This post is adapted for the Health & Medical Case Studies created by the Master of Medical Biotechnology program of the University of Windsor. This work licensed under a Creative Commons Attribution-NonCommercial (CC BY-NC-ND) 4.0 International License.
23 Case 2-2018: A 78-year-old female with anemia and purple blotches in oral cavity
A case of acquired hemophilia A in an elderly female. Journal of community hospital internal medicine perspectives,2018, 8(4), 237-240. doi: 10.1080/20009666.2018.1487246
Kaur, K. & Kalla, A.
Case Summary 1
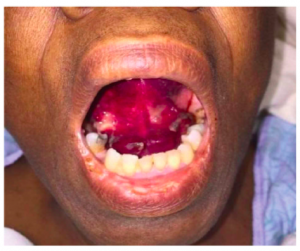
A 78-year-old African American woman presented with gradually worsening anemia with slurred speech, dysphagia, odynophagia with purple blotches in her oral cavity. She gave a history of recurrent GI bleeding and spontaneous bruising in her body. She underwent endoscopies twice revealing a bleeding gastric ulcer. On physical examination, multiple ecchymoses (bruising) were found in her mouth, chest, and extremities. Laboratory investigations revealed a very low Hb level (6.7 g/dl), prolonged aPTT (Activated partial thromboplastin time), and low activity of factor VIII. She was treated according to the diagnosis and her condition gradually improved which reflected as normal aPTT, stable hemoglobin (10.7 g/dL) after 6 months of treatment.
Learning Objectives
- Identify the clinical features of bleeding disorders.
- Describe the confirmatory tests for bleeding disorders.
- Discuss the outcome and prognosis of the treatment.
- Familiarizing and defining new medical terminology associated with bleeding disorders.
Clinical History 1
- Age: 78 years old
- Sex: Female
- Ethnicity: African American
Medical History 1
- History of two endoscopies that revealed bleeding gastric ulcer both times and treatment was done during the endoscopies.
- She also described having multiple spontaneous bruises and ecchymosis sporadically throughout her body over past few months.
- In addition to recurrent GI bleeding, past medical history was significant for chronic iron deficiency anemia, type 2 diabetes mellitus and multinodular goiter requiring thyroidectomy.
- She denied any history of a bleeding diathesis in the family.
- No history of heparin administration.
Symptoms 1
- Slurred speech for 2 days which was suspected as stroke.
- She also complained of dysphagia, odynophagia, and having purple blotches inside her oral cavity.
- She also developed worsening anemia for the past few months and had needed three blood transfusions for symptomatic anemia within the past 2 months.
Examinations (Clinical Assays/Tests/Imaging) 1
Physical Examination 1
- The patient was hemodynamically stable.
- A large ecchymosis was found along the floor of the mouth, as well as on the ventral tongue, and the rest of the buccal mucosa was normal.
- Presence of multiple ecchymoses over the chest and upper extremities.
Laboratory Investigations 1
|
Investigation Name1 |
Result1 |
Reference Range1 |
|
Hemoglobin |
6.7 g/dL |
12.0-15.5 g/dL |
|
aPTT |
35-48 s |
20-28s |
|
Normal |
11.0-12.5s |
|
|
Factor VIII activity |
<1% |
50-150% |
|
Factor VIII inhibitor level |
59.7 Bethesda units |
</ = 0.50 |
|
Factor IX level |
201% |
78–184% |
|
von Willebrand Factor |
256% |
52–214% |
Question & Answers Leading to Diagnosis:
Question 1: Based on the clinical history and lab investigations, what diagnosis is suspected and why?
Question 2: What is the possible cause(s) of low hemoglobin in this patient?
Question 3: What are the manifestations of bleeding disorder?
** For answers please check the next chapter.
Medical terminology/Abbreviations:
- Ecchymosis – Medical term for common bruise caused by the impact of an injury.3
- Endoscopy – An endoscopy is a procedure in which your doctor uses specialized instruments to view and operate on the internal organs and vessels of your body.4
- Bleeding diathesis – In medicine (hematology), bleeding diathesis is an unusual susceptibility to bleed (hemorrhage) mostly due to hypocoagulability (a condition of irregular and slow blood clotting), in turn, caused by a coagulopathy (a defect in the system of coagulation).
- Dysphagia – Difficulty in swallowing. 5
- Odynophagia – Painful swallowing.6
- APTT or PTT – The partial thromboplastin time (PTT; also known as activated partial thromboplastin time (aPTT)) is a screening test that helps evaluate a person’s ability to appropriately form blood clots.7
- PT – Prothrombin time, a test to evaluate blood clotting.8
- Acquired Hemophilia A – Acquired Hemophilia A (AHA) is a rare bleeding disorder related to the formation of autoantibodies to Factor VIII.1
References
- Kaur, K. & Kalla, A. (2018). A case of acquired hemophilia A in an elderly female. Journal of community hospital internal medicine perspectives, 8(4), 237-240. doi: 10.1080/20009666.2018.1487246
- Bleeding Disorders. (n.d.). American Society of Hematology. Retrieved 16 March 2021, from https://www.hematology.org/education/patients/bleeding-disorders
- Osborn, C. O. (2018, September 18). Understanding Ecchymosis. Healthline. Retrieved 16 March 2021, from https://www.healthline.com/health/ecchymosis
- Krans, B. (2018, October 12). Endoscopy. Healthline. Retrieved 16 March 2021, from https://www.healthline.com/health/endoscopy
- Dysphagia. (n.d.). Mayoclinic. Retrieved 16 March 2021, from https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
- Smith, A. (2018, January 31). Odynophagia: Symptoms, causes
- Partial Thromboplastin Time (PTT, aPTT) | Lab Tests Online. Labtestsonline.org. (2021). Retrieved 14 May 2021, from https://labtestsonline.org/tests/partial-thromboplastin-time-ptt-aptt
- Prothrombin time test – Mayo Clinic. Mayoclinic.org. (2021). Retrieved 14 May 2021, from https://www.mayoclinic.org/tests-procedures/prothrombin-time/about/pac-20384661.
Creative Commons License
Difficulty in swallowing.
Painful swallowing.
The partial thromboplastin time (PTT; also known as activated partial thromboplastin time (aPTT)) is a screening test that helps evaluate a person's ability to appropriately form blood clots.
Medical term for common bruise caused by the impact of an injury.
In medicine (hematology), bleeding diathesis is an unusual susceptibility to bleed (hemorrhage) mostly due to hypocoagulability (a condition of irregular and slow blood clotting), in turn, caused by a coagulopathy (a defect in the system of coagulation).
Prothrombin time, a test to evaluate blood clotting.


