3 Birth and the Newborn
Chapter Objectives
After this chapter, you should be able to:
- Compare and contrast different methods of childbirth preparation.
- Describe the stages of vaginal delivery.
- Explain why induction or Caesarean section may be necessary.
- Differentiate the common procedures for assessing the condition of the newborn.
- Examine problems newborns experience before, during, and after birth.
introduction
In this chapter we will explore childbirth and the early experiences of the newborn which includes having to regulate their own body temperature, breathe for themselves, and take in all of their nutrition through feeding.
After around 266 days of developing inside the womb (for a full-term pregnancy), comes the arduous process of childbirth. For many reasons, each pregnancy and delivery is unique and influenced by social and cultural factors as well as personal choices made about preparing for childbirth. Let’s begin by exploring some of the approaches to childbirth.
Preparing for Childbirth
Prepared childbirth refers to being not only in good physical condition to help provide a healthy environment for the baby to develop, but also helping individuals to prepare to accept their new roles as parents. Additionally, parents can receive information and training that will assist them in delivery and life with the baby. The more future parents can learn about childbirth and the newborn, the better prepared they will be for the adjustment they must make to a new life.
Approaches to Childbirth
Support for Culturally Safe Indigenous Birth
Children born into their home community are more likely to develop a clear sense of identity, which helps to promote resilience and build strong community bonds. However, most Indigenous women are forced to travel to urban centres to give birth in settings that may not feel culturally secure. Care providers and administrators need to value and incorporate birth traditions, rituals, and ceremonies, provide different options for safe maternity care outside of major centres, and increase the number of Indigenous maternity care providers (e.g., midwives, doulas, birth workers).
Care providers may be well-meaning in their intentions to care for the Indigenous mother and their infant based on their professional training, but this has also resulted in birth being medicalized in Western ways with subsequent loss of traditional birth practices, ceremonies, and rituals for Indigenous families (National Aboriginal Council of Midwives, 2016, as cited in Exner-Pirot, Norbye and Butler, 2018). To offer quality maternity care to Indigenous mothers and their families, providers should work towards practicing cultural safety. Cultural safety addresses inequities arising from sociocultural factors and power differentials between service providers and those they care for; clinical practice without cultural safety contributes to the continued oppression of Indigenous peoples (Roy, 2014, as cited in Exner-Pirot, Norbye and Butler, 2018). Learning about different peoples and cultures is a key component of gaining cultural competence for care providers (Kirmayer, 2012; Tervalon & Murray-García, 1998, as cited in Exner-Pirot, Norbye and Butler, 2018). Therefore, increasing care provider understanding about traditional maternal and newborn Indigenous birthing practices and ceremonies is essential to promote cultural security for childbearing women (Exner-Pirot, Norbye and Butler, 2018).
| Method | Description |
| The Lamaze Method | The emphasis of this method is on teaching the woman to be in control in the process of delivery. It includes learning muscle relaxation, breathing through contractions, having a focal point (usually a picture to look at) during contractions and having a support person who goes through the training process with the mother and serves as a coach during delivery. |
| The Leboyer Method | This method involves giving birth in a quiet, dimly lit room and allowing the newborn to lie on the mother’s stomach with the umbilical cord intact for several minutes while being given a warm bath. |
| Dick-Read Method / Mongan Method / Hypnobirthing | This method comes from the suggestion that the fear of childbirth increases tension and makes the process of childbearing more painful. It emphasizes the use of relaxation and proper breathing with contractions as well as family support and education. |
| Bradley Method | “The Bradley Method focuses on preparing the mother for a natural childbirth coached by her partner. They learn techniques to reduce the perception of pain and stay relaxed. The emphasis is on being prepared for an unassisted vaginal birth without medication.” Oberg, Erica (n.d.). Childbirth Delivery Methods and Types. Retrieved from https://www.medicinenet.com/ 7_childbirth_and_delivery_methods/article.htm#childbirth_and_delivery_methods_and_types_facts. |
| Alexander Technique | This is a technique that can be used during childbirth that involves training to stop habitual reactions to pain, such as tensing muscles and increase conscious awareness and control over posture and movement. This involves being able to move freely and stay upright during labor and using body positioning that is beneficial to the labor process. Machover, Ilana. (n.d.). The Alexander Technique in Natural Childbirth. Retrieved from https://www.alexandertechnique.com/articles/ childbirth/. |
| Waterbirth | Involves immersion in warm water. Proponents believe this method is safe and provides many benefits for both mother and infant, including pain relief and a less traumatic birth experience for the baby. However, critics argue that the procedure introduces unnecessary risks to the infant such as infection and water inhalation. Water Birth by Wikidoc is licensed under CC BY-SA 3.0 |
