4.10 MMT (Methadone Maintenance Treatment Case Management)
In this chapter we look through a Case Management lens and examine a variety of Withdrawal Management Programs that include RAAM clinics, OAT (Opioid Agonist Treatment) and MMT (Methadone Maintenance Treatment) including Suboxone. Each area will have different components of Case Management.
MMT (Methadone Maintenance Treatment)

Methadone is a medication primarily used to treat chronic pain and as a treatment for opioid use disorder. It is a controlled substance that is regulated under the Controlled Drugs and Substances Act (CDSA), and the Narcotic Control Regulations (NCR).
In the past, practitioners were required to obtain an exemption from Health Canada before they could prescribe, sell, provide or administer methadone.
Methadone is a long-acting opiate, which is substituted for short acting opiates like fentanyl, Percocet, oxycodone, and heroin (Centre for Addiction and Mental Health, 2021b). This type of OAT manages the withdrawal symptoms a person experiences as withdrawal from opiates can be physically painful. It can also be emotionally distressing, particularly if the substance is being used as a coping tool. Evidence from research around the globe has demonstrated that methadone is an effective treatment; it can help people with an opioid addiction in more ways than one (Centre for Addiction and Mental Health, 2021).
2 minutes – Neuroscience on Methadone
2-Minute Neuroscience: Methadone. By: Neuroscientifically Challenged. Methadone is commonly used to treat opioid use disorder even though its pharmacological action is very similar to that of other opioids like morphine. In this video, I discuss the qualities that make methadone an effective treatment for opioid addiction, along with how it acts to reduce the risks associated with opioid abuse.
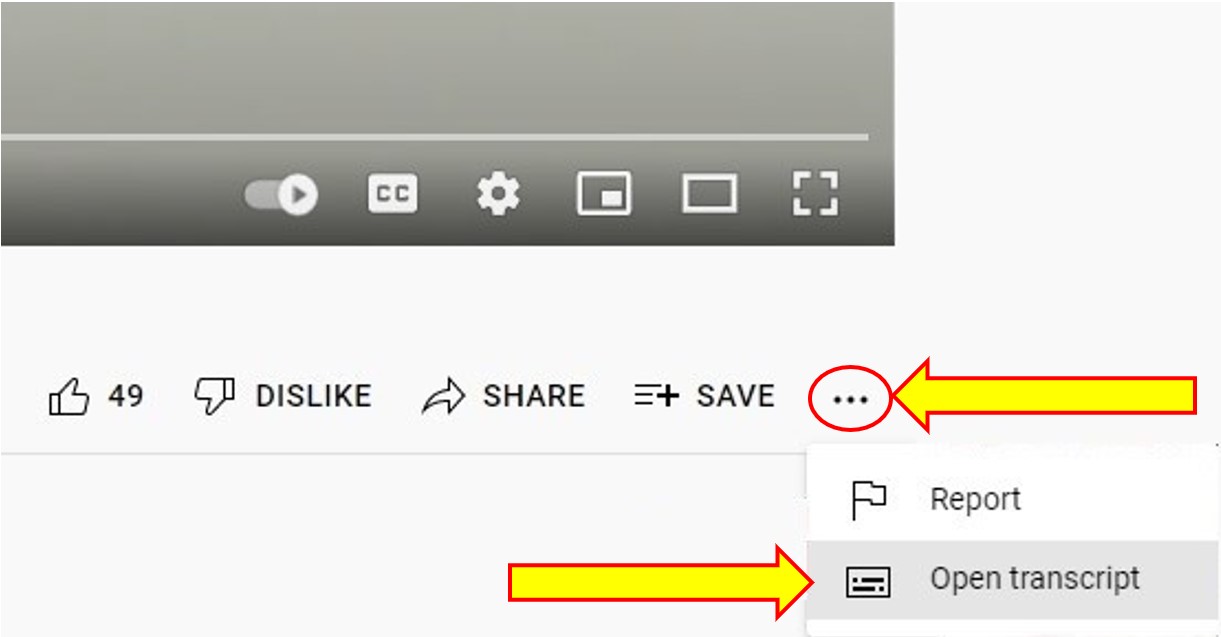
Transcript
To Access the Video Transcript:
1. Click on “YouTube” on the bottom-right of the video. This will take you directly to the YouTube video.
2. Click on the More Actions icon (represented by three horizontal dots)
3. Click on “Open Transcript”
Suboxone (Buprenorphine/Naloxone)

