and furthering your relationship building through respect for Anishinaabe or other Indigenous cultures.
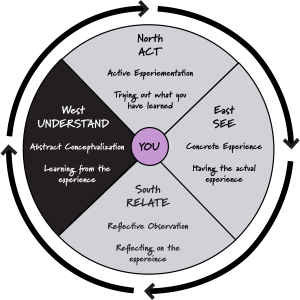
THE WEST: UNDERSTANDING THE THEORY BEHIND THE EXPERIENCE
You will begin Connection 3 in the West where you will learn about and understand the meaning of cultural safety, who defines it, and why it matters when working with Anishinaabeg. Recalling our learning from Module 1, Connection 5, we will examine the impact of colonialism and why this is an important lens for cultural safety. You will conclude this module with a Reflection Checkpoint exercise.
Defining Cultural Safety
“Cultural safety refers to the need for health professionals to consider their own cultural background and the impact of power, privilege and their personal biases on healthcare systems and organizations and the relationships within them. Cultural safety focuses on the [client]. It provides space for [clients] to be involved in decision making about their own care and contribute to the achievement of positive health outcomes and experiences” (Health Navigator, 2022).
Cultural safety refers to what is felt or experienced by a client and only the client can determine when they feel culturally safe when receiving care. This occurs when service providers communicate in respectful, inclusive ways and empower clients in decision-making. It requires building relationships where clients and service providers can work together as a team to ensure better, more equitable care (Health Navigator, 2022).
For deeper understanding, particularly with the Anishinaabeg, one needs to be open to learning about the impact of colonialism, politics both from the past, and the present that lie beneath the health inequities for Indigenous peoples (see Module 1, Connection 5). Of particular importance is that what it means to be culturally safe can only be defined by the client receiving the care. The issue is, as service providers, we all have different understandings, perspectives, and approaches. We began our analysis of our own positionality and wellness stories in Module 2, Connection 2. We also learned about how historical factors such as colonialism affect wellness and how every care provider has a responsibility to address the current health disparities among Indigenous peoples (see Module 1, Connection 5).
When we think about the ideas we have about other people and cultures that differ from ours we should examine where these ideas come from. We might get these ideas from our families, schools, or the media like newspapers, magazines, books, television, or social media. But as we will learn in Module 2, Connection 3, cultural safety is about challenging and interrogating certain narratives to create better relationships with clients. If we think about ideas as the seeds that we cultivate to build better relationships with Indigenous peoples, we can instill change in those ideas. We know that not all ideas are beneficial, and some can be harmful and may stem from racism.
Review the three types of racism identified by Dr. Anderson-DeCoteau in Module 1, Connection 2![]() :
:
Health Literacy – Indigenous Perspectives on Health and Well-Being
In this video [4:09] Regional Aboriginal Cancer Lead, Dr. Bernice Downey, and former Aboriginal navigator, Joanna Vautour describe their roles in the western healthcare system, and share the importance of health literacy and communication for Indigenous patients and families.
Video Transcript: Health Literacy – Indigenous Perspectives on Health and Well-Being [Doc]![]()
Key Messages from the Video
- It is important to understand cultural safety for working with Indigenous populations
- Cultural safety can mean empowering a person and engaging in a “therapeutic relational space with an individual” so that Indigenous clients can have “personal agency” for their health care (Cancer Care Ontario, 2018).
- Clients should feel empowered to ask questions, and all their questions are important
- Indigenous perspectives are important to delivering positive health messages to clients in a culturally appropriate and safe manner
Checkpoint 3: Delivering Positive Health Messages
After watching the video, consider one way that this video matters to your emerging perspective on how to build relationships with Indigenous peoples?
Answer by either recording yourself speaking or by taking notes. Be sure to download a copy of your audio clip or notes before proceeding on.
The Cultural Safety Continuum
In the following section, you will gain an understanding of the cultural safety continuum using a metaphor of how a tree grows.