| Lotus Birth | Or umbilical cord nonseverance – UCNS, is the practice of leaving the umbilical cord uncut after childbirth so that the baby is left attached to the placenta until the cord naturally separates at the umbilicus. This usually occurs within 3–10 days after birth. The practice is performed mainly for spiritual purposes of the parents, including for the perceived spiritual connection between placenta and newborn. Lotus Birth by Wikipedia is licensed under CC BY-SA 3.0 |
| Silent Birth | Sometimes known as quiet birth, is a birthing procedure in which “everyone attending the birth should refrain from spoken words as much as possible.” Silent Birth by Wikipedia is licensed under CC BY-SA 3.0 |
| Medicated Childbirth | Health care providers can provide pain relief during labor with different types of medication, including epidurals, spinal blocks, combined spinal-epidurals, and systemic and local analgesia. There are benefits and side effects of each.Epidural and Spinal Anesthesia Use During Labor: 27-state Reporting Area, 2008 by Michelle J.K. Osterman and Joyce A. Martin is in the public domain |
Table 3.1: Birthing Methods (Lally & Valentine French, 2019, as cited in Paris, Ricardo, Raymond, & Johnson, 2021)

Figure 3.1: Expectant parents in a childbirth preparation class. (Image by liz.schrenk is licensed under CC BY-NC-ND 2.0)
Choosing Location of Childbirth & Who Will Deliver
The vast majority of births occur in a hospital setting. However, approximately 1% of births in Canada in 2019 were in locations other than a hospital (Statistics Canada, 2020). Live births and fetal deaths (stillbirths), by place of birth (hospital or non-hospital) Women who are at low risk for birth complications can successfully deliver at home. More than half (67%) of home deliveries are by certified nurse midwives. In 1994, Ontario became the first province in Canada to regulate midwifery. “Midwifery is a health care profession distinct from nursing. Midwives specialize in providing primary care to women during pregnancy, labour, birth and postpartum in relation to low risk prenatal, intrapartum and postnatal care.” (Mah, 2013). In order to practice midwifery in Ontario, midwives must be registered with the College of Midwives of Ontario, and must adhere to the by-laws of the College. There are exemptions to these legal requirements for aboriginal midwives and healers. In Ontario, services of midwives are funded by the provincial government and there is no fee charged to the expectant mother.
childbirth
Onset of Labor
Childbirth typically occurs within a week of a woman’s due date, unless the woman is pregnant with more than one fetus, which usually causes an early labor early. As a pregnancy progresses into its final weeks, several physiological changes occur in response to hormones that trigger labor.
A common sign that labor is beginning is the so-called “bloody show.” During pregnancy, a plug of mucus accumulates in the cervical canal, blocking the entrance to the uterus. Approximately 1–2 days prior to the onset of true labor, this plug loosens and is expelled, along with a small amount of blood.
As labor nears, the mothers’ pituitary gland produces oxytocin. This begins to stimulate stronger, more painful uterine contractions, which—in a positive feedback loop—stimulate the secretion of prostaglandins from fetal membranes. Like oxytocin, prostaglandins also enhance uterine contractile strength. The fetal pituitary gland also secretes oxytocin, which increases prostaglandins even further.
And the stretching of the cervix by a full-term fetus in the head-down position is regarded as a stimulant to uterine contractions. Combined, these stimulate true labor (Biga, Dawson, Harwell, Hopkins, Kaufmann, LeMaster, Matern, Morrison-Graham, Quick, & Runyeon, n.d., as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Stages of Birth for Vaginal Delivery: The First Stage
Uterine contractions signify that the first stage of labor has begun. These contractions may initially last about 30 seconds and be spaced 15 to 20 minutes apart. These increase in duration and frequency to more than a minute in length and about 3 to 4 minutes apart. Typically, doctors and midwives advise that they be called when contractions are coming about every 5 minutes. Some women experience false labor or Braxton-Hicks Contractions, especially with the first child. These may come and go. They tend to diminish when the mother begins walking around. Real labor pains or contractions tend to increase with walking. In one out of 8 pregnancies, the amniotic sac or water in which the fetus is suspended may break before labor begins. In such cases, the physician or midwife may induce labor with the use of medication if it does not begin on its own within twenty-four hours in order to reduce the risk of infection. Normally this sac does not rupture until the later stages of labor.
The first stage of labor is typically the longest. During this stage the cervix or opening to the uterus dilates to 10 centimeters or just under 4 inches. This may take around 12-16 hours for first children or about 6-9 hours for women who have previously given birth. It is during this stage that strategies learned in childbirth classes such as breathing techniques and finding visual focal points can be of great benefit to the labour process. Labor may also begin with a discharge of blood or amniotic fluid.
