Environmental hazards for humans
Key Concepts
After completing this chapter, you will be able to
- Describe some of the most important environmental threats to human health
- Consider the links between poverty, race, and environmental health threats
- Recall some of the major environmental contaminants
- Describe some of the processes that can reduce environmental threats to human health.
The Impacts of Environmental Conditions
Our industrialized society dumps huge amounts of pollutants and toxic wastes into the earth’s biosphere without fully considering the consequences. Such actions seriously degrade the health of the earth’s ecosystems, and this degradation ultimately affects the health and well-being of human populations.
For most of human history, biological agents were the most significant factor in health. These included pathogenic (disease causing) organisms such as bacteria, viruses, protozoa, and internal parasites. In modern times, cardiovascular diseases, cancer, and accidents are the leading killers in most parts of the world. However, infectious diseases still cause about 22 million deaths a year, mostly in undeveloped countries. These diseases include: tuberculosis, malaria, pneumonia, influenza, whooping cough, dysentery and Acquired Immune Deficiency Syndrome (AIDS). Most of those affected are children. Malnutrition, unclean water, poor sanitary conditions and lack of proper medical care all play roles in these deaths. Compounding the problems of infectious diseases are factors such as drug-resistant pathogens, insecticide resistant carriers, and overpopulation. Overuse of antibiotics have allowed pathogens to develop a resistance to drugs. For example, tuberculosis (TB) was nearly eliminated in most parts of the world, but drug-resistant strains have now reversed that trend. Another example is malaria. The insecticide DDT (Dichlorodiphenyltrichloroethane) was widely used to control malaria-carrying mosquito populations in tropical regions. However, after many years the mosquitoes developed a natural resistance to DDT and again spread the disease widely. Anti-malarial medicines were also over-prescribed, which allowed the malaria pathogen to become drug-resistant.
Chemical agents also have significant effects on human health. Toxic heavy metals, dioxins, pesticides, and endocrine disrupters are examples of these chemical agents. Heavy metals (e.g., mercury, lead, & cadmium) are typically produced as by-products of mining and manufacturing processes. All of them biomagnify (become more concentrated in species with increasing food chain level). For example, mercury from polluted water can accumulate in swordfish to levels toxic to humans. When toxic heavy metals get into the body, they accumulate in tissues and may eventually cause sickness or death. Studies show that people with above-average lead levels in their bones have an increased risk of developing attention deficit disorder and aggressive behavior. Lead can also damage brain cells and affect muscular coordination.
Environmental Persistence of DDT
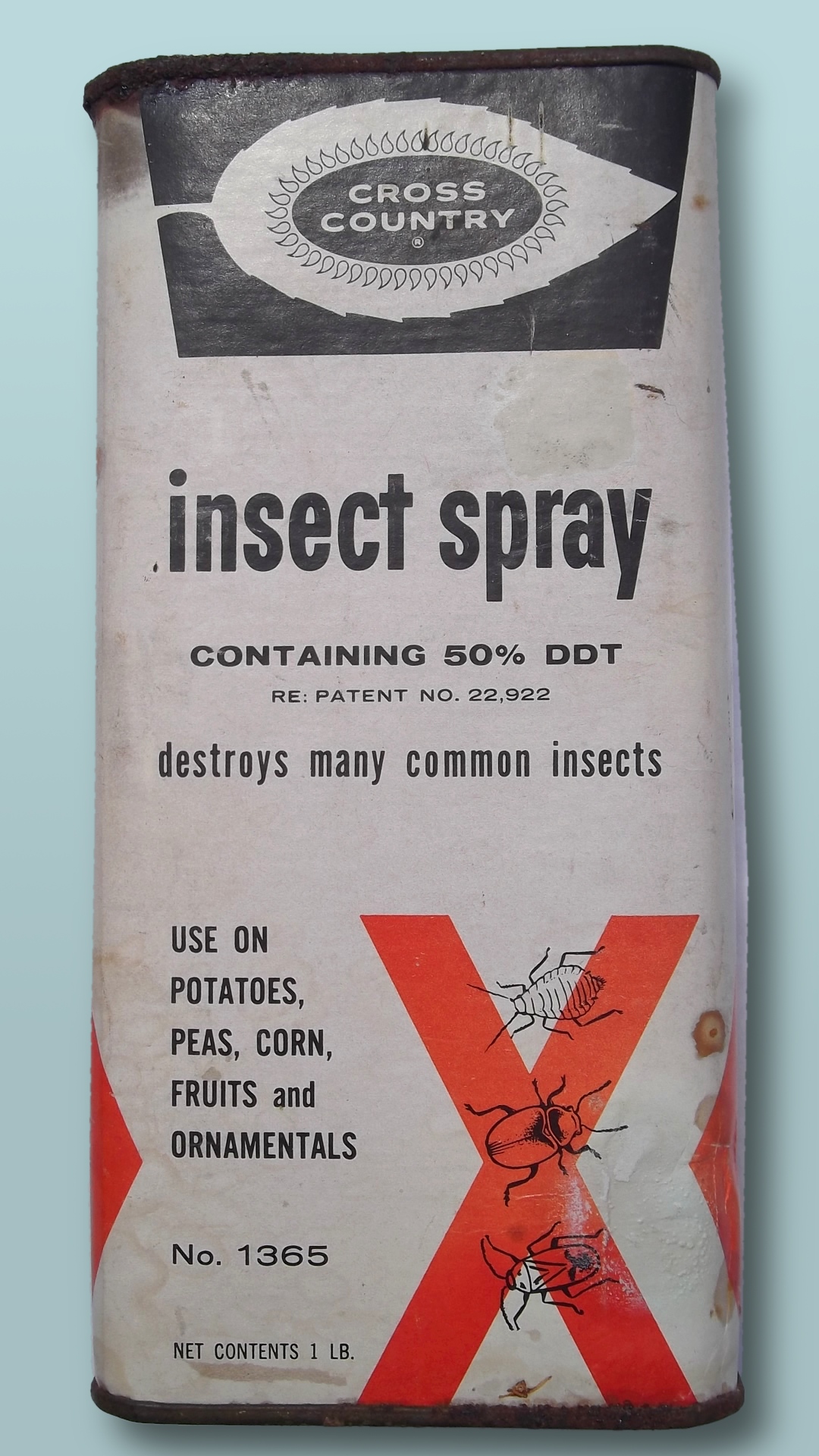
The pesticide DDT was widely used for decades. It was seen as an ideal pesticide because it is inexpensive and breaks down slowly in the environment. Unfortunately, the latter characteristic allows it to biomagnify through the food chain. Populations of bird species at the top of the food chain, e.g., eagles and pelicans, are greatly affected by DDT in the environment. When these birds have sufficient levels of DDT, the shells of their eggs are so thin that they break, making reproduction impossible. After DDT was banned in the United States in 1972, affected bird populations made noticeable recoveries, including the iconic bald eagle.
Attribution
Essentials of Environmental Science by Kamala Doršner is licensed under CC BY 4.0
Science can be defined as the systematic examination of the structure and functioning of the natural world, including both its physical and biological attributes. Science is also a rapidly expanding body of knowledge, whose ultimate goal is to discover the simplest general principles that can explain the enormous complexity of nature. These principles can be used to gain insights about the of the natural world and to make predictions about future change.
Environmental Health
Environmental health is concerned with preventing disease, death and disability by reducing exposure to adverse environmental conditions and promoting behavioral change. It focuses on the direct and indirect causes of diseases and injuries, and taps resources inside and outside the health care system to help improve health outcomes.

