This post is adapted for the Health & Medical Case Studies created by the Master of Medical Biotechnology program of the University of Windsor. This work is licensed under a Creative Commons Attribution-NonCommercial (CC BY-NC-ND) 4.0 International License.
37 Case 1-2020: A 29-year-old male with high grade fever
Value of dynamic plasma cell-free DNA monitoring in septic shock syndrome: A case report. World Journal of Clinical Cases. 2020;8(1):200-207.
Liu J, Zhang S, Pan S.
Case Summary 1
A 29-year-old male was brought to the hospital with a history of high fever, gum pain, and swelling for 1 day along with intermittent upper abdominal pain, nausea, and retching. His physical examination revealed a temperature of 39.8 °C, very low BP (80/50mmHg), rapid pulse rate (130 beats/min), and abdominal palpation manifested tender right upper abdomen with positive Murphy’s sign and liver percussion pain. Laboratory investigation showed signs of sepsis in CBC with elevated CRP, liver enzymes, procalcitonin, and metabolic acidosis with hypokalemia and hypocalcemia. Blood culture was positive for Gram-negative bacilli. An abdominal CT scan revealed liver and gall bladder involvement with cardiac dysfunction and pulmonary edema. The patient was treated in ICU and initial investigations were repeated for monitoring purposes. Cell-free DNA (CfDNA) level was also measured as a marker of sepsis. Unfortunately, the patient expired on the 9th day of his admission due to septic shock.
Learning Objectives
- Identifying the signs of suspected septic shock.
- Recognize the clinical and laboratory findings associated with sepsis.
- Understand the rationale of newer biomarkers such as the cfDNA test (cell free DNA).
- Familiarizing and defining new medical terminology associated with septic shock.
Clinical History 1
- Age: 29 years old
- Sex: Male
Medical History 1
- History of a left lateral malleolus fracture subluxation 6 years ago.
- Allergies to penicillin and amoxicillin.
- No history of smoking, drinking, hyperlipemia, and chronic diseases, such as coronary heart disease, hypertension and diabetes.
Drug History 1
- Not applicable.
Symptoms 1
- Pain and bilateral gum swelling for 1 day.
- Sudden chill and a high fever with a peak of 39.8 °C on the morning of admission on July 27, 2017.
- Also presented intermittent right upper quadrant pain, accompanied by nausea and retching.
Examinations (Clinical Assays/Tests/Imaging) 1
Physical Examination 1
- Temperature: 39.8 °C
- Blood pressure: 80/50 mmHg
- Pulse: 130 beats/min.
- On abdominal examination:
- Prominent right upper abdomen which was tender at palpation without guarding and rebound tenderness.
- Presence of positive Murphy’s sign and liver percussion pain.
Laboratory Investigations 1
- Laboratory tests showed leukocytopenia (2.38 × 109/L), a high percentage of neutrophils (83.2%), mild thrombocytopenia (68 × 109/L), abnormal blood coagulation function, a reduced international normalized ratio, hypokalemia, hyperbilirubinemia, elevated liver enzymes (both hepatocellular and cholestatic enzymes), an elevated procalcitonin (PCT) concentration (35.30 ng/mL), metabolic acidosis, and hyperlactatemia, suggesting progressive sepsis.
Chart 1: Laboratory parameters1

Microscopic Examinations 1
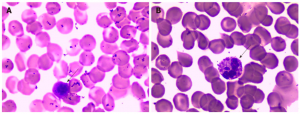
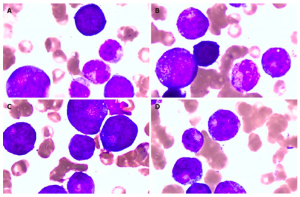
- On light microscopy, the peripheral blood smear showed a left shift of neutrophil nuclei, prominent toxic granulations and vacuolation in the neutrophil cytoplasm (Figure 1).
- Gram-negative bacilli were isolated from blood cultures.
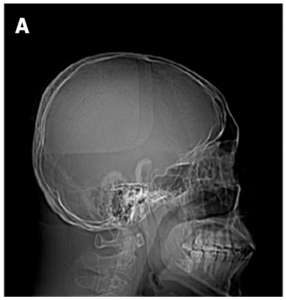
Head Computed Tomography (CT) Scan 1
- No abnormality was reported.
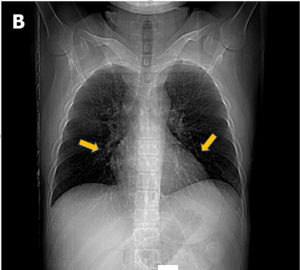
Chest Computed Tomography (CT) Scan 1
- Showed little interstitial change in the lower lung. (yellow arrows pointing to the lower lung).