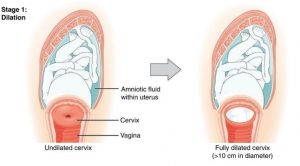
Figure 3.2: Early Cervical dilation. (Image by OpenStax is licensed under CC BY 3.0)
The Second Stage
The passage of the baby through the birth canal is the second stage of labor. This stage takes about 10-40 minutes. Contractions usually come about every 2-3 minutes. The mother pushes and relaxes as coached by the birthing team. Typically, the head is delivered first. The baby is then rotated so that one shoulder can come through and then the other shoulder. The rest of the baby quickly passes through. At this stage, an episiotomy, or incision made in the tissue between the vaginal opening and anus, may be performed to avoid tearing the tissue of the back of the vaginal opening (Mayo Clinic, 2016, as cited in Lally & Valentine French, 2019). The baby’s mouth and nose are suctioned out. The umbilical cord is clamped and cut (Lally & Valentine French, 2019, p.60, as cited in Paris, Ricardo, Raymond, & Johnson, 2021)
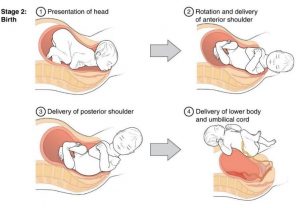
Figure 3.3: Full dilation and expulsion of the newborn.(Image by OpenStax is licensed under CC BY 3.0)
The Third Stage
The third and final stage of labor is relatively painless. During this stage, the placenta or afterbirth is delivered. This is typically within 20 minutes after delivery. If an episiotomy was performed it is stitched up during this stage (Lally & Valentine French, 2019, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
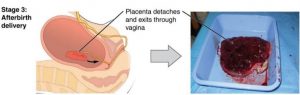
Figure 3.4: Delivery of the placenta and associated fetal membranes. (Image by OpenStax is licensed under CC BY 3.0)
Indigenous Perspective
Once the baby is born there is a ceremony performed that will connect the baby to mother earth (connection to the land and all creation).
Additional Considerations
An epidural block is a regional analgesic that can be used during labor and alleviates most pain in the lower body without slowing labor. The epidural block can be used throughout labor and has little to no effect on the baby. Medication is injected into a small space outside the spinal cord in the lower back. It takes 10 to 20 minutes for the medication to take effect. An epidural block with stronger medications, such as anesthetics, can be used shortly before a Cesarean Section or if a vaginal birth requires the use of forceps or vacuum extraction (Lally & Valentine French, 2019, p. 60). In Canada, epidural rates have risen from 53.2% in 2006/07 to 57.8% in 2015/16 (Public Health Agency of Canada,2018).
Women giving birth can also receive other pain medications (although medications given through injection can have negative side effects on the baby). In emergency situations (such as the need for a C-section), women may be given general anesthesia. They can also choose not to utilize any pain medications. That is often referred to as natural childbirth.

Figure 3.5: Natural childbirth. (Image by U.S. Army Alaska is licensed under CC BY 2.0)
Women can also use alternate positions (including standing, squatting, being on hands and knees, and using a birthing stool) and labouring, and even delivering in tubs of warm water to help relieve the pain of childbirth.
Medical Interventions in Childbirth
Sometimes women cannot go into labor on their own and/or deliver vaginally. Let’s look at induction of labor and cesarean sections.
Sometimes a baby’s arrival may need to be induced before labor begins naturally. Induction of labor may be recommended for a variety of reasons when there is a concern for the health of the mother or baby. For example:
- The mother is approaching two weeks beyond the due date and labor has not started naturally
- The mother’s water has broken, but contractions have not begun
- There is an infection in the mother’s uterus
- The baby has stopped growing at the expected pace
- There is not enough amniotic fluid surrounding the baby
- The placenta peels away, either partially or completely, from the inner wall of the uterus before delivery
- The mother has a medical condition that might put them or the baby at risk, such as high blood pressure or diabetes (Mayo Clinic, 2014, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
A cesarean section (C-section) is surgery to deliver the baby by being removed through the mother’s abdomen. In Canada, cesarean births have risen from 17.6% in 1995/96 to 27.9% in 2015/16 (Public Health Agency of Canada, 2018). Most C-sections are done when problems occur during delivery unexpectedly.
These can include:
- Health problems in the mother
- Signs of distress in the baby
- Not enough room for the baby to go through the vagina
- The position of the baby, such as a breech presentation where the head is not in the downward position or a transverse lie, where the baby may be sideways.

Figure 3.6: A woman receiving a C-section. (Image by Tammra M is licensed under CC BY 2.0)

Figure 3.7: A baby being delivered by C-section. (Image by Patricia Prudente on Unsplash)
C-sections are also more common among women carrying more than one baby. Although the surgery is relatively safe for mother and baby, it is considered major surgery and carries health risks. Additionally, it also takes longer to recover from a C-section than from vaginal birth. After healing, the incision may leave a weak spot in the wall of the uterus. This could cause problems with an attempted vaginal birth later. In the past, doctors were hesitant to allow a vaginal birth after a C-section. However, now more than half of women who have a C-section go on to have a vaginal birth later (Lally & Valentine-French, 2019, p. 61). This is referred to as a Vaginal Birth After Cesarean (VBAC).