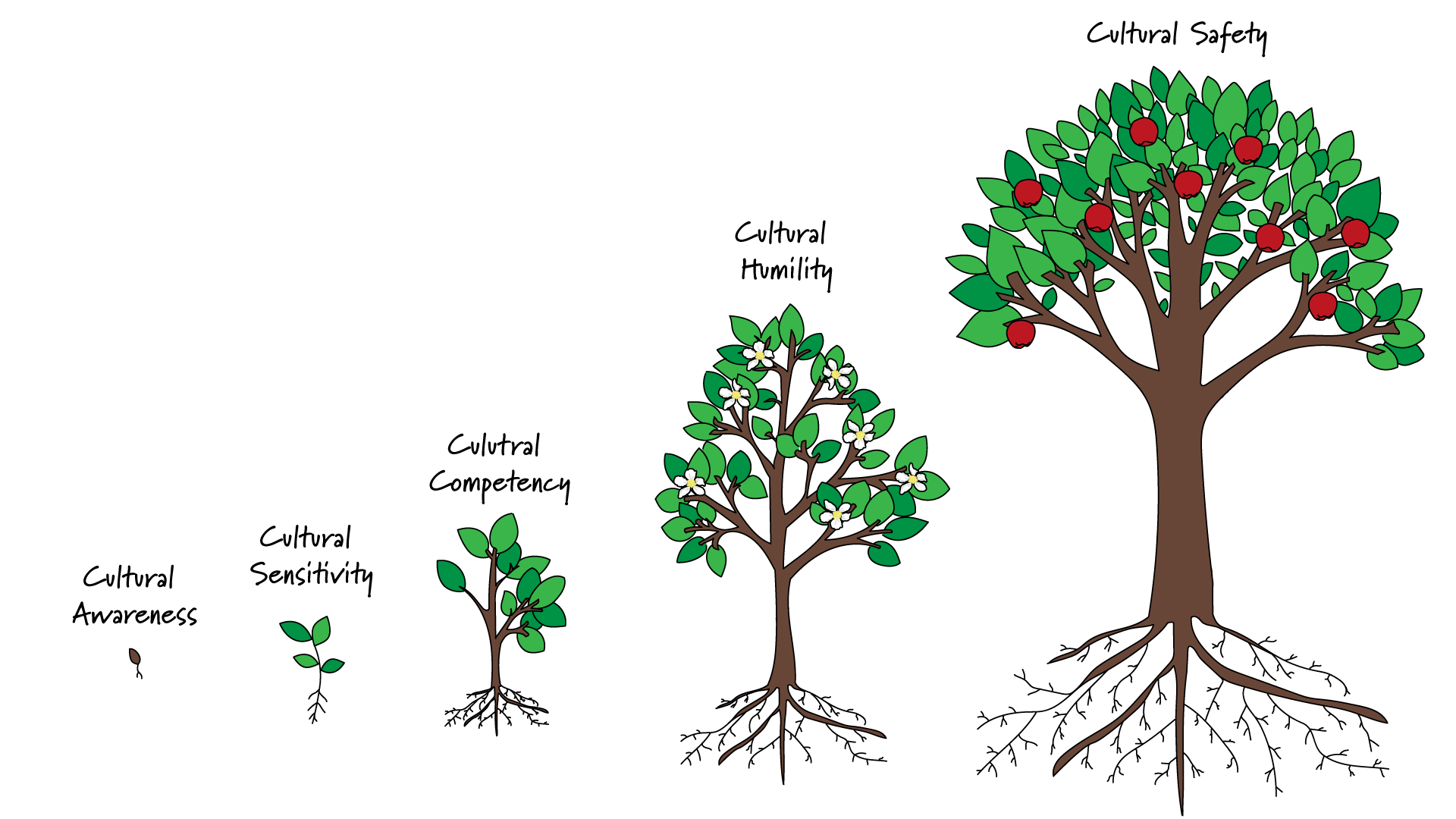
Image Description: Cultural Safety Continuum [Doc]
 The Seedling – Cultural Awareness
The Seedling – Cultural Awareness
This continuum begins with cultural awareness. Cultural awareness is the seedling that begins the process for realizing cultural safety. It requires a person to notice what is common and different amongst and across cultures. One must be critical when noticing differences as they do not necessarily mean deficits. Remember, that perspectives emerge from our positionality. To become culturally aware means learning about the true history of Indigenous peoples in Canada and recognizing the impact of the colonial narrative (Northern Health, 2022).
 The Sprout – Cultural Sensitivity
The Sprout – Cultural Sensitivity
For trees to sprout they need help from elements like water, nutrients, and the sun, to thrive and grow. Likewise, cultural sensitivity grows when we notice how our own culture and biases may have an influence on persons from other cultures. We consider the biases we hold because of our beliefs, values, and lifestyles. Truth and honesty require both courage and humility. This growing awareness brings forth the responsibility to be respectful of others (Northern Health, 2022).
 The Young Tree – Cultural Competency
The Young Tree – Cultural Competency
When a tree matures and its root system is established, it can sustain itself. When we become aware of the impact of our own culture on others, cultural competency is initiated where practical skills in acting respectfully with others is sustained. Being culturally competent is not about becoming experts in another’s culture – rather it’s knowing how one’s culture may impact another person and understanding what it means to act respectfully. It is also about making room or empowering a person to integrate their own cultural practices in the healing process (Northern Health, 2022).
