This post is adapted for the Health & Medical Case Studies created by the Master of Medical Biotechnology program of the University of Windsor. This work licensed under a Creative Commons Attribution-NonCommercial (CC BY-NC-ND) 4.0 International License.
11 Case 4-2020: A 65-year-old woman chest tightness, nausea, vomiting during bronchoscopy
Diagnosis and prognosis of myocardial infarction in a patient without obstructive coronary artery disease during bronchoscopy: a case study and literature review. BMC Cardiovasc Disord 20, 185 (2020). https://doi.org/10.1186/s12872-020-01458-5
Li, M., Liu, Y. & Wang, H.
Case Summary 1
A 65-year-old woman was hospitalized with the main complaint of chest tightness, nausea, and vomiting for 30 min during bronchoscopy under local anesthesia. Immediate electrocardiogram (ECG) showed ST-segments elevation in leads V2–6 compared with those at admission, and the further evolvement of leads V2–3 into pathological Q wave. Serum cardiac biomarkers revealed an increase of high-sensitive cardiac troponin T (hs-cTnT) levels. Emergency coronary angiography (CAG) showed only approximately 30% stenosis in the left anterior descending (LAD) ostium and 40% stenosis in the first diagonal branch(D1), with a quantitative flow ratio (QFR) value for LAD of 0.96. Moreover, her echocardiographic examination presented new significant abnormal wall motion (anterior ventricular wall) with an estimated left ventricular ejection fraction (LVEF) of 62.1% after the cardiac attack. Thoracic enhanced CT scanning indicated no obvious sign of pulmonary embolism. This patient was diagnosed with MINOCA (Myocardial infarction with nonobstructive coronary arteries) based on her atypical angina symptoms, dynamic changes of ECGs, and elevated cardiac biomarker with CAG revealing no significant obstruction of coronary arteries. She was treated accordingly and had a good prognosis during a 14-month follow-up.
Learning Objectives
- Understanding emergency cardiac conditions.
- Investigating cardiac cases based on the patient’s history and presenting symptoms.
- Determine the required lab investigations and their role in the diagnosis.
- Familiarizing and defining new medical terminology associated with the disease.
Clinical History 1
- Age: 65 years old
- Sex: Female
- Ethnicity: Not mentioned.
Medical History 1
- The patient underwent right upper lung adenocarcinoma resection 4 months back and was found to have an elevated carcinoembryonic antigen (CEA), 2 days before admission. A bronchoscopy examination was scheduled to determine local recurrence.
- History of hypertension for 1 year but no history of taking any anti-hypertensive medication.
- No history of other chronic diseases such as diabetes, coronary artery disease (CAD), or stroke, and no history of cigarettes, alcohol, or substance abuse.
Symptoms 1
- Sudden onset of chest tightness, nausea, and vomiting for half an hour during the scheduled bronchoscopy procedure.
Examinations (Clinical Assays/Tests/Imaging) 1
Physical Examination 1
- Blood pressure: 166/94 mmHg
- BMI: 22.73 kg/m2 (normal)
Laboratory Investigations 1
|
Investigation name |
Result |
Reference range |
|
High-sensitive cardiac troponin T (hs-cTnT) |
20.12 ng/L and 674.6 ng/L at the peak |
0-14 ng/L |
|
Total cholesterol |
6.70 mmol/L |
3.00–5.70 mmol/L |
|
Low-density-lipoprotein cholesterol (LDL-C) |
4.18 mmol/L
|
2.60–4.10 mmol/L |
|
Routine complete blood count, urine test, glucose levels, renal and liver function, coagulation factors, hemoglobin A1c, thyroid function and autoimmune indicators were within the normal ranges. |
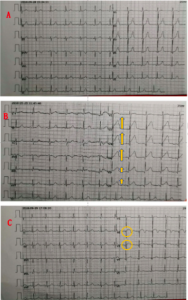
Immediate Electrocardiogram 1
- Showed ST-segments elevation in leads V2–6 compared with those at admission, then the further evolvement of leads V2–3 into pathological Q wave.
Thoracic Enhanced Computed Tomography (CT) Scan 1
- No obvious sign of pulmonary embolism.
- New significant abnormal wall motion (anterior ventricular wall) with an estimated left ventricular ejection fraction (LVEF) of 62.1%.
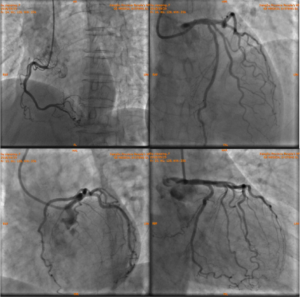
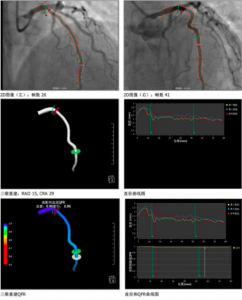
Emergency CAG (Coronary Angiography)1
- Approximate 30% stenosis in the left anterior descending (LAD) ostium and 40% stenosis in the first diagonal branch, functional quantitative flow ratio (QFR) value for LAD was 0.96.
Question & Answers Leading to Diagnosis:
Question 1: Based on clinical history and lab investigations result what diagnosis can we make for this patient?
Question 2: What does the ST elevation in ECG indicate?
Question 3: Based on the symptoms present, how can we recognize emergency cardiac conditions?