The Newborn

Figure 3.8: A new mother holding her newborn. (Image by the U.S. Air Force is in the public domain)
Assessing the Newborn
The Apgar assessment is conducted one minute and five minutes after birth. This is a very quick way to assess the newborn’s overall condition. Five measures are assessed: Heart rate, respiration, muscle tone (assessed by touching the baby’s palm), reflex response (the Babinski reflex is tested), and colour. A score of 0 to 2 is given on each feature examined. An Apgar of 5 or less is cause for concern. The second Apgar should indicate improvement with a higher score (Lally & Valentine-French, 2019, p. 63).
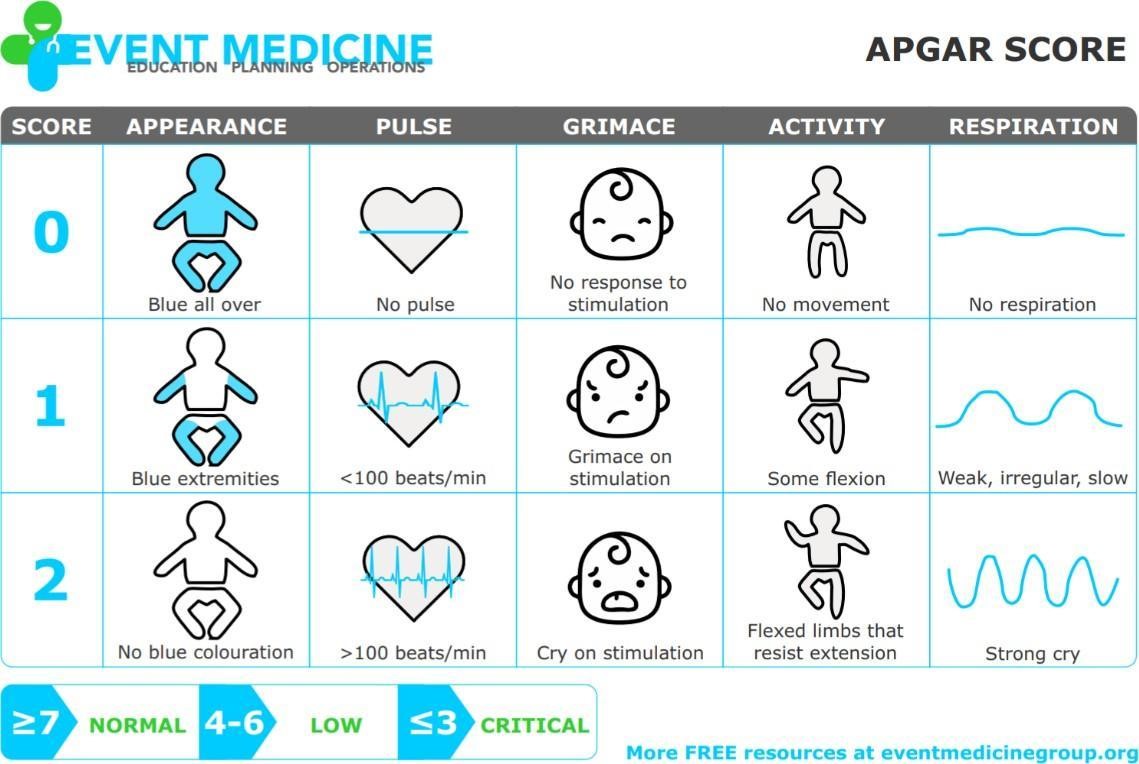
Figure 3.9: The Apgar assessment. (Image by Event Medicine Group)
Another way to assess the condition of the newborn is the Neonatal Behavioral Assessment Scale (NBAS). The baby’s motor development, muscle tone, and stress response are assessed. This tool has been used around the world to further assess the newborn, especially those with low Apgar scores, and to make comparisons of infants in different cultures (Brazelton & Nugent, 1995, as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Newborns are also routinely screened for different conditions. Within the first 24 to 48 hours after birth, babies born in hospitals undergo a simple heel stick and a few drops of blood are collected on a special paper card. Providers test those dried blood spots for a variety of different congenital disorders, or conditions that are present when the baby is born.

Figure 3.10: A medical professional performing the heel stick test. (Image by the U.S. Air Force is in the public domain) Newborns are also screened for hearing disorders and certain serious heart problems using methods other than dried blood spots.Newborn Screening is in the public domain ; Newborn Screening Program (NBS) by the California Department of Public Health is in the public domain
In Ontario all newborns in hospital and community settings have a universal hearing screening administered as part of the Infant Hearing Program. This screening identifies infants who should have more in-depth testing for hearing loss as early as possible.
