2 Conception, Heredity and Prenatal Development
Chapter Objectives
After this chapter, you should be able to:
- Evaluate roles of nature and nurture in development.
- Define genes and chromosomes.
- Differentiate mitosis and meiosis.
- Explain dominant and recessive patterns on inheritance.
- List common genetic disorders and chromosomal abnormalities.
- Describe changes that occur within each of the three periods of prenatal development.
- Recognize the risks to prenatal development posed by exposure to teratogens.
- Evaluate different types of prenatal assessment.
Introduction
In this chapter, we will begin by examining some of the ways in which heredity helps to shape the way we are. We will look at what happens genetically during conception, and describe some known genetic and chromosomal disorders. Next, we will consider what happens during prenatal development, including the impact of teratogens. We will also discuss the impact that both the mother and father have on the developing fetus (Lally & Valentine-French, 2019, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Heredity, Nature & Nurture
Most scholars agree that there is a constant interplay between nature (heredity) and nurture (the environment). It is difficult to isolate the root of any single characteristic as a result solely of nature or nurture, and most scholars believe that even determining the extent to which nature or nurture impacts a human feature is difficult to answer. In fact, almost all human features are polygenic (a result of many genes) and multifactorial (a result of many factors, both genetic and environmental). It’s as if one’s genetic make-up sets up a range of possibilities, which may or may not be realized depending upon one’s environmental experiences. For instance, a person might be genetically predisposed to develop diabetes, but the person’s lifestyle may determine whether or not they actually develop the disease.
This bidirectional interplay between nature and nurture is the epigenetic framework, which suggests that the environment can affect the expression of genes just as genetic predispositions can impact a person’s potentials. And environmental circumstances can trigger symptoms of a genetic disorder (Lumen Learning, n.d.).
This aspect of development is an important one for educators and caregivers to consider. In fact, in Ontario the College of Early Childhood Educators considers it a professional role and responsibility to demonstrate practice that embraces an understanding of the influence of a child’s experiences on their overall development (College of Early Childhood Educators, 2017). This also includes working with families as partners to ensure the best outcomes for children.
Environment Correlations
Environment Correlations refer to the processes by which genetic factors contribute to variations in the environment (Plomin, DeFries, Knopik, & Neiderhiser, 2013, as cited in Lumen Learning, n.d.). There are three types of genotype-environment correlations:
Passive genotype-environment correlation occurs when children passively inherit the genes and the environments their family provides. Certain behavioural characteristics, such as being athletically inclined, may run in families. The children have inherited both the genes that would enable success at these activities, and given the environmental encouragement to engage in these actions.

Figure 2.1: Two skiers. (Image by Alexey Ruban on Unsplash)
Evocative genotype-environment correlation refers to how the social environment reacts to individuals based on their inherited characteristics. For example, whether one has a more outgoing or shy temperament will affect whether or not they seek out others and how he or she is treated by others.
Active genotype-environment correlation occurs when individuals seek out environments that support their genetic tendencies. This is also referred to as niche picking. For example, children who are musically inclined seek out music instruction and opportunities that facilitate their natural musical ability.
Conversely, Genotype-Environment Interactions involve genetic susceptibility to the environment. Adoption studies provide evidence for genotype-environment interactions. For example, the Early Growth and Development Study (Leve, Neiderhiser, Scaramella, & Reiss, 2010, as cited in Paris, Ricardo, Raymond, & Johnson, 2021) followed 360 adopted children and their adopted and biological parents in a longitudinal study. Results have shown that children whose biological parents exhibited psychopathology, exhibited significantly fewer behaviour problems when their adoptive parents used more structured parenting than unstructured. Additionally, elevated psychopathology in adoptive parents increased the risk for the children’s development of behaviour problems, but only when the biological parents’ psychopathology was high. Consequently, the results show how environmental effects on behaviour differ based on the genotype, especially stressful environments on genetically at-risk children (Lally & Valentine-French, 2019).
Genes and Chromosomes
Now, let’s look more closely at just nature. Nature refers to the contribution of genetics to one’s development. The basic building block of the nature perspective is the gene. Genes are recipes for making proteins, while proteins influence the structure and functions of cells. Genes are located on the chromosomes and there are an estimated 20,500 genes for humans, according to the Human Genome Project (NIH, 2015, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
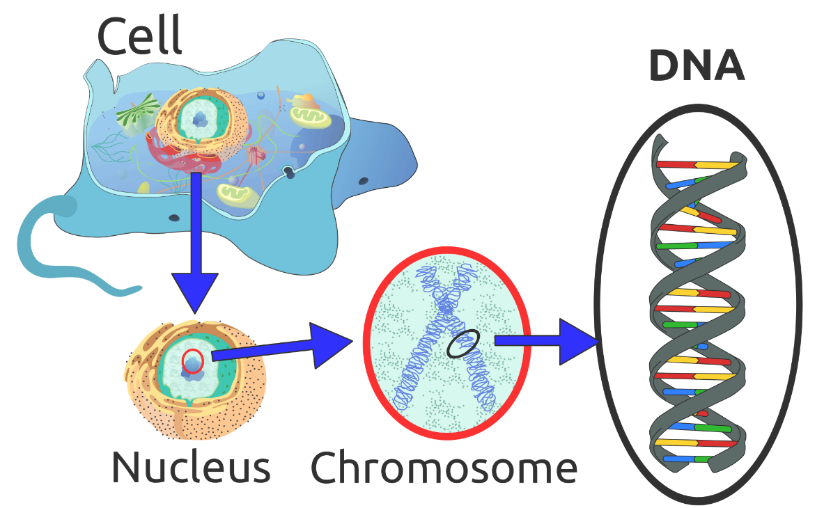
Figure 2.2: DNA’s Location in the cell (Image by Radio89 is licensed under CC BY-SA 3.0 (original image has been modified)
Normal human cells contain 46 chromosomes (or 23 pairs; one from each parent) in the nucleus of the cells. After conception, most cells of the body are created by a process called mitosis. Mitosis is defined as the cell’s nucleus making an exact copy of all the chromosomes and splitting into two new cells.
However, the cells used in sexual reproduction, called the gametes (sperm or ova), are formed in a process called meiosis. In meiosis, the gamete’s chromosomes duplicate, and then divide twice resulting in four cells containing only half the genetic material of the original gamete. Thus, each sperm and egg possesses only 23 chromosomes and combine to produce the normal 46.
| Type of Cell Division | Explanation | Steps |
| Mitosis | All cells, except those used in sexual reproduction, are created by mitosis | Chromosomes make a duplicate copy
Two identical cells are created |
| Meiosis | Cells used in sexual reproduction are created by meiosis | Exchange of gene between the chromosomes (crossing over)
Chromosomes make a duplicate First cell division Second cell division |
Table 2.1: Mitosis & Meiosis (Lally & Valentine-French, 2019).