 The Blooming Mature Tree – Cultural Humility
The Blooming Mature Tree – Cultural Humility
Once a tree has grown, it bears fruit for regeneration. The blossoms are a sign that fruit is about to grow. In this continuum, cultural humility emerges when a person realizes and grows into a reflective and relational practitioner who practices the skills of self-evaluation and reflection to achieve a state of understanding how one’s experience impact and influence others. This is a lifelong journey and involves being non-judgmental and is foundational for cultural safety (Northern Health, 2022).
 The Mature Tree with Fruit – Cultural Safety
The Mature Tree with Fruit – Cultural Safety
In this metaphor, cultural safety is the state where the tree is established and grows to bear edible fruit and all people feel respected and safe from racism and discrimination as they interact with one another. Cultural safety grows when “people are supported to draw strengths from their identity, culture, and community” (Northern Health, 2022).
Service providers who understand the impacts of colonialism are foundational to achieving health equity. Health equity also requires structural intervention and is the responsibility of service providers who hold power.
The outcome of cultural safety is client satisfaction. To be respected for one’s uniqueness and individuality honours dignity and personhood while celebrating the gifts that everyone offers. Collaboratively, we may benefit from working together towards the utmost healing for the client.
The suggestions put forth by Interior Health (2019) below provide service providers with ideas on how to nurture cultural safety:
Key Components of Cultural Safety in Practice
- Educate oneself on the ‘colonial narrative’
- Be reflective of situations and of self
- Be mindful of the power imbalances in a health care interaction
- Acknowledging that cultural safety is defined by the Indigenous recipient of care
- Be committed to life-long and ongoing learning
(Interior Health, 2019).
Examples of Cultural Safety in Practice
- Respectfully ask about self-identification
- Develop care plans which meaningfully integrate Indigenous peoples’ cultural and wellness preferences
- Ensure that all Indigenous [clients] and their families feel welcomed, supported, and validated during their care journey
- Ensure that [clients] have access to spiritual care, ceremony, and cultural support
- Ensure that co-workers have information about cultural safety
- Acknowledge the ‘colonial narrative’ and its effects on the health and wellness of Indigenous peoples
(Interior Health, 2019).
How to Stand Up to Culturally Unsafe Situations
- Notice how implicit biases may lead to harm of others
- Be courageous to stand up for what is right and intervene through respectful dialogue
- When speaking to someone about implicit biases choose an appropriate environment to have an assertive and respectful dialogue that promotes deeper discussion
- Be gentle and welcome dialogue
- Challenge and deconstruct negative stereotypes to move deeper into what was communicated
- Report culturally unsafe encounters to your manager
- Engage in debriefing with your supervisor or colleagues
(Interior Health, 2019).
Checkpoint 4: Your Commitment to Cultural Safety
Now that you have begun on your path towards cultural safety, reflect on these questions.
- Are you willing to engage in reflecting on your own assumptions to become aware about how this influences the care you provide?
- Are you willing to become aware of this to understand how you can create a relationally and respectful space for others?
Your Commitment to Cultural Safety
When you have finished reflecting on the questions posed above, you are encouraged to complete the commitment card below.
Connection 3 Summary
In Connection 3, we learned:
- Cultural safety refers to what is felt or experienced by a client where the outcome is client satisfaction with the care or services provided
- Cultural safety is about challenging and interrogating certain narratives to create better relationships with clients
- Cultural safety involves a journey along a continuum of understanding and represents a lifelong journey rather than an endpoint

To move on to the Module 2 Finish Point, click on the “Next: Finish Point: Acting on your learning through a learning scenario →” button at the bottom right hand corner of this page.
References
Cancer Care Ontario. (2018, September 27). Health literacy – Indigenous perspectives on health and well-being [Video]. YouTube. https://youtu.be/8M5mG4btiFo![]()
First Nations Health Authority. (2022). “My commitment to cultural safety & humility” pledge card. https://www.fnha.ca/Documents/FNHA-Cultural-Humility-Pledge-Card.pdf![]()
Health Navigator, New Zealand. (2022). Cultural safety. Health Navigator NZ. https://www.healthnavigator.org.nz/clinicians/c/cultural-safety/![]()
Interior Health. (2019, April 15). Aboriginal cultural safety: Cultural safety in practice – How to be an ally [Video]. YouTube. https://youtu.be/cLDkA2RIeCM![]()
Northern Health Indigenous Health. (2022). Cultural safety: Supporting increased cultural competency and safety throughout Northern health. https://www.indigenoushealthnh.ca/cultural-safety![]()
TEDx UManitoba. (2016, April 13).Marcia Anderson-DeCouteau: Indigenous knowledge to close gaps in Indigenous health [Video] YouTube. https://www.youtube.com/watch?v=IpKjtujtEYI![]()