Most babies will pass the newborn hearing screening which means their hearing is fine at this time (Government of Ontario, 2021).
Complications with the Newborn
Anoxia
Anoxia is a temporary lack of oxygen to the brain. Difficulty during delivery may lead to anoxia which can result in brain damage or in severe cases, death. Babies who suffer both low birth weight and anoxia are more likely to suffer learning disabilities later in life as well.
Low Birth Weight
A child is considered low birth weight if they weigh less than 2500 grams (5.5lbs). In 2017, 6.5% of babies born in Canada weighed less than 2500 grams. There are regional differences in this statistic. For example, in the Northwest Territories, 5.9% of babies were low birth weight. Ontario was slightly above the national figure at 6.7%. In Nunavut, 7.8% of babies were low birth weight (Statistics Canada, 2018a).
A low birth weight baby has difficulty maintaining adequate body temperature because it lacks the fat that would otherwise provide insulation. Such a baby is also at more risk for infection.
Very low birth weight babies (2 pounds or less) have an increased risk of developing cerebral palsy. Many causes of low birth weight are preventable with proper prenatal care.
Preterm
A newborn might also have a low birth weight if it is born at less than 37 weeks gestation, which qualifies it as a preterm baby (CDC, 2015, as cited in Paris, Ricardo, Raymond, & Johnson, 2021). Early birth can be triggered by anything that disrupts the mother’s system. For instance, vaginal infections can lead to premature birth because such infection causes the mother to release anti-inflammatory chemicals which, in turn, can trigger contractions. Smoking and the use of other teratogens can lead to preterm birth. A significant consequence of preterm birth includes respiratory distress syndrome, which is characterized by weak and irregular breathing (see the image below). Premature babies often cannot yet regulate their own temperature or feed by nursing or bottle. They may struggle to regulate their heart rate effectively and may experience jaundice. They often require care in the Neonatal Intensive Care Unit (NICU) until they are as healthy as a full-term baby.

Figure 3.11: a premature baby on CPAP (continuous positive airway pressure)in the NICU. (Photo by Jennifer Paris used with permission)
Small-for-Date Infants
Infants that have birth weights that are below expectation based on their gestational age are referred to as small-for-date. These infants may be full term or preterm (see image below), but still weigh less than 90% of all babies of the same gestational age. This is a very serious situation for newborns as their growth was adversely affected. Regev et al. (2003, as cited in Paris, Ricardo, Raymond, & Johnson, 2021) found that small-for-date infants died at rates more than four times higher than other infants.

Figure 3.12: This baby was born at 32 weeks and only weighed 2 pounds and 15 ounces. (Photo by Jennifer Paris used with permission)
Postmature
When babies are not born by 42 weeks gestation, or two weeks after their due date, they are considered overdue or postmature. There are some concerns about how long the placenta can function and most doctors will consider induction for overdue babies.
Stillborn
When a fetus (unborn baby) dies while still inside the mother (after 20-24 weeks gestation) or dies during delivery (childbirth), it is said that the delivered baby is stillborn. The causes of many stillbirths are unknown, even when special tests are done to learn the cause. Possible causes include: nicotine, alcohol, or drugs taken by the mother during pregnancy, physical trauma, radiation poisoning, Rh disease, and umbilical cord problems.
In 2019, there were 3,191 stillbirths in Canada. This is a fetal death rate of 8.6 per 1,000 total births (Statistics Canada, 2020).
Characteristics of Newborns
Size
The average newborn in the United States weighs about 7.5 pounds and is about 20 inches in length. In Canada the average weight is 3,530 grams or 7 pounds, 12.5 ounces. Read this article in The Star for more info.
For the first few days of life, infants typically lose about 5 percent of their body weight as they eliminate waste and get used to feeding. This often goes unnoticed by most parents, but can be cause for concern for those who have a smaller infant. This weight loss is temporary, however, and is followed by a rapid period of growth.

Figure 3.13: A newborn being weighed. (Image by Trei Brundrett is licensed under CC BY-SA 2.0)
Body Proportions
The head initially makes up about 50 percent of our entire length when we are developing in the womb. At birth, the head makes up about 25 percent of our length (think about how much of your length would be head if the proportions were still the same!).