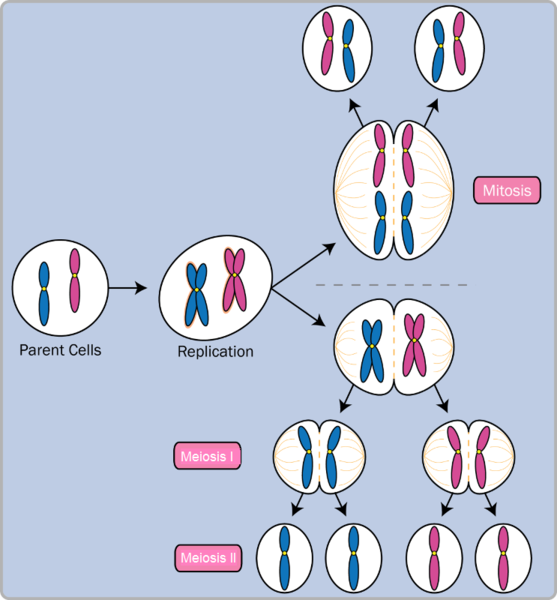
Figure 2.3: Mitosis and Meiosis. (Image by Community College Consortium for Bioscience Credentials is licensed under CC BY 3.0)
Given the number of genes present and the unpredictability of the meiosis process, the likelihood of having offspring that are genetically identical (and not twins) is one in trillions (Gould & Keeton, 1997, as cited in as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Of the 23 pairs of chromosomes created at conception, 22 pairs are similar in length. These are called autosomes. The remaining pair, or sex chromosomes, may differ in length. It is the Y chromosome that determines sex. If the Y chromosome is present, the child will be genetically male. If the Y chromosome is absent, the child will be genetically female (Lally & Valentine-French, 2019).
Here is an image (called a karyogram) of what the 23 pairs of chromosomes look like. Notice the differences between the sex chromosomes in female (XX) and male (XY).
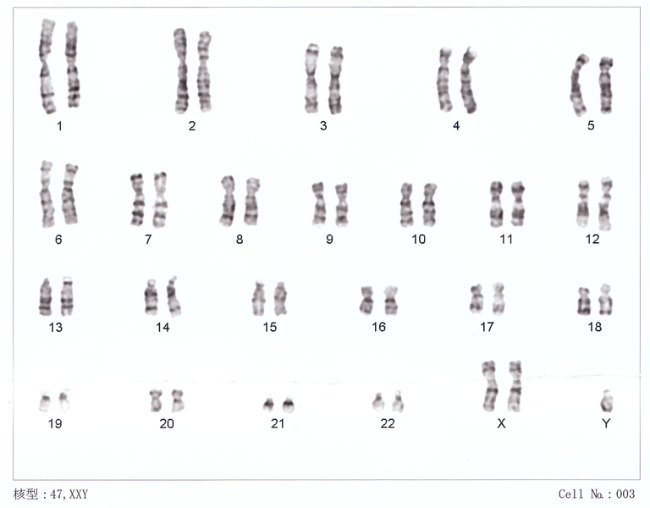
Figure 2.4: The 23 pairs of chromosomes. (Image by Nami-ja is in the public domain)
Genotypes, Phenotypes & Patterns on Inheritance
The word genotype refers to the sum total of all the genes a person inherits. The word phenotype refers to the features that are actually expressed. Look in the mirror. What do you see, your genotype or your phenotype? What determines whether or not genes are expressed?
Because genes are inherited in pairs on the chromosomes, we may receive either the same version of a gene from our mother and father, that is, be homozygous for that characteristic the gene influences. If we receive a different version of the gene from each parent, that is referred to as heterozygous.
In the homozygous situation we will display that characteristic. It is in the heterozygous condition that it becomes clear that not all genes are created equal. Some genes are dominant, meaning they express themselves in the phenotype even when paired with a different version of the gene, while their silent partner is called recessive. Recessive genes express themselves only when paired with a similar version gene. Geneticists refer to different versions of a gene as alleles. Some dominant traits include having facial dimples, curly hair, normal vision, and dark hair. Some recessive traits include red hair, being nearsighted, and straight hair.
Most characteristics are not the result of a single gene; they are polygenic, meaning they are the result of several genes. In addition, the dominant and recessive patterns described above are usually not that simple either. Sometimes the dominant gene does not completely suppress the recessive gene; this is called incomplete dominance (Lally & Valentine-French, 2019).
Genetic Disorders
Most of the known genetic disorders are dominant gene-linked.
Recessive gene disorders, such as cystic fibrosis and sickle-cell anemia, are less common but may actually claim more lives because they are less likely to be detected as people are unaware that they are carriers of the disease.
Some genetic disorders are sex-linked; the defective gene is found on the X-chromosome. Males have only one X chromosome so are at greater risk for sex-linked disorders due to a recessive gene such as hemophilia, color-blindness, and baldness. For females to be affected by recessive genetic defects, they need to inherit the recessive gene on both X-chromosomes. But if the defective gene is dominant, females are equally at risk.
Recessive Disorders (Homozygous): The individual inherits a gene change from both parents. If the gene is inherited from just one parent, the person is a carrier and does not have the condition.
| Disorder | Description | Incidence |
| Sickle Cell Disease (SCD) | A condition in which the red blood cells in the body are shaped like a sickle (like the letter C) and affect the ability of the blood to transport oxygen. | 1 in 500 Black births
1 in 36,000 Hispanic births 1 in 2,500 babies born in Canada |
| Cystic Fibrosis (CF) | A condition that affects breathing and digestion due to thick mucus building up in the body, especially the lungs and digestive system. In CF, the mucus is thicker than normal and sticky. | 1 in 3,600 live births in Canada |
| Phenylketonuria (PKU) | A metabolic disorder in which the individual cannot metabolize phenylalanine, an amino acid. Left untreated, intellectual deficits occur. PKU is easily detected and is treated with a special diet. | 1 in 12,000 births in Canada |
| Tay Sachs Disease | Caused by an enzyme deficiency resulting in the accumulation of lipids in the nerves cells of the brain. This accumulation results in progressive damage to the cells and a decrease in cognitive and physical development. Death typically occurs by age five. | 1 in 320,000 births in the general population
1 in 30 people of Ashkenazi Jewish descent is a carrier 1 in 20 people of French-Canadian descent is a carrier |
| Albinism | When the individual lacks melanin and processes little to no pigment in the skin, hair, and eyes. Vision problems can also occur. | 1 in every 17,000 – 20,000 people in North America and Europe |
Table 2.2: Recessive Disorders (Homozygous) (Lally & Valentine-French, 2019).
Autosomal Dominant Disorders (Heterozygous): In order to have the disorder, the individual only needs to inherit the gene change from one parent.
| Disorder | Description | Incidence |
| Huntington’s Disease | A condition that affects the individual’s nervous system. Nerve cells become damaged, causing various parts of the brain to deteriorate. The disease affects movement, behavior and cognition. It is fatal, and occurs at midlife. | 1 in 10,000 |
| Tourette Syndrome | A tic disorder which results in uncontrollable motor and vocal tics as well as body jerking | 1 in 250 |
| Achondroplasia | The most common form of disproportionate short stature. The individual has abnormal bone growth resulting in short stature, disproportionately short arms and legs, short fingers, a large head, and specific facial features. | 1 in 15,000-40,000 |
Table 2.3 : Autosomal Dominant Disorders (Heterozygous) (Lally & Valentine-French, 2019).
Sex-Linked Disorders: When the X chromosome carries the mutated gene, the disorder is referred to as an X-linked disorder. Males are more affected than females because they possess only one X chromosome without an additional X chromosome to counter the harmful gene.
| Disorder | Description | Incidence |
| Fragile X Syndrome | Occurs when the body cannot make enough of a protein it needs for the brain to grow and problems with learning and behavior can occur. Fragile X syndrome is caused from an abnormality in the X chromosome, which then breaks. If a female has a fragile X, her second X chromosome usually is healthy, but males with fragile X don’t have a second healthy X chromosome. This is why symptoms of Fragile X usually are more serious in males. | 1 in 4000 males
1 in 8000 females |
| Hemophilia | Occurs when there are problems in blood clotting causing both internal and external bleeding. Hemophilia is more common in males than females. The two most common types are hemophilia A and hemophilia B. | Hemophilia A: leas than 1 in 10,000 people in Canada
Hemophilia B: 1 in 50,000 people in Canada |
| Duchenne Muscular Dystrophy | A weakening of the muscles resulting in an inability to move, wasting away, and possible death. This form of muscular dystrophy affects males almost exclusively. | 1 in 3500 Male live births |
Table 2.4: Sex-Linked Disorders (Lally & Valentine-French, 2019).