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms.
Is Suboxone legal in Canada?
Health Canada has authorized 2 dosage forms of SUBOXONE (buprenorphine and naloxone), a sublingual tablet and soluble film, that are not bioequivalent at all doses and routes of administration.
Important Information:
MMT (Methadone Maintenance Treatment) Case Management in Ontario
The Ontario Ministry of Health and Long-Term Care has recognized the importance of case management in MMT (Methadone Maintenance Treatment Case Management). Because of the multi-faceted issues involved in MMT, effective case management is critical for client success. It is necessary to have many skills to be able to work effectively in MMT as a case manager. The case manager provides the link between the many resources, services and roles involved in the MMT program.
When we look at the different components/areas that are important as a MMT Case Manager, we need to take into consideration:
- Role of Case Management in MMT
- Who’s on the MMT
- Assessment and Client Matching (Intensity of Case Management Services)
- Core Knowledge, Competencies and Training
- Confidentiality
- the Client consultation
- Co-ordination of continuity of care and support
- Crisis/drop-in
- Case conferences
- Advocacy
- Counselling
- Treatment planning
- Effective communication skills
For More Information on Methadone Maintenance Treatment – Case Management (CAMH)
Food for Thought
Creating and implementing standardized and accredited training in the role and functions of case manager is difficult in Canada. Substance use counsellors and case managers are not always accredited and have various levels of education. Methadone is a regulated and controlled medication, but there are many laws, regulations and standings in Ontario for prescribing, distributing and supporting.
The better informed and trained a case manager is about these policies and laws, the more support, advocacy and assistance they can provide effectively to a client. Since case managers are client advocates, they need to translate and clarify programs, systems, services, resources, and other information for their clients.
Clients’ Handbook – CAMH
Education for everyone, even clients, is mandatory for a standard of care. Clients’ Handbook: Making the Choice, Making it Work – CAMH
This handbook is to provide clients with answers to the questions they have about participating in an MMT program. Reading this handbook will help you better understand a client’s perspective on MMT.
For More Information
Methadone Maintenance Treatment (MMT) is a very broad term that covers a variety of components and supports. At its core, it usually involves the prescription of methadone to long-term opioid users. Methadone is a synthetic opioid which was created to assist in the withdrawal and long-term recovery from opioid addiction. It has been found to be very effective when used for tapering and stabilizing clients and for chronic pain management.
In Canada, MMT programs generally include (in addition to methadone):
- Medical care
- Counselling and support
- Treatment for other substance use
- Mental health services
- Community-based services and supports (e.g. housing, transportation, employment, school, life skills)
Roles involved in MMT
MMT also involves many professionals including medical doctors, nurses, social workers, psychiatrists, pharmacists and case managers who are specifically trained to work with this population. Learning about each professional’s roles and expectations will assist the client as well as the case manager.
Challenges in MMT Programs
There are many challenges and gaps in MMT programs, including:
- Distribution of services, such as not having access to medication during holidays
- Fewer programs for rural and suburban communities
- Access to methadone while in hospital (for other medical issues)
- Access to newer drug treatments (for example, Ontario health system pays for methadone, but not suboxone, which is a newer drug for treating opioid addiction)
- Lack of education for professionals
- Stigma within health, social work and general communities
Learning Activity
As a case manager for MMT, choose three of the above listed skills, experiences, or competencies that you feel you have and rate your skill level.
| Skills/Competencies | 0 (none) | 1 (little) | 2 (average) | 3 (above average) | 4 (excellent) |
|---|---|---|---|---|---|
| Skill 1 | |||||
| Skill 2 | |||||
| Skill 3 |
What do you need to do, learn, or practice to move each of these three skills to a higher skill level?
Rapid Access to Addictions Medicine (RAAM) Clinics
The RAAM Clinic is an easy to access walk-in/drop-in clinic that people can visit to get help for substance use without an appointment or formal referral. RAAM Clinics are attached to hospitals and have a multi-disciplinary team. RAAM Clinics are situated in most provinces across Canada. Services are provided on a first come, first served basis, with some prioritization by clinic staff based on urgency. Contact the closest clinic to find out what their hours and days are.
What is a RAAM clinic and who is it for?
RAAM clinics are for:
- people looking to get help with high risk substance use and addictions
- interested in trying medical assistance to reduce or stop their substance use
- experience frequent intoxication or overdose symptoms, as well as unpleasant withdrawal symptoms when attempting to reduce or stop their substance use
- people who have substance-related health issues, such as hepatitis, pancreatitis, or infections, among others..
RAAM clinics are not for people who:
- need urgent medical attention for urgent physical problems or mental health symptoms such as psychosis (paranoia, delusions, hallucinations) or agitation
- active risk of harm to self or others
- requiring police/security involvement.
The people working at these clinics know how difficult it is to ask for help. You don’t need an appointment to go to the clinic – just show up during clinic hours with your Health card.
It is that medical treatment for problematic substance use is safe and effective.
What happens when you go to a RAAM clinic?