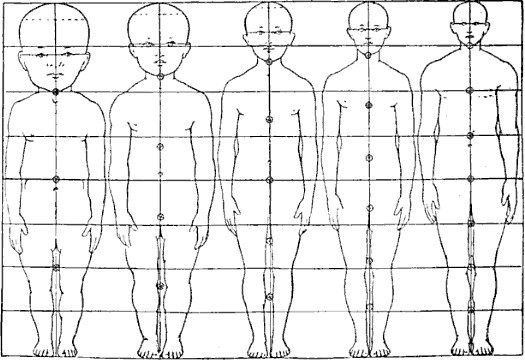
Figure 3.14: Body proportions from infancy to adulthood.(Image is in the public domain)
Brain Development
Some of the most dramatic physical changes that occur during this period are in the brain. At birth, the brain is about 25 percent its adult weight and this is not true for any other part of the body. While most of the brain’s 100 to 200 billion neurons are present at birth, they are not fully mature. During the next several years dendrites or connections between neurons will undergo a period of transient exuberance or temporary dramatic growth.
Appearance at Birth
During labor and birth, the infant’s skull changes shape to fit through the birth canal, sometimes causing the child to be born with a misshapen or elongated head. It will usually return to normal on its own within a few days or weeks.
Some newborns have a fine, downy body hair called lanugo. It may be particularly noticeable on the back, shoulders, forehead, ears and face of premature infants. Lanugo disappears within a few weeks. Likewise, not all infants are born with lush heads of hair. Some may be nearly bald while others may have very fine, almost invisible hair. Some babies are even born with a full head of hair. Amongst fair-skinned parents, this fine hair may be blond, even if the parents are not.
Immediately after birth, a newborn’s skin is often grayish to dusky blue in colour. As soon as the newborn begins to breathe, usually within a minute or two, the skin’s colour returns to its normal tone. Newborns are wet, covered in streaks of blood, and coated with a white substance known as vernix, which is thought to act as an antibacterial barrier.
The scalp may also be temporarily bruised or swollen, especially in hairless newborns, and the area around the eyes may be puffy.
The newborn may also have congenital dermal melanocytosis (sometimes referred to as “Mongolian spots”) (blue or blue black birthmark on the lower back), various other birthmarks, or peeling skin, particularly on the wrists, hands, ankles, and feet (as cited in Paris, Ricardo, Raymond, & Johnson, 2021).
Indigenous Perspective
Mongolian spots are most common in Indigenous people, Native Americans, Asian, Hispanic or African American descent. Unfortunately there have been cases where Indigenous women were accused of abusing their child where Child and Family Services took the baby away because of these marks.
A newborn’s genitals are enlarged and reddened, with male infants having an unusually large scrotum. The breasts may also be enlarged, even in male infants. This is caused by naturally-occurring maternal hormones and is a temporary condition.
The umbilical cord of a newborn is bluish-white in colour. After birth, the umbilical cord is normally cut, leaving a 1–2 inch stub. The umbilical stub will dry out, shrivel, darken, and spontaneously fall off within about 3 weeks. Occasionally, hospitals may apply triple dye to the umbilical stub to prevent infection, which may temporarily colour the stub and surrounding skin purple.

Figure 3.15: Lanugo on the shoulder and back of twin girls. (Image is in the public domain)

Figure 3.16: The clamping and cutting of a newborn’s umbilical cord. (Image by NNethala is licensed under CC BY-SA 3.0)
Sleep
In a typical day 24 hour period a newborn will eat and have periods of wakefulness and sleep. For many reasons this varies greatly between infants. It can take some time for an infant to fall into a somewhat recognizable and predictable schedule. A number of factors can influence this. The child’s temperament, their capacity to manage stressors, whether they are bottle fed or nursed, the environment, the experience of their families.
A newborn typically sleeps approximately 16.5 hours per 24-hour period. The infant sleeps in several periods throughout the day and night, which means they wake often throughout the day and night (Salkind, 2005, as cited in Lally & Valentine-French, 2019).

Figure 3.17: An older newborn baby. (Image by brytny.com on Unsplash)
Reflexes
Newborns are equipped with a number of reflexes, which are involuntary movements in response to stimulation. Some of the more common reflexes, such as the sucking reflex and rooting reflex, are important to feeding. The grasping and stepping reflexes are eventually replaced by more voluntary behaviours. Within the first few months of life these reflexes disappear, while other reflexes, such as the eye-blink, swallowing, sneezing, gagging, and withdrawal reflex stay with us as they continue to serve important functions (Lally & Valentine-French, 2019, p. 73).
Sensory Capacities
Throughout much of history, the newborn was considered a passive, disorganized being who possessed minimal abilities. However, current research techniques have demonstrated just how developed the newborn is with especially organized sensory and perceptual abilities.
Vision
The womb is a dark environment void of visual stimulation. Consequently, vision is the most poorly developed sense at birth and time is needed to build those neural pathways between the eye and the brain. Newborns typically cannot see further than 8 to 16 inches away from their faces, and their visual acuity is about 20/400, which means that an infant can see something at 20 feet that an adult with normal vision could see at 400 feet. Thus, the world probably looks blurry to young infants.