Chromosomal Abnormalities: A chromosomal abnormality occurs when a child inherits too many or two few chromosomes. Some gametes do not divide evenly when they are forming. Therefore, some cells have more than 46 chromosomes. In fact, it is believed that close to half of all zygotes have an odd number of chromosomes. Most of these zygotes fail to develop and are spontaneously aborted by the mother’s body (Lally & Valentine-French, 2019, p.38).
Autosomal Chromosome Disorders: The individual inherits too many or two few chromosomes.
| Disorder | Description |
| Down Syndrome/ Trisomy 21 | Caused by an extra chromosome 21 and includes a combination of birth defects. Affected individuals have some degree of intellectual disability, characteristic facial features, often heart defects, and other health problems. The severity varies greatly among affected individuals. In Canada, approximately 1 in every 781 babies is born with Down Syndrome While the risk of having a baby with Down Syndrome increases with the mother’s age, half of babies born with Down Syndrome are born to mothers under 35 years of age. (Reference: Canadian Down Syndrome Society). |
| Trisomy 9 Mosaicism | Caused by having an extra chromosome 9 in some cells. The severity of effects relates to the proportion of cells with extra chromosomes. The effects include fetal growth restriction resulting in low birth weight and multiple anomalies, including facial, cardiac, musculoskeletal, genital, kidney, and respiratory abnormalities. |
| Trisomy 13 | Caused by an extra chromosome 13. Affected individuals have multiple birth defects and generally die in the first weeks or months of life. |
| Trisomy 18 | Caused by an extra chromosome 18 and the affected individual also has multiple birth defects and early death. |
Table 2.5: Autosomal Chromosomal Disorders[Trisomy 9 Mosaicism Diagnosed In Utero by Hironori Takahashi, Satoshi Hayashi, Yumiko Miura, Keiko Tsukamoto, Rika Kosaki, Yushi Itoh, and Haruhiko Sago is licensed under CC BY 3.0; Lifespan Development: A Psychological Perspective (page 39) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0
Figure 2.5: Infant boy with Trisomy 9 Mosaicism. (Image by Ashley Onken used with permission)

Figure 2.6: Girl with XXX Syndrome. (Image is in the public domain)
Sex-linked Chromosome Disorders: When the abnormality is on 23rd pair, the result is a sex-linked chromosomal abnormality. This happens when a person has less than or more than two sex chromosomes (Lally & Valentine-French, 2019, p. 38).
| Disorder | Description |
| Turner Syndrome (XO) | Caused when all or part of one of the X chromosomes is lost before or soon after conception due to a random event. The resulting zygote has an XO composition. Turner Syndrome affects cognitive functioning and sexual maturation in females. Infertility and a short stature may be noted. |
| Klinefelter Syndrome (XXY) | Caused when an extra X chromosome is present in the cells of a male due to a random event. The Y chromosome stimulates the growth of male genitalia, but the additional X chromosome inhibits this development. The male can have some breast development, infertility, and low levels of testosterone. |
| XXY Syndrome | Caused when an extra Y chromosome is present in the cells of a male. There are few symptoms. They may include being taller than average, acne, and an increased risk of learning problems. The person is generally otherwise normal, including normal fertility. |
| Triple X Syndrome (XXX) | Caused when an extra X chromosome is present in the cells of a female. It may result in being taller than average, learning difficulties, decreased muscle tone, seizures, and kidney problems. |
Table 2.6: Sex-Linked Chromosomal Disorders]XYY Syndrome by Wikipedia is licensed under CC BY-SA 3.0; Triple X Syndrome by Wikipedia is licensed under CC BY-SA 3.0; Lifespan Development: A Psychological Perspective (page 39) by Martha Lally and Suzanne Valentine-French is licensed under CC BY-NC-SA 3.0
Triple Screening in Pregnancy: The triple screen blood test is one type of genetic screening test. It measures alpha-fetoprotein, human chorionic gonadotropin and unconjugated estriol. An abnormal test result is not a diagnosis, only an indication that the baby might be at higher risk for some birth defects. Additional testing is usually required, such as an ultrasound or amniocentesis.
Prenatal Development
Now we turn our attention to prenatal development which is divided into three periods: The germinal period, the embryonic period, and the fetal period. The following is an overview of some of the changes that take place during each period.
The Germinal Period
The germinal period (about 14 days in length) lasts from conception to implantation of the fertilized egg in the lining of the uterus. At ejaculation millions of sperm are released into the vagina, but only a few reach the egg and typically only one fertilizes the egg. Once a single sperm has entered the wall of the egg, the wall becomes hard and prevents other sperm from entering. After the sperm has entered the egg, the tail of the sperm breaks off and the head of the sperm, containing the genetic information from the father, unites with the nucleus of the egg. It is typically fertilized in the top section of the fallopian tube and continues its journey to the uterus. As a result, a new cell is formed. This cell, containing the combined genetic information from both parents, is referred to as a zygote.

Figure 2.7: Sperm and ovum at conception. (Image is in the public domain)
During this time, the organism begins cell division through mitosis. After five days of mitosis there are 100 cells, which is now called a blastocyst. The blastocyst consists of both an inner and outer group of cells. The inner group of cells, or embryonic disk will become the embryo, while the outer group of cells, or trophoblast, becomes the support system which nourishes the developing organism. This stage ends when the blastocyst fully implants into the uterine wall (U.S. National Library of Medicine, 2015, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
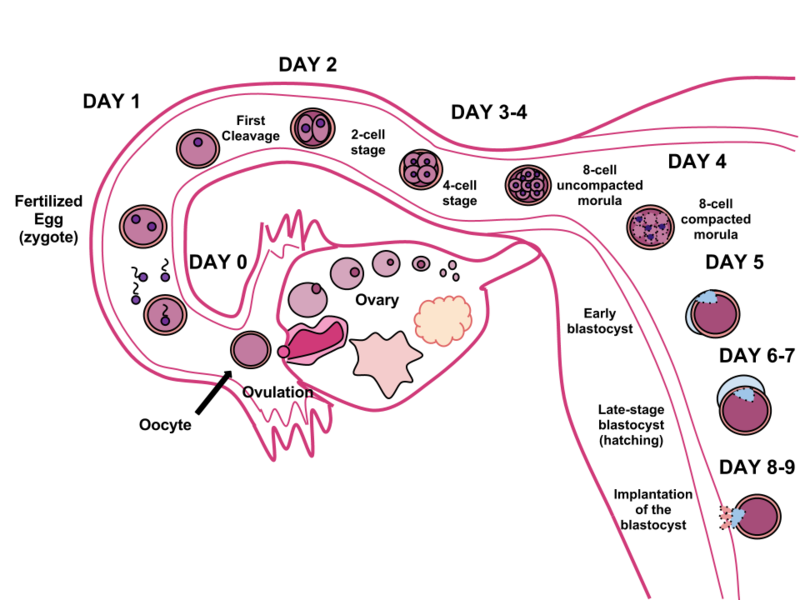
Figure 2.8: The cycle of fertilization. (Image by Ttrue12 is licensed under CC BY-SA 3.0)
Mitosis is a fragile process and fewer than one half of all zygotes survive beyond the first two weeks (Hall, 2004). Some of the reasons for this include: the egg and sperm do not join properly, thus their genetic material does not combine, there is too little or damaged genetic material, the zygote does not replicate, or the blastocyst does not implant into the uterine wall. The figure above illustrates the journey of the ova from its release to its fertilization, cell duplication, and implantation into the uterine lining (Lally & Valentine-French, 2019,p. 42-43).