The clinic team will ask you about your history of substance use:
- when and how you started using
- how much and how frequently you use
- how it may impact your life and responsibilities
The RAAM clinic team then recommends what treatment will likely work best for you. There are four options:
- Advice – Many people who have to go to the hospital for a substance-related problem are injured as a result of using too much. In these cases, the RAAM clinic team will provide you with advice on how to make choices that will minimize the risks of substance use, such as tips on how to pace your use and situations to avoid.
- Counselling – The RAAM clinic team may refer you to counselling as part of your treatment. Counselling programs can include education on substances and healthy lifestyle choice, group and individual therapy sessions, help with developing coping skills, cognitive behavioural therapy, and peer support groups. The team will work with you to determine what form of counselling would be most helpful for you.
- Medications – Addiction to some substances, such as alcohol or opioids, can be treated with a medication that will help to lessen cravings, as well as the withdrawal symptoms that may accompany your early days of sobriety. Medication usually makes other types of treatment much more effective and reduces the risk of relapse. These medications are safe, effective, and non-addictive. The team will discuss your options with you.
- Support – If you’re feeling anxious or hesitant about going to the RAAM clinic, consider bringing a supportive person with you. Changing your substance use can be very difficult, and having someone with you while you speak to the team may make you feel less overwhelmed and less alone.

IMPORTANT – If you are seeking treatment for opioid addiction, abstinence (including withdrawal management/detoxification) is NOT recommended. Opioid Agonist Treatment (OAT) (the use of long-acting medications to treat withdrawal and prevent relapse) is recommended as a safe and effective way to treat your opioid addiction.
When you begin your recovery from opioid addiction, abstinence can place you at higher risk of overdose, medical harms and death. You are welcome to attend a RAAM clinic or contact other OAT providers to discuss your options.
YOU SHOULD KNOW
Individuals do not have to be substance-free for any length of time to access RAAM services. However, they must be able to have an informed conversation about treatment, understanding the risks and benefits of treatment options. If a person is too intoxicated to have an informed conversation, they may be asked to return at a later date or referred to another community service.
If an individual with opioid use disorder is to receive Opioid Agonist Treatment (OAT) with buprenorphine/naloxone (Suboxone), the time from last opioid use will factor into the decision on how to safely start the medication.There is no specific timeframe of required abstinence from opioids before attending RAAM
OPIOID AGONIST THERAPY (OAT)

How does Opioid Agonist Therapy (OAT) Work?
(OAT) is an effective treatment for addiction to opioid drugs such as heroin, oxycodone, hydromorphone (Dilaudid), fentanyl and Percocet. The therapy involves taking the opioid agonists methadone (Methadose) or buprenorphine (Suboxone). These medications work to prevent withdrawal and reduce cravings for opioid drugs. People who are addicted to opioid drugs can take OAT to help stabilize their lives and to reduce the harms related to their drug use
When a person is addicted to shorter-acting opioids, a long-acting opioid (methadone and buprenorphine) are used. The long-acting means that the drug works for a longer period of time by acting more slowly in the body. This prevents withdrawal for 24 to 36 hours without causing a person to get high. OAT reduces or eliminate cravings for opioid drugs. When combined with support, such as individual or group counselling, there are best outcomes.
Usage of opiates in Canada is being called a public health crisis by both advocates of substance use treatment programs (Canadian Centre on Substance Use and Addiction, 2021) and the Government of Canada (2021b). The Government has recognized this crisis has only worsened during the Covid-19 pandemic. Many urban and rural communities across Canada have reported a record number of opioid-related deaths, emergency calls and hospitalizations (Government of Canada, 2021b). While medications like medical grade heroin and hydromorphone can treat opiate use disorders, there are other medications that have also positively impacted the lives of people who use opiates.
More Information:
References
- Figure 4.10.1 – Pixabay License
- Figure 4.10.2, 4.10.3, 4.10.4, 4.11]0.5, 4.10.6, – Unsplash License
- 2-Minute Neuroscience: Methadone. (2019, June 7). [Video]. YouTube. https://www.youtube.com/watch?v=dw6laQ4-Zgs&t=1s
- CAMH. (n.d.-b). Opioid Agonist Therapy. Retrieved March 26, 2022, from https://www.camh.ca/-/media/files/oat-info-for-clients.pdf
- Shared Health Manitoba. (n.d.). Rapid Access to Addictions Medicine (RAAM) Clinic. Retrieved March 29, 2022, from https://sharedhealthmb.ca/services/mental-health/raam-clinic/