** For answers please check the next chapter.
Medical terminology/Abbreviations:
- Adenocarcinoma – Adenocarcinoma is a type of cancer that starts in mucus-producing glandular cells of the body.5
- Bronchoscopy – Bronchoscopy is a procedure that looks inside the lung airways. It can detect tumors, signs of infection, excess mucus in the airways, bleeding, or blockages in the lungs.7
- CEA – A carcinoembryonic antigen (CEA) test is a blood test used to help diagnose and manage certain types of cancers.6
- Coronary Angiography – Coronary angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the arteries in the heart.11
- ECG – An electrocardiogram or ECG is a test to record the electrical signals in the heart.9
- Echocardiogram – An echocardiogram (echo) is a graphic outline of the heart’s movement done by ultrasound.10
- High-sensitive cardiac troponin T – Cardiac troponin is the preferred biomarker for the diagnosis of acute myocardial infarction and high-sensitive cardiac troponin T (hs-cTnT) assay permits detection of very low levels of cTnT.8
- MINOCA – Myocardial infarction with nonobstructive coronary arteries (MINOCA) is clinically defined by the presence of the universal acute myocardial infarction (AMI) criteria, absence of obstructive coronary artery disease (≥50% stenosis), and no overt cause for the clinical presentation at the time of angiography.2
References
- Li, M., Liu, Y. & Wang, H. (2020). Diagnosis and prognosis of myocardial infarction in a patient without obstructive coronary artery disease during bronchoscopy: a case study and literature review. BMC Cardiovasc Disord 20, 185. https://doi.org/10.1186/s12872-020-01458-5
- Pasupathy, S. Tavella, R. & Beltrame, J. F. (2017). Myocardial Infarction With Nonobstructive Coronary Arteries (MINOCA)The Past, Present, and Future Management. Circulation, 135(16), 1490-1493. https://doi.org/10.1161/CIRCULATIONAHA.117.027666
- What is a STEMI? (2015, June 24). ECG Medical Training. Retrieved March 16, 2021, from https://www.ecgmedicaltraining.com/what-is-a-stemi/
- Signs of a heart attack. (n.d.). Heart & Stroke. Retrieved March 16, 2021, from https://www.heartandstroke.ca/heart-disease/emergency-signs
- Moyer, N. (2019, January 25). Adenocarcinoma Symptoms: Learn Symptoms of the Most Common Cancers. Healthline. Retrieved March 16, 2021, from https://www.healthline.com/health/cancer/adenocarcinoma-symptoms#symptoms
- Cafasso, J. (2020, April 1). Carcinoembryonic Antigen Test (CEA). Healthline. Retrieved March 16, 2021, from https://www.healthline.com/health/cea
- Bronchoscopy. (n.d.). National Heart, Lung and Blood Institute. Retrieved March 16, 2021, from https://www.nhlbi.nih.gov/health-topics/bronchoscopy
- Xu, R., Zhu, X., Yang, Y., Ye, P. (2013). High-sensitive cardiac troponin T. J Geriatr Cardiol, 10(1): 102–109. doi: 10.3969/j.issn.1671-5411.2013.01.015
- Electrocardiogram (ECG or EKG). (n.d.). Mayoclinic. Retrieved March 16, 2021, from https://www.mayoclinic.org/tests-procedures/ekg/about/pac-20384983
- Echocardiogram. (n.d.). Cleveland Clinic. Retrieved March 16, 2021, from https://my.clevelandclinic.org/health/diagnostics/16947-echocardiogram#:~:text=An%20echocardiogram%20(echo)%20is%20a,pumping%20action%20of%20the%20heart
- Coronary angiography. (n.d.). Medine Plus. Retrieved March 16, 2021, from https://medlineplus.gov/ency/article/003876.htm
- Mendis, S., Thygesen, K., Kuulasmaa, K., Giampaoli, S., Mahonen, M., Ngu Blackett, K., & Lisheng, L. (2010). World Health Organization definition of myocardial infarction: 2008-09 revision. International Journal Of Epidemiology, 40(1), 139-146. https://doi.org/10.1093/ije/dyq165
- What is a STEMI? – ECG Medical Training. ECG Medical Training. (2021). Retrieved 28 May 2021, from https://www.ecgmedicaltraining.com/what-is-a-stemi/.
- Graphix, i. (2021). ECG 12-lead BASIC. The Resuscitation Group. Retrieved 28 May 2021, from https://www.resuscitationgroup.com/classes/ecg-basic/.
Creative Commons License
Bronchoscopy is a procedure that looks inside the lung airways. It can detect tumors, signs of infection, excess mucus in the airways, bleeding, or blockages in the lungs
An electrocardiogram or ECG is a test to record the electrical signals in the heart.
Cardiac troponin is the preferred biomarker for the diagnosis of acute myocardial infarction and high-sensitive cardiac troponin T (hs-cTnT) assay permits detection of very low levels of cTnT.
Coronary angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the arteries in the heart.
Myocardial infarction with nonobstructive coronary arteries (MINOCA) is clinically defined by the presence of the universal acute myocardial infarction (AMI) criteria, absence of obstructive coronary artery disease (≥50% stenosis), and no overt cause for the clinical presentation at the time of angiography.
Adenocarcinoma is a type of cancer that starts in mucus-producing glandular cells of the body.
A carcinoembryonic antigen (CEA) test is a blood test used to help diagnose and manage certain types of cancers.
An echocardiogram (echo) is a graphic outline of the heart's movement done by ultrasound.
An opening into a vessel or cavity of the body.