The Embryonic Period
Starting the third week, the blastocyst has implanted in the uterine wall. Upon implantation this multi-cellular organism is called an embryo. Now blood vessels grow forming the placenta. The placenta is a structure connected to the uterus that provides nourishment and oxygen from the mother to the developing embryo via the umbilical cord.
During this period, cells continue to differentiate. Growth during prenatal development occurs in two major directions: from head to tail called cephalocaudal development and from the midline outward referred to as proximodistal development. This means that those structures nearest the head develop before those nearest the feet and those structures nearest the torso develop before those away from the center of the body (such as hands and fingers). You will see that this pattern continues after birth.
The head develops in the fourth week and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. However, by the end of this stage they disappear and the organism takes on a more human appearance.

Figure 2.9: A human embryo. (Image by Anatomist90 is licensed under CC BY-SA 3.0)
About 20 percent of organisms fail during the embryonic period, usually due to gross chromosomal abnormalities, often before the mother even knows that they are pregnant. It is during this stage that the major structures of the body are taking form, making the embryonic period the time when the organism is most vulnerable to the greatest amount of damage if exposed to harmful substances. Prospective mothers are not often aware of the risks they introduce to the developing embryo during this time. The embryo is approximately 1 inch in length and weighs about 4 grams at the end of eight weeks. The embryo can move and respond to touch at this time. (Lally & Valentine-French, 2019, p. 43).
The Fetal Period
From the ninth week until birth (which is forty weeks for a full-term pregnancy), the organism is referred to as a fetus. During this stage, the major structures are continuing to develop. By the third month, the fetus has all its body parts including external genitalia. The fetus is about 3 inches long and weighs about 28 grams. In the following weeks, the fetus will develop hair, nails, teeth and the excretory and digestive systems will continue to develop.

Figure 2.10: A human fetus. (Image by lunar caustic is licensed under CC BY-SA 2.0)
During the 4th – 6th months, the eyes become more sensitive to light and hearing develops. The respiratory system continues to develop, and reflexes such as sucking, swallowing and hiccupping, develop during the 5th month. Cycles of sleep and wakefulness are present at this time as well. The first chance of survival outside the womb, known as the age of viability is reached at about 24 weeks (Morgan, Goldenberg, & Schulkin, 2008, as cited in Paris, Ricardo, Raymond & Johnson, 2021). The majority of the neurons in the brain have developed by 24 weeks, although they are still rudimentary, and the glial or nurse cells that support neurons continue to grow. At 24 weeks the fetus can feel pain (Royal College of Obstetricians and Gynecologists, 1997, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Between the 7th – 9th months, the fetus is primarily preparing for birth. It is exercising its muscles and its lungs begin to expand and contract. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy, and during the 8th month a layer of fat develops under the skin. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
At around 36 weeks the fetus is almost ready for birth. It weighs about 6 pounds and is about 18.5 inches long. By week 37 all of the fetus’s organ systems are developed enough that it could survive outside the mother’s uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. By then the fetus has very little room to move around and birth becomes imminent. The progression through the stages is shown in the following figure (Lally & Valentine-French, 2019, p. 44).

Figure 2.11: The development of a fetus. (Image by CNX Psychology is licensed under CC BY 4.0)
Monozygotic and Dizygotic Twins
Monozygotic or identical twins occur when a fertilized egg splits apart in the first two weeks of development. The result is the creation of two separate identical offspring. That is, they possess the same genotype and often the same phenotype. About one-third of twins are monozygotic twins.
Sometimes, however, two eggs or ova are released and fertilized by two separate sperm. The result is dizygotic or fraternal twins. These two individuals share the amount of genetic material as would any two children from the same mother and father. In other words, they possess a different genotype and phenotype.
Older mothers are more likely to have dizygotic twins than are younger mothers, and couples who use fertility drugs are also more likely to give birth to twins (Lally & Valentine-French, 2019, p. 36) .
Figure 2.12: Monozygotic Twins. (Image is in the public domain)
Figure 2.13: Dizygotic Twins. (Image by Jennifer Paris used with permission)
Teratogens
Good prenatal care is essential to protect against maternal and fetal/infant mortality and birth complications. The embryo and fetus are most at risk for some of the most severe problems during the first three months of development. Unfortunately, this is a time at which many mothers are unaware that they are pregnant. Today, we know many of the factors that can jeopardize the health of the developing child. Teratogens are environmental factors that can contribute to birth defects, and include some maternal diseases, pollutants, drugs and alcohol. The study of these factors that contribute to birth defects is called teratology.
Factors influencing prenatal risks: There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Berger, 2005, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). These include:
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, the ears and arms reach their critical periods at about 6 weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed. (see figure below)
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
- The number of teratogens: Fetuses exposed to multiple teratogens typically have more problems than those exposed to only one.
- Genetics: Genetic makeup also plays a role on the impact a particular teratogen might have on the child. This is suggested by fraternal twins exposed to the same prenatal environment, but they do not experience the same teratogenic effects. The genetic makeup of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Being male or female: Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact (Lally & Valentine-French, 2019, p. 46/47).
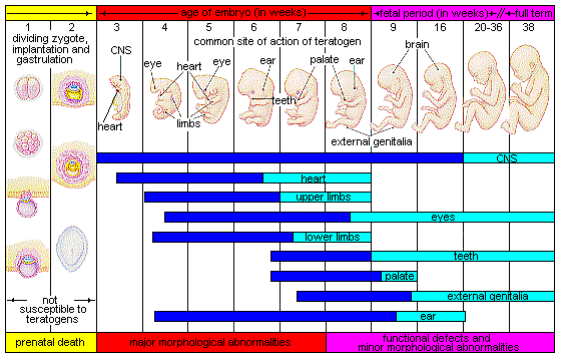
Figure 2.14: The development of an embryo into a fetus. (Image by Laura Overstreet is licensed under CC BY-NC-SA 3.0)
There are four categories of teratogens:
- Physical teratogens: These could be saunas, hot tubs, or infections that raise a pregnant woman’s body temperature to 102 degrees Fahrenheit or higher. This is associated with neural tube defects, spontaneous abortions, and various cardiovascular abnormalities.
- Metabolic conditions affecting pregnant females: Metabolic conditions are abnormalities in the chemical process of producing energy from food, and thereby affect the development and function of the body. If a pregnant woman is malnourished, then her fetus likely lacks the nutrients essential for its development. These include: malnutrition, diabetes, and thyroid disorders.
- Infections: Different maternal infections, including rubella virus, herpes simplex virus, and syphilis can cause congenital abnormalities in fetuses.
- Drugs and chemicals: When pregnant females ingest or absorb these, they may cause a variety of different effects based on specific agent, amount of exposure, and timing. This category includes: radiation, heavy metals (including lead), insecticides and herbicides, prescription and over the counter drugs, illicit and recreational drugs, alcohol, cigarettes, nicotine, caffeine, and even some vitamins (Tantibanchachai, 2014).