Abdominal Computed Tomography (CT) Scan 1
- Scanning of the abdomen showed gallbladder wall edema with increased gallbladder density, swelling of the kidneys, and an enlarged pancreas. There was interlobular septal thickening on both sides and bilateral pleural effusion with lower lung insufficiency of both longs, suggesting cardiac dysfunction with pulmonary edema.
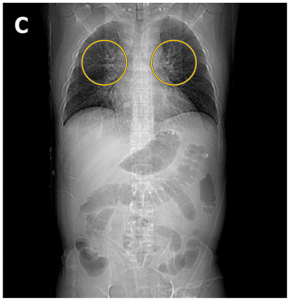
Figure 4: C. An abdominal CT scan suggested cardiac dysfunction with pulmonary edema.1 (Yellow circle showing batwing sign of pulmonary edema.6)
Plasma Cell-Free DNA Levels 1
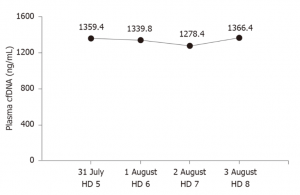
- cfDNA levels were measured by a duplex real-time PCR assay with internal control, which was developed as a novel method for the accurate quantification of plasma cfDNA. Within the 95% confidence interval, the normal reference intervals were 0-52.5 ng/mL for males and 0-45.8 ng/mL for females. However, plasma cfDNA levels were constantly high, peaking at 1366.40 ng/mL (Figure 5).
Peripheral Blood Smear and Bone Marrow Examination 1
- On the 7th day, Peripheral blood and bone marrow examinations showed granulocyte maturation disorders, which may have been caused by infection (figure 6).
Question & Answers Leading to Diagnosis:
Question 1: Based on chief complaints, medical history, physical examination, what initial diagnosis can we suspect?
Question 2: Which lab investigations should be done to confirm the diagnosis and what finding are confirmatory to reach the final diagnosis in this case study?
Question 3: What investigations can be suggested to monitor the condition of this patient? Is there any specific biomarker which can be useful in this regard?
** For answers please check the next chapter.
Medical terminology/Abbreviations:
- Murphy’s sign – Murphy’s sign is elicited in patients with acute cholecystitis by asking the patient to take in and hold a deep breath while palpating the right subcostal area. If pain occurs on inspiration, when the inflamed gallbladder meets the examiner’s hand, Murphy’s sign is positive.2 A positive Murphy’s sign is seen in acute cholecystitis.
- Procalcitonin – Procalcitonin is a substance produced by many types of cells in the body, often in response to bacterial infections but also in response to tissue injury. The level of procalcitonin in the blood can increase significantly in systemic bacterial infections and sepsis. This test measures the level of procalcitonin in the blood.3
- Toxic granulations – Toxic granulations are purple or dark-blue staining azurophilic granules in the cytoplasm of neutrophils, bands, and metamyelocytes resulting from an abnormality in the maturation of the primary granules with consequent retention of their azurophilic property, while toxic vacuolizations are vacuoles representing phagocytosis and depletion of toxic granules.4
- Interstitial change in the lung – When these interstitial changes occur, your physician may see “increased interstitial markings” on your chest x-ray or CT scan because the inflammation, swelling, or scarring of the interstitium makes the tissue denser so that it is now visible as white “interstitial markings” on the x-ray or scan.5
- CfDNA – In addition to the classic biomarkers, cfDNA was first described in 1948, has the potential to be a useful marker in septic shock. CfDNA is released into the circulation through cell lysis, necrosis, apoptosis, and active DNA release, resulting in higher concentrations of cfDNA in patients with microbial infections, trauma, cancer, and other clinical conditions. Although elevated levels of cfDNA are not specific to a single disease, elevated cfDNA has been shown to be an extremely sensitive and promising prognostic marker in septic shock. This observation may be associated with the shorter half-life of cfDNA than that of PCT and CRP. According to Ahmed, cfDNA is a good prognostic predictor for patients in the ICU and, to a lesser extent, is a good marker of septic shock. However, the inevitable loss of cfDNA during extraction has become a considerable detriment, hindering its clinical applications. We previously developed a duplex real-time PCR assay with an internal control as a novel method for the accurate quantification of plasma cfDNA, which can eliminate preanalytical errors and increase precision and accuracy. Our previous studies showed the clinical value of plasma cfDNA levels, as measured by this novel method, in several conditions. CfDNA levels can be useful not only in evaluating chemotherapy effects and guiding treatment in advanced lung cancer patients but also in assessing liver injury in hepatitis B patients. In this case, cfDNA remained high until the patient died, suggesting that cfDNA could be used to monitor disease progression more effectively than PCT.1
References
- Liu J, Zhang S, Pan S. Value of dynamic plasma cell-free DNA monitoring in septic shock syndrome: A case report. World Journal of Clinical Cases. 2020;8(1):200-207.