Figure 3.18: A newborn gazing up at a parent. (Image is in the public domain)
Hearing
The infant’s sense of hearing is very keen at birth, and the ability to hear is evidenced as soon as the 7th month of prenatal development. In fact, an infant can distinguish between very similar sounds as early as one month after birth and can distinguish between a familiar and unfamiliar voice even earlier. Infants are especially sensitive to the frequencies of sounds in human speech and prefer the exaggeration of infant-directed speech, which will be discussed later. Newborns also prefer their mother’s voices over another female when speaking the same material (DeCasper & Fifer, 1980, as cited by Paris, Ricardo, Raymond, & Johnson, 2021). Additionally, they will register in utero specific information heard from their mother’s voice (Lally & Valentine-French, 2019).
Early Hearing
DeCasper and Spence (1986), as cited by Paris, Ricardo, Raymond, & Johnson, 2021). tested 16 infants whose mothers had previously read to them prenatally. The mothers read several passages to their fetuses, including the first 28 paragraphs of The Cat in the Hat, beginning when they were 7 months pregnant. The fetuses had been exposed to the stories on average of 67 times or 3.5 hours.
During the testing, the infants were able to choose between recordings of two stories, one of which was a story their mothers read to them while in the womb, based on how fast they sucked on their pacifiers. They showed a preference for the stories that their mothers read to them while in the womb (Lally & Valentine-French, 2019).
Touch and Pain
Immediately after birth, a newborn is sensitive to touch and temperature, and is also highly sensitive to pain, responding with crying and cardiovascular responses (Balaban & Reisenauer, 2013, as cited by Paris, Ricardo, Raymond, & Johnson, 2021). Newborns who are circumcised, which is the surgical removal of the foreskin of the penis, without anesthesia experience pain as demonstrated by increased blood pressure, increased heart rate, decreased oxygen in the blood, and a surge of stress hormones (United States National Library of Medicine, 2016, as cited by Paris, Ricardo, Raymond, & Johnson, 2021). Research has demonstrated that infants who were circumcised without anesthesia experienced more pain and fear during routine childhood vaccines. Fortunately, many circumcisions are now done with the use of local anesthetics.
Taste and Smell
Studies of taste and smell demonstrate that babies respond with different facial expressions, suggesting that certain preferences are innate. Newborns can distinguish between sour, bitter, sweet, and salty flavors and show a preference for sweet flavors. Newborns also prefer the smell of their mothers. An infant, only 6 days old is significantly more likely to turn toward its own mother’s breast pad than to the breast pad of another baby’s mother (Porter, Makin, Davis, & Christensen, 1992, as cited by Paris, Ricardo, Raymond, & Johnson, 2021), and within hours of birth, an infant also shows a preference for the face of its own mother (Bushnell, 2001; Bushnell, Sai, & Mullin, 1989, as cited by Paris, Ricardo, Raymond, & Johnson, 2021).
Infants seem to be born with the ability to perceive the world in an intermodal way; that is, through stimulation from more than one sensory modality. For example, infants who sucked on a pacifier with a smooth surface preferred looking at visual models of a pacifier with a smooth surface. But those that were given a pacifier with a textured surface preferred to look at a visual model of a pacifier with a textured surface (Lally & Valentine-French, 2019, p. 76-77).

Figure 3.19: A baby sucking on a pacifier. (Image by Beeki is licensed under CC0 1.0)
A New Family
There is no doubt that becoming a parent is a life changing event and can be challenging even for those individuals who are knowledgeable about child development and have experience with children! Hormones play a critical role in pregnancy, childbirth, postpartum and lactation. The hormonal changes, the physical, emotional and psychological recovery from childbirth and delivery are experienced by the mother. In addition, the mother and baby may be figuring out nursing. According to Statistics Canada (2019), one in three women report feelings consistent with postpartum depression or an anxiety disorder. Postpartum psychosis is rarer and is experienced in about 1 in 1000 women.
In the first few days and weeks after birth the family are tasked with getting to know this brand-new human being who is unique and unlike anyone else who has ever existed…even unlike a twin sibling, if they have one! In turn the infant is learning how to live in this world…to breathe air, regulate their body temperature, communicate their needs and process information to name a few.
For a variety of reasons in Canada 30% of women giving birth are considered a lone parent. Being a lone parent can be challenging no matter the age or experience of the parent. Caring for an infant is a twenty-four hour, seven day a week job. Hopefully, the mother can access support from family members and community agencies.
The mother’s partner can play a significant role in parenting, especially during this period of adjustment. The support may involve sharing in home and child care responsibilities and accepting help from friends and family. (Canadian Mental Health Association, 2021) It is important to ensure that the mother’s basic needs are met. In the early days, some mothers may not even know what support they need while others will articulate their needs. They may want to shower, take a nap or eat a meal without holding the baby. When safe to do so, some mothers may wish to exercise by going for a run, to a gym class or yoga. This supports their overall well being. The partner can offer emotional support and respect the wishes of the mother. It is important to nurture the partnership during this adjustment period. Couples need protected time to share their feelings as they take on the new role of being a parent. Some couples protect time for ‘date nights’ to reconnect as a couple.