While there are many, many potential teratogens, the following tables look at the effects of some different types of teratogens. The risks of exposure vary based on lifestyle and health. The effects may vary greatly depending on the factors mentioned previously. Protection and prevention will vary based on the method of exposure.
| Teratogen | Potential Effects |
| Caffeine | Moderate amounts of caffeine (200 mg or around 12 ounces of coffee) appear to be safe during pregnancy. Some studies have shown a link between higher amounts of caffeine and miscarriage and preterm birth. Staying healthy and safe by OWH is in the public domain |
| Tobacco | Tobacco use has been associated with low birth weight, placenta previa, preterm delivery, fetal growth restriction, sudden infant death syndrome, cleft lip or palate, and later health problems (such as high blood pressure and diabetes).Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Staying healthy and safe by OWH is in the public domain |
| Alcohol | There is no safe amount of alcohol a woman can drink while pregnant. Alcohol can slow down the baby’s growth, affect the baby’s brain, and cause birth defects, and may results in fetal alcohol spectrum disorder (FASD). The effects can be mild to severe. Children born with a severe form of FASD can have abnormal facial features, severe learning disabilities, behavioral problems, and other problems.Staying healthy and safe by OWH is in the public domain |
| Cocaine | Cocaine use has connected with low birth weight, stillbirths, spontaneous abortion, placental abruption, premature birth, miscarriage, and neonatal abstinence syndrome (fetal addiction leads the newborn to experiences withdrawal).Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Marijuana | No amount of marijuana has been proven safe to use during pregnancy. Heavy use has been associated with brain damage, premature birth, and stillbirth.Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0; Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx |
| Heroin | Using heroin during pregnancy can cause birth defects, placental abruption, premature birth, low birthweight, neonatal abstinence syndrome, still birth, and sudden infant death syndrome.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx |
| Over-the-Counter (OTC) medication | Some OTC medications are safe to use during pregnancy and others may cause health problems during pregnancy. Pregnant women should consult their health care provider before using OTC medications.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Prescription drugs | Some prescription drugs can cause birth defects that change the shape or function of one or more parts of the body that can affect overall health. Pregnant women should consult their health care provider before discontinuing or starting new medications.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Herbal or dietary supplements | Except for some vitamins, little is known about using herbal or dietary supplements while pregnant. Most often there are no good studies to show if the herb can cause harm to you or your baby. Also, some herbs that are safe when used in small amounts as food might be harmful when used in large amounts as medicines.Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0[ |
Table 2.7 – Drugs as Teratogens (Paris, Ricardo, Raymond, & Johnson, 2021)
| Teratogen | Potential Effects |
| Lead> | Exposure to high levels of lead before and during pregnancy can lead to high blood pressure, problems with fetal brain and nervous system development, premature birth, low birthweight, and miscarriage.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Mercury | Exposure to mercury in the womb can cause brain damage and hearing and vision problems.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Radiation | Exposure to radiation during pregnancy (especially between 2 and 18 weeks of pregnancy) can slow growth, cause birth defects, affect brain development, cause cancer, and cause miscarriage.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Solvents | These chemicals include degreasers, paint thinners, stain and varnish removers, paints, and more Maternal inhalation of solvents can cause fetal exposure than may cause miscarriage, slow fetal growth, premature birth, and birth defects.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Radon | Radon is a radioactive gas naturally found in the environment when uranium in soil and rock breaks down. Radon is odorlous, invisible and tasteless. Research in this area is limited, but one unreplicated research study in 2016 concluded there is an association between residential radon levels and the occurrence of cleft lip and cystic hygroma (a fluid-filled sac that results from a blockage in the lymphatic system). (Langlois, P. H., Lee, M., Lupo, P. J., Rahbar, M. H., & Cortez, R. K. (2016). Residential radon and birth defects: A population-based assessment. Birth defects research. Part A, Clinical and molecular teratology, 106(1), 5–15. https://doi.org/10.1002/bdra.23369) |
Table 2.8 – Environmental Teratogens (Paris, Ricardo, Raymond, & Johnson, 2021)
| Teratogen | Potential Effects |
| Rubella | Congenital infection (becoming infected while in the womb) can damage the development of the eyes, ears, heart, and brain and result in deafness.Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0[ |
| Zika | Congenital infection can cause microcephaly and other severe brain abnormalities.Protocols on prenatal care for pregnant women with Zika infection and children with microcephaly: nutritional approach by Rachel de Sá Barreto Luna Callou Cruz, Malaquias Batista Filho, Maria de Fátima Costa Caminha, and Edvaldo da Silva Souza is licensed under CC BY 4.0[ |
| Varicella (chicken pox) | Congenital infection can cause a severe form of the infection affecting the eyes, limbs, skin, and central nervous system.Congenital Varicella syndrome by WikiDoc is licensed under CC BY-SA 3.0[ |
| Sexually transmitted infections | Infections such as HIV, gonorrhea, syphilis, and chlamydia can be passed from the mother during pregnancy and/or delivery.Chapter 3: Prenatal Development – Environmental Risks references Psyc 200 Lifespan Psychology by Laura Overstreet, which is licensed under CC BY 4.0[ |
| Listeria | Pregnant women are more susceptible to this food-borne illness. Congenital infection can cause miscarriage, stillbirth, premature labor, and neonatal sepsis.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2860824/[ |
Table 2.9 – Maternal Infections as Teratogens (as cited in Paris, Ricardo, Raymond, & Johnson, 2021)
| Teratogen | Potential Effects |
| Toxoplamosis | This parasite can be passed through cat feces and undercooked meat (especially pork, lamb, or deer meat). If the fetus is infected it can cause miscarriage, stillbirth, hydrocephalus, macro or microcephalus, vision issues, and damage to the nervous system.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
| Lymphocytic choriomeningitis | This virus carried by rodents including mice, hamsters, and guinea pigs. If an infected mother passes it to her fetus it can cause issues with brain development, long-term neurological and/or visual impairment, and higher mortality rates after birth.Prescription drugs, over-the-counter drugs, supplements and herbal products (n.d.). Retrieved from: https://www.marchofdimes.org/pregnancy/prescription-drugs-over-the-counter-drugs-supplements-and-herbal- products.aspx[ |
Table 2.10: Teratogens from Animals/Pets (as cited in Paris, Ricardo, Raymond, & Johnson, 2021)
Maternal Factors
There are additional factors that affect the outcome of pregnancy for both mother and child. Let’s look at these next.
Mothers over 35
Most women over 35 who become pregnant are in good health and have healthy pregnancies. However, according to the March of Dimes (2016d, as cited in as cited in Paris, Ricardo, Raymond, & Johnson, 2021), women over age 35 are more likely to have an increased risk of:
- Fertility problems
- High blood pressure
- Diabetes
- Miscarriages
- Placenta Previa
- Cesarean section
- Premature birth
- Stillbirth
- A baby with a genetic disorder or other birth defects
Because are born with all of their eggs, environmental teratogens can affect the quality of the eggs as women get older. Also, a woman’s reproductive system ages which can adversely affect the pregnancy. Some women over 35 choose special prenatal screening tests, such as a maternal blood screening, to determine if there are any health risks for the baby.
Although there are medical concerns associated with having a child later in life, there are also many positive consequences to being a more mature parent. Older parents are more confident, less stressed, and typically married, providing family stability. Their children perform better on math and reading tests, and they are less prone to injuries or emotional troubles (Albert, 2013, as cited in as cited in Paris, Ricardo, Raymond, & Johnson, 2021). Women who delay pregnancy either by choice or because of challenges with conceiving are often better educated and have healthier lifestyles. According to Gregory (2007, as cited in as cited in Paris, Ricardo, Raymond, & Johnson, 2021), older women are more stable, demonstrate a stronger family focus, possess greater self-confidence, and have more money. Having a child later in one’s career equals overall higher wages. In fact, for every year a woman delays motherhood, she makes 9% more in lifetime earnings. Lastly, women who delay having children actually live longer.