- Leith, M. (2021). Murphy’s sign • LITFL • Medical Eponym Library. Life in the Fast Lane • LITFL. Retrieved 5 April 2021, from https://litfl.com/murphys-sign-eponymictionary/#:~:text=Murphy’s%20sign%20is%20elicited%20in,hand%2C%20Murphy’s%20sign%20is%20positive.
- Procalcitonin Test – Understand the Test & Your Results. Labtestsonline.org. (2021). Retrieved 5 April 2021, from https://labtestsonline.org/tests/procalcitonin#:~:text=Procalcitonin%20is%20a%20substance%20produced,systemic%20bacterial%20infections%20and%20sepsis.
- Toxic Granulation – an overview | ScienceDirect Topics. Sciencedirect.com. (2021). Retrieved 5 April 2021, from https://www.sciencedirect.com/topics/medicine-and-dentistry/toxic-granulation#:~:text=Toxic%20granulations%20are%20purple%20or,toxic%20vacuolizations%20are%20vacuoles%20representing.
- Understanding ILD. Interstitial Lung Disease Program. (2021). Retrieved 5 April 2021, from https://med.stanford.edu/ild/patient-resources/understanding-ild.html#:~:text=When%20these%20interstitial%20changes%20occur,the%20x%20ray%20or%20scan.
- Bickle, I. (2021). Bat’s wings of pulmonary edema | Radiology Case | Radiopaedia.org. Radiopaedia.org. Retrieved 21 May 2021, from https://radiopaedia.org/cases/bats-wings-of-pulmonary-oedema.
Creative Commons License
Murphy’s sign is elicited in patients with acute cholecystitis by asking the patient to take in and hold a deep breath while palpating the right subcostal area. If pain occurs on inspiration, when the inflamed gallbladder meets the examiner’s hand, Murphy’s sign is positive.2 A positive Murphy's sign is seen in acute cholecystitis.
Procalcitonin is a substance produced by many types of cells in the body, often in response to bacterial infections but also in response to tissue injury. The level of procalcitonin in the blood can increase significantly in systemic bacterial infections and sepsis. This test measures the level of procalcitonin in the blood.
Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance.
Emmett, Michael; Szerlip, Harold. "Approach to the adult with metabolic acidosis"
Hypokalemia is a low level of potassium in the blood serum.
Soar, J; Perkins, GD; Abbas, G; Alfonzo, A; Barelli, A; Bierens, JJ; Brugger, H; Deakin, CD; Dunning, J; Georgiou, M; Handley, AJ; Lockey, DJ; Paal, P; Sandroni, C; Thies, KC; Zideman, DA; Nolan, JP (October 2010). "European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution". Resuscitation. 81 (10): 1400–33. doi:10.1016/j.resuscitation.2010.08.015. PMID 20956045.
Hypocalcemia is low calcium levels in the blood serum.
LeMone, Priscilla; Burke, Karen; Dwyer, Trudy; Levett-Jones, Tracy; Moxham, Lorna; Reid-Searl, Kerry (2015). Medical-Surgical Nursing. Pearson Higher Education AU. p. 237.
In addition to the classic biomarkers, cfDNA was first described in 1948, has the potential to be a useful marker in septic shock. CfDNA is released into the circulation through cell lysis, necrosis, apoptosis, and active DNA release, resulting in higher concentrations of cfDNA in patients with microbial infections, trauma, cancer, and other clinical conditions. Although elevated levels of cfDNA are not specific to a single disease, elevated cfDNA has been shown to be an extremely sensitive and promising prognostic marker in septic shock. This observation may be associated with the shorter half-life of cfDNA than that of PCT and CRP. According to Ahmed, cfDNA is a good prognostic predictor for patients in the ICU and, to a lesser extent, is a good marker of septic shock. However, the inevitable loss of cfDNA during extraction has become a considerable detriment, hindering its clinical applications. We previously developed a duplex real-time PCR assay with an internal control as a novel method for the accurate quantification of plasma cfDNA, which can eliminate preanalytical errors and increase precision and accuracy. Our previous studies showed the clinical value of plasma cfDNA levels, as measured by this novel method, in several conditions. CfDNA levels can be useful not only in evaluating chemotherapy effects and guiding treatment in advanced lung cancer patients but also in assessing liver injury in hepatitis B patients. In this case, cfDNA remained high until the patient died, suggesting that cfDNA could be used to monitor disease progression more effectively than PCT.
Toxic granulations are purple or dark-blue staining azurophilic granules in the cytoplasm of neutrophils, bands, and metamyelocytes resulting from an abnormality in the maturation of the primary granules with consequent retention of their azurophilic property, while toxic vacuolizations are vacuoles representing phagocytosis and depletion of toxic granules.