The Fourth Trimester
You may bump into this concept. The term was first used by Dr. Harvey Carp in 2002 to describe the first 12 weeks after an infant’s birth. During this post-partum period the mother is adjusting to the baby and the baby is adjusting to the world. In his studies of self-regulation Dr. Stuart Shanker (2016) explains that when humans began to walk upright their hands became free to engage in more complex tasks including the use of tools which in turn led to an increase in the size of the human brain. In fact, the brain became so large that it would be impossible for a human female to give birth to an infant with a fully developed brain. So, nature adapted resulting in human infants being born with brains which continue to develop particularly in the few months after birth. This is where the fourth trimester comes in. This approach encourages new parents and caregivers to respond to the infant as if they were still in utero, recognizing that some infants are more sensitive than others as far as the demands of life outside of the womb. This might mean keeping lights dimmed, reducing noise, playing soothing music etc.
All of these factors mean that new families benefit from intentional and responsive support as they navigate their new roles and responsibilities. In the past much of this support was provided through extended families, where it was not uncommon for members of different generations to live in one household. While this still occurs in some communities and cultures, in many jurisdictions this post-partum care is now offered through health care providers and community agencies. Local health units may offer resources and services. In Ontario the EarlyON Child and Family centres offer support nursing and infant care.
New parents in all populations frequently report being sleep deprived and feeling like their lives have been turned upside down. As educators it is important to show empathy and understanding to families. Recognizing the signs that a family may be struggling is an opportunity to share community resources and agencies that can offer support.
Over the last few decades labour force participation by mothers of young children has increased significantly. Statistics show that between 1976 and 2014, the share of dual-earner couples almost doubled among couple families with children, from 36% to 69%. Families with two full-time working parents now represent at least one-half of all couple families with children in Canada (Statistics Can, 2018b). This means that many mothers need to secure care for their child so that they can work or study.
In Canada, there are a number of forms of childcare. Some families may seek regulated or formal care in a licensed early learning program. In Ontario, such programs are required to comply with provincially legislated standards in the Child Care and Early Years Act (2014). In Ontario there is a critical shortage of licensed child care spaces, particularly for infants. This means that families may end up on a long waiting list even if they put their name on the list as soon as they knew they were expecting.
Another option for regulated or formal care offered in Ontario is licensed home child care. In this model a small number of children are cared for in the home of a child care provider who is affiliated with a licensed child care agency. Again, infant spaces are limited and families may end up on a waiting list for care. A large number of children in Ontario tend to be in what is referred to as informal or unregulated care. This could be a family’s choice or be because formal care was unavailable. Other families may secure care with a friend or a relative.
Summary
References
References
Canadian Mental Health Association. (2021) Post-partum depression. Retrieved from https://www.camh.ca/en/health-info/mental-illness-and-addiction-index/postpartum-depression
Exner-Pirot, H., Norbye, B. & Butler, L. (Eds). (2018). Northern and indigenous health and health care. Retrieved from http://openpress.usask.ca/northernhealthcare
Lally, M. & Valentine-French, S. (2019). Lifespan development: A psychological perspective (2nd Ed). Retrieved from http://dept.clcillinois.edu/psy/LifespanDevelopment.pdf
Government of Ontario, (2021). Infant hearing program. Retrieved from https://www.ontario.ca/page/infant-hearing-program
Mah, C. (2013). Midwifery in Canada. Retrieved from https://www.lawnow.org/midwifery-canada/
Public Health Agency of Canada. (2018). Care and labour during birth. Retrieved from https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/healthy-living/maternity-newborn-care/maternity-newborn-care-guidelines-chapter-4-eng.pdf
Shanker, S. (2016). Self-reg: How to help your child (and you) break the stress cycle and successfully engage with life. Toronto, ON: Viking, an imprint of Penguin Canada.
Statistics Canada. (2020). Live births by marital status of the mother. Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310041901
Statistics Canada. (2019). Maternal mental health in Canada. Retrieved from https://www150.statcan.gc.ca/n1/daily-quotidien/190624/dq190624b-eng.htm
Statistics Canada. (2018a). Low birth weight babies by province and territory. Retrieved from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310040401
Statistics Canda. (2018b). The surge of women in the workforce. Retrieved from https://www150.statcan.gc.ca/n1/pub/11-630-x/11-630-x2015009-eng.htm
The World Bank. (2021). Labor force, female (% of total labor force). Retrieved from https://data.worldbank.org/indicator/SL.TLF.TOTL.FE.ZS?locations=CA