Paternal Factors
Male fertility is also affected by age. The quality of semen starts to decline after the age of 35. Sperm motility also declines with age. Genetic defects in sperm increase with age. These defects have been associated with: decreased fertility, increased risk of miscarriage, increase risk of some birth defects and increase risk of stillbirth (Gurevich, 2020).
Teenage Pregnancy
A teenage mother is at a greater risk for having pregnancy complications including anemia, and high blood pressure.
These risks are even greater for those under age 15. Infants born to teenage mothers have a higher risk for being premature and having low birthweight or other serious health problems. Premature and low birthweight babies may have organs that are not fully developed which can result in breathing problems, bleeding in the brain, vision loss, serious intestinal problems, and higher likelihood of dying. Reasons for these health issues include that teenagers are the least likely of all age groups to get early and regular prenatal care and they may engage in negative behaviours including eating unhealthy food, smoking, drinking alcohol, and taking drugs.
Experiences of Indigenous Women
An extensive literature review conducted in 2016 concluded that availability of healthcare resources, healthcare services’ consideration of socio-economic or lifestyle barriers to health, and the impact of colonization on interactions with healthcare providers were main factors that impacted Indigenous women’s maternal health experiences. Medical evacuation was often due to limited maternity care options available in remote communities, and was associated with emotional, physical, and financial stress. The review highlighted the importance of consistent health policies and practices for maternal health in Canada and providing culturally safe and patient-centered maternity healthcare services within indigenous communities (Kolahdooz, Launier, Nader, Yi, Baker, McHugh, Vallianatos & Sharma, 2016).
Kenhteke Midwives on the Tyendinaga Mohawk Territory in Canada is an example of culturally appropriate maternal and newborn care that “sustains our way of life by birthing our children in the hands of our own people, on our land, using our language, traditions, culture and traditional medicines” (Kenhteke Midwives, 2017).
Gestational Diabetes
Gestational diabetes can occur if the body cannot produce enough insulin to adapt to the effects of a growing fetus and changing hormone levels. The cells become resistant to the action of insulin and, in turn, the pancreas cannot secrete enough insulin to counterbalance the effect of these hormones.
In Canada, between 3% and 20% of pregnant women develop gestational diabetes, depending on their risk factors. While the rate for all pregnancies is roughly 2%-4%, the rate in First Nations women has been reported to be between 8% and 18% (Diabetes Canada, 2022). Research by Dyck et al. (2002, as cited in First Nations Centre, National Aboriginal Health Organization, 2009) concluded that First Nations ancestry is an independent risk factor; that is, even when a woman has none of the other risk factors for developing gestational diabetes, if she is of First Nations ancestry, she is more likely to develop gestational diabetes. The researchers concluded that the reasons for this were unclear.
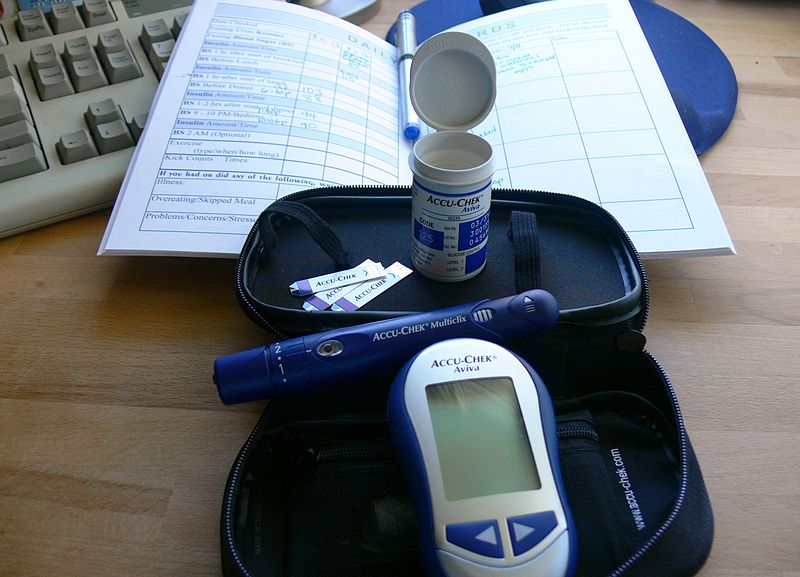
Figure 2.15: A gestational diabetes kit. (Image by Jessica Merz is licensed under CC BY 2.0)
Most pregnant women have their glucose level tested between 24 to 28 weeks of pregnancy. Gestational diabetes usually goes away after the mother gives birth, but it might indicate a risk for developing diabetes later in life. If untreated, gestational diabetes can cause premature birth, stillbirth, the baby having breathing problems at birth, jaundice, or low blood sugar. Babies born to mothers with gestational diabetes can also be considerably heavier (more than 9 pounds) making the labor and birth process more difficult. For expectant mothers, untreated gestational diabetes can cause preeclampsia (high blood pressure and signs that the liver and kidneys may not be working properly) discussed later in the chapter.
Risk factors for gestational diabetes include age (being over age 25), being overweight or gaining too much weight during pregnancy, family history of diabetes, having had gestational diabetes with a prior pregnancy, and race and ethnicity. In addition to women with First Nation ancestry, African-American, Native American, Hispanic, Asian, or Pacific Islander have a higher risk. Eating healthy, exercising regularly and maintaining a healthy weight during pregnancy can reduce the chance of developing gestational diabetes. If these actions are unsuccessful at controlling blood sugar levels, insulin may be required. Women who already have diabetes and become pregnant need to attend all their prenatal care visits, and follow the same advice as those for women with gestational diabetes as the risk of preeclampsia, premature birth, birth defects, and stillbirth are the same.
High Blood Pressure (Hypertension)
Hypertension is a condition in which the pressure against the wall of the arteries becomes too high. There are two types of high blood pressure during pregnancy, gestational and chronic. Gestational hypertension only occurs during pregnancy and goes away after birth. Chronic high blood pressure refers to women who already had hypertension before the pregnancy or to those who developed it during pregnancy and it did not go away after birth.

Figure 2.16: A woman having her blood pressure taken. (Image by rawpixel on Unsplash)
According to the March of Dimes (2015, as cited in Paris, Ricardo, Raymond, & Johnson, 2021), about 8 in every 100 pregnant women have high blood pressure. High blood pressure during pregnancy can cause premature birth and low birth weight (under five and a half pounds), placental abruption, and mothers can develop preeclampsia.
Rh Disease
Rh is a protein found in the blood. Most people are Rh positive, meaning they have this protein. Some people are Rh negative, meaning this protein is absent. Mothers who are Rh negative are at risk of having a baby with a form of anemia called Rh disease (March of Dimes, 2009). A father who is Rh-positive and mother who is Rh-negative can conceive a baby who is Rh-positive. Some of the fetus’s blood cells may get into the mother’s bloodstream and the immune system is unable to recognize the Rh factor.
The immune system starts to produce antibodies to fight off what it thinks is a foreign invader. Once the body produces immunity, the antibodies can cross the placenta and start to destroy the red blood cells of the developing fetus. As this process takes time (longer than 9 months), often the first Rh positive baby is not harmed, but as the mother’s body will continue to produce antibodies to the Rh factor across their lifetime, subsequent pregnancies can pose greater risk for an Rh positive baby. When there is Rh incompatibility (Rh negative woman conceives an Rh positive baby), RhoGAM, a manufactured antibody, is given to the pregnant woman at 28 weeks and again after delivery. This prevents the mother from developing the antibodies that would attack the baby’s blood cells in the event that the blood crosses the placenta. In the newborn, Rh disease can lead to jaundice, anemia, heart failure, brain damage and death.
Weight Gain during Pregnancy
According to March of Dimes (2016, as cited in Paris, Ricardo, Raymond, & Johnson, 2021), during pregnancy most women need only an additional 300 calories per day to aid in the growth of the fetus. Gaining too little or too much weight during pregnancy can be harmful. Women who gain too little may have a baby who is low-birth weight, while those who gain too much are likely to have a premature or large baby. There is also a greater risk for the mother developing preeclampsia and diabetes, which can cause further problems during the pregnancy.
The table below shows the healthy weight gain during pregnancy. Putting on the weight slowly is best. Mothers who are concerned about their weight gain should talk to their health care provider.
| If you were a healthy weight before pregnancy: | If you were underweight before pregnancy:> | If you were overweight before pregnancy: | If you were obese before pregnancy: |
| Gain 25-35 pounds | Gain 28-30 pounds | Gain 12-25 pounds | 11-20 pounds |
| 1-4½ pounds in the 1st trimester
1 pound per week in the 2nd and 3rd trimesters |
1-4½ pounds in the 1st trimester
A little more than 1 pound per week |
1-4½ pounds in the 1st trimester
A little more than ½ pound per week in 2nd and 3rd |
1-4½ pounds in the 1st trimester
A little more than ½ pound per week in 2nd and 3rd |
| Mothers of twins or higher order multiples need to gain more in each category. | thereafter | trimesters | trimesters |
Table 2.10 – Weight Gain during Pregnancy (Paris, Ricardo, Raymond & Johnson, 2021).
Stress
Feeling stressed is common during pregnancy, but high levels of stress can cause complications including having a premature baby or a low-birthweight baby. Babies born early or too small are at an increased risk for health problems. Stress-related hormones may cause these complications by affecting a woman’s immune systems resulting in an infection and premature birth. Additionally, some women deal with stress by smoking, drinking alcohol, or taking drugs, which can lead to problems in the pregnancy. High levels of stress in pregnancy have also been correlated with problems in the baby’s brain development and immune system functioning, as well as childhood problems such as trouble paying attention and being afraid (March of Dimes, 2012, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Depression
Depression is a significant medical condition in which feelings of sadness, worthlessness, guilt, and fatigue interfere with one’s daily functioning. According to the Mayo Clinic, about 7% of women experience depression during pregnancy (Mayo Clinic, 2022).
Women who have experienced depression previously are more likely to have depression during pregnancy. Consequences of depression include the baby being born premature, having a low birth weight, being more irritable, less active, less attentive, and having fewer facial expressions.
About 13% of pregnant women take an antidepressant during pregnancy. It is important that women taking antidepressants during pregnancy discuss the medication with a health care provider as some medications can cause harm to the developing organism.
Paternal Impact
The age of fathers at the time of conception is also an important factor in health risks for children. According to Nippoldt (2015, as cited in Paris, Ricardo, Raymond, & Johnson, 2021), offspring of men over 40 face an increased risk of miscarriages, autism, birth defects, achondroplasia (bone growth disorder) and schizophrenia. These increased health risks are thought to be due to accumulated chromosomal aberrations and mutations during the maturation of sperm cells in older men (Bray, Gunnell, & Smith, 2006, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). However, like older women, the overall risks are small.
In addition, men are more likely than women to work in occupations where hazardous chemicals, many of which have teratogenic effects or may cause genetic mutations, are used (Cordier, 2008, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). These may include petrochemicals, lead, and pesticides that can cause abnormal sperm and lead to miscarriages or diseases. Men are also more likely to be a source of second hand smoke for their developing offspring. As noted earlier, smoking by either the mother or around the mother can hinder prenatal development (Lally & Valentine-French, 2019. p.52).

Figure 2.17: A USDA employee pouring hazardous chemicals into a storage container. (Image by USDA is in the public domain)
Prenatal Assessment
A number of assessments are suggested to women as part of their routine prenatal care to find conditions that may increase the risk of complications for the mother and fetus (Eisenberg, Murkoff, & Hathaway, 1996, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). These can include blood and urine analyses and screening and diagnostic tests for birth defects.

Figure 2.18: A woman receiving an ultrasound. (Creator: Keith Brofsky | Credit: Getty Images)
Ultrasound is one of the main screening tests done in combination with blood tests. The ultrasound is a test in which sound waves are used to examine the fetus. There are two general types. Transvaginal ultrasounds are used in early pregnancy, while transabdominal ultrasounds are more common and used after 10 weeks of pregnancy (typically, 16 to 20 weeks).
Ultrasounds are used to check the fetus for defects or problems. It can also find out the age of the fetus, location of the placenta, fetal position, movement, breathing and heart rate, amount of amniotic fluid in the uterus, and number of fetuses. Most women have at least one ultrasound during pregnancy, but if problems are noted, additional ultrasounds may be recommended.
When diagnosis of a birth defect is necessary, ultrasounds help guide the more invasive diagnostic tests of amniocentesis and chorionic villus sampling. Amniocentesis is a procedure in which a needle is used to withdraw a small amount of amniotic fluid and cells from the sac surrounding the fetus and later tested.
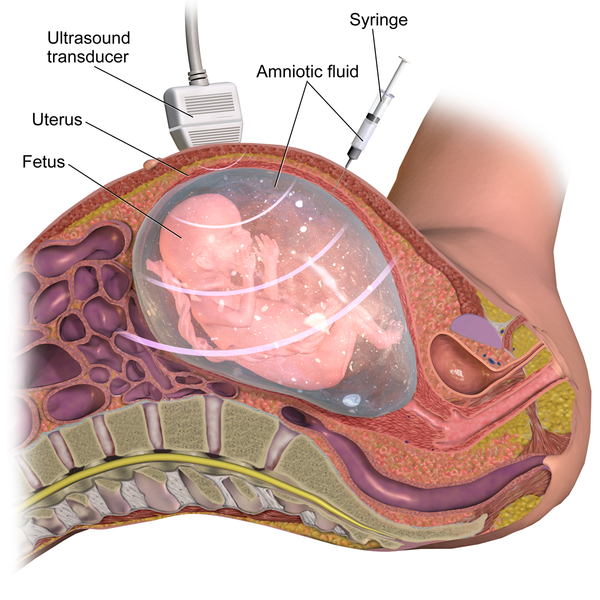
Figure 2.19: Amniocentesis. (Image by BruceBlaus is licensed under CC BY-SA 4.0)
Chorionic Villus Sampling is a procedure in which a small sample of cells is taken from the placenta and tested. Both amniocentesis and chorionic villus sampling have a risk of miscarriage, and consequently they are not done routinely (Lally & Valentine-French, 2019).
Side Effects of Pregnancy
There are a number of common side effects of pregnancy. Not everyone experiences all of these, nor to the same degree. In most cases, these side effects will not harm the developing fetus, but this is not to say that they are not potentially very uncomfortable for the mother. These side effects include nausea (particularly during the first 3-4 months of pregnancy as a result of higher levels of estrogen in the system), heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, shortness of breath or varicose veins (as a result of carrying a heavy load on the abdomen).
But there are also serious complications of pregnancy which can pose health risks to mother and child and that often require hospitalization.
Hyperemesis gravidarum is characterized by severe nausea, vomiting, weight loss, and possibly dehydration. Signs and symptoms may also include vomiting many times a day and feeling faint. The exact causes of hyperemesis gravidarum are unknown. Risk factors include the first pregnancy, multiple pregnancy, obesity, prior or family history of HG, trophoblastic disorder, and a history of eating disorders. Treatment includes drinking fluids and a bland diet. Medication, intravenous fluids, and hospitalization may be required. Hyperemesis gravidarum is estimated to affect 0.3–2.0% of pregnant women. Those affected have a low risk of miscarriage but a higher risk of premature birth.
Ectopic Pregnancy occurs when the zygote becomes attached to the fallopian tube before reaching the uterus. The rate of ectopic pregnancy is about 2% in the general population (Canadian Medical Association Journal, 2005).
This number has been increasing because of the higher rates of pelvic inflammatory disease and Chlamydia (Carroll, 2007, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). Abdominal pain, vaginal bleeding, nausea and fainting are symptoms of ectopic pregnancy.
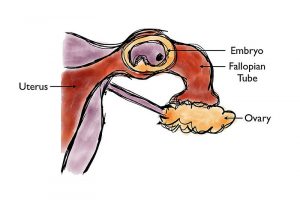
Figure 2.20: An ectopic pregnancy. (Image by Takatakatakumi is licensed under CC BY-SA 3.0)
The Society of Obstetricians and Gynaecologists of Canada estimates that 15 to 20% of pregnancies end in a miscarriage. In many cases, a miscarriage is due to chromosomal abnormalities in the developing fetus, and this typically happens before the 12th week of pregnancy. Cramping and bleeding result and normal periods return after several months. Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems, but miscarriage can also be a result of defective sperm (Carrell et. al., 2003, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Preeclampsia, also known as Toxemia, is characterized by a sharp rise in blood pressure, a leakage of protein into the urine as a result of kidney problems, and swelling of the hands, feet, and face during the third trimester of pregnancy. Preeclampsia is the most common complication of pregnancy. When preeclampsia causes seizures, the condition is known as eclampsia. Preeclampsia is also a leading cause of fetal complications, which include low birth weight, premature birth, and stillbirth. Treatment is typically bed rest and sometimes medication. If this treatment is ineffective, labor may be induced.
Maternal Mortality: According to to the World Health Organization (2017), approximately 800 women around the world died each day from preventable causes related to pregnancy and childbirth. Rates are highest in Sub-Saharan Africa and South Asia, although there has been a substantial decrease in these rates. The campaign to make childbirth safe for everyone has led to the development of clinics accessible to those living in more isolated areas and training more midwives to assist in childbirth (as cited in Lally & Valentine-French, 2019, p. 58).
Options for Building Families
There are numerous options to pursue parenthood and building families. Let’s briefly explore some of these.
Assisted Reproductive Technology: Assisted reproductive technology (ART) is the technology used to achieve pregnancy in procedures such as fertility medication (to stimulate ovulation), surgical procedures, artificial insemination IUI), in vitro fertilization (IVF) and surrogacy. These options are available for people who are experiencing infertility or cannot conceive children naturally, which also includes single parents, and LGBTQIA2S+ couples (Fertilitypedia, n.d., as cited by Paris, Ricardo, Raymond, & Johnson, 2021).
Intrauterine insemination: (IUI) as a type of artificial insemination involves the placement of sperm directly into the uterus at the time of ovulation, either in a natural menstrual cycle or following ovarian stimulation (Fertilitypedia, n.d., as cited by Paris, Ricardo, Raymond, & Johnson, 2021).
In vitro fertilization (IVF): IVF generally starts with stimulating the ovaries to increase mature egg production. Most fertility medications are agents that stimulate the development of follicles in the ovary. Examples are gonadotropins and gonadotropin releasing hormone. After stimulation, the physician surgically extracts one or more eggs from the ovary, and unites them with sperm in a laboratory setting, with the intent of producing one or more embryos. Fertilization takes place outside the body, and the fertilized egg is reinserted into the woman’s reproductive tract, in a procedure called embryo transfer (Fertilitypedia, n.d., as cited by Paris, Ricardo, Raymond, & Johnson, 2021).

Figure 2.21: The IVF process. (Image by Manu5 is licensed under CC BY-SA 4.0)
Donor Gametes & Embryos: People can also use sperm, ova (eggs), and embryos from donors in conjunction with assisted reproduction technology. In Canada, the Assisted Human Reproduction Act (2004) makes it illegal to sell or buy sperm, ova and embryos.
Surrogacy: In surrogacy, one woman (surrogate mother) carries a child for another person/s (commissioning person/couple), based on a legal agreement before conception requiring the child to be relinquished to the commissioning person/couple following birth. There are different types of surrogacy which relate to whether or not the ova used to conceive the child are their own (traditional surrogacy) or not (gestational surrogacy) (Fertilitypedia, n.d., as cited by Paris, Ricardo, Raymond, & Johnson, 2021).
Adoption: People can also choose to pursue adoption to build their families (with or without experiencing infertility). Adoption can take place through the foster care system, privately, or through agencies. Adoptions can be domestic (within Canada) or international. And they can be open (with differing amounts of contact between biological/birth families and adoptive families) or closed.
Family Built with Surrogacy (Photo by Daryn Crawford used with permission)

Figure 2.22: This same-sex couple used a surrogate. (Photo by Daryn Crawford used with permission)

Figure 2.23: This single mother adopted her daughter. (Photo by Michaela Szidloski used with permission)
Summary
- Heredity, including genetic disorders and chromosomal abnormalities
- Conception
- The germinal, embryonic, and fetal stages of prenatal development
- Influences on prenatal development including teratogens and maternal and paternal factors
- Complications of pregnancy
- Infertility and options for building families
References
Canadian Medical Association Journal. (2005, October 11). Diagnosis and treatment of etopic pregnancy. Retrieved from https://www.cmaj.ca/content/173/8/905
College of Early Childhood Educators. (2017). Code of ethics and standards of practice for early childhood educators in Ontario. Retrieve from https://www.college-ece.ca/en/Documents/Code_and_Standards_2017.pdf
Diabetes Canada. (2022). Gestational diabetes. Retrieved from https://www.diabetes.ca/about-diabetes/gestational
First Nations Centre, National Aboriginal Health Organization. (2009, December). Gestational diabetes and first nations women:
A literature review. Retrieved from https://fnim.sehc.com/getmedia/a7198c67-da87-44e9-9cc4-1d681303fef8/Gestational_Diabetes_LitReview_2009.pdf.aspx?ext=.pdf
Gurevich, R. (2020, April 20). Does age affect male fertility? Retrieved from https://www.verywellfamily.com/does-age-affect-male-fertility-1959934
Kenhteke Midwives. (2017). Welcome to Kenhteke midwives. Retrieved from https://kenhtekemidwives.com/#tab-id-4
Kolahdooz, F. , Launier, K., Nader, F. , Yi,K., Baker, P., McHugh, T., Vallianatos, H. and Sharma, S. (2016, September 2). Canadian indigenous womens perspectives of maternal health and health care services: A systematic review. Retrieved from https://diversityhealthcare.imedpub.com/canadian-indigenous-womens-perspectives-ofmaternal-health-and-health-care-services-asystematic-review.php?aid=11328
Lally, M. & Valentine-French, S. (2019). Lifespan development: A psychological perspective. Retrieved from http://dept.clcillinois.edu/psy/LifespanDevelopment.pdf
Lumen Learning. (n.d.). Introduction to heredity, prenatal development and birth. Retrieved from https://courses.lumenlearning.com/lifespandevelopment2/chapter/lesson-3-heredity-prenatal-development-and-birth/
Mayo Clinic. (2022). Depression during pregnancy; You’re not alone. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/depression-during-pregnancy/art-20237875
Tantibanchachai, C. (2014, January 22). Teratogens. In the embryo project encyclopedia. Retrieved from https://embryo.asu.edu/pages/teratogens