Poverty, Health and Environment
Environmental health risks can be grouped into two broad categories. Traditional hazards are related to poverty and the lack of development and mostly affect developing countries and poor people. Their impact exceeds that of modern health hazards by 10 times in Africa, 5 times in Asian countries (except for China), and 2.5 times in Latin America and Middle East (Figure 1). Water-related diseases caused by inadequate water supply and sanitation impose an especially large health burden in Africa, Asia, and the Pacific region. In India alone, over 700,000 children under 5 die annually from diarrhea. In Africa, malaria causes about 500,000 deaths annually. More than half of the world’s households use unprocessed solid fuels, particularly biomass (crop residues, wood, and dung) for cooking and heating in inefficient stoves without proper ventilation, exposing people—mainly poor women and children—to high levels of indoor air pollution(IAP). IAP causes about 2 million deaths in each year.

Modern hazards, caused by technological development, prevail in industrialized countries where exposure to traditional hazards is low. The contribution of modern environmental risks to the disease burden in most developing countries is similar to – and in quite a few countries, greater than – that in rich countries. Urban air pollution, for example, is highest in parts of China, India and some cities in Asia and Latin America. Poor people increasingly experience a “double burden” of traditional and modern environmental health risks. Their total burden of illness and death from all causes per million people is about twice that in rich countries, and the disease burden from environmental risks is 10 times greater.
Environmental Health and Child Survival

Worldwide, the top killers of children under five are acute respiratory infections (from indoor air pollution); diarrheal diseases (mostly from poor water, sanitation, and hygiene); and infectious diseases such as malaria. Children are especially susceptible to environmental factors that put them at risk of developing illness early in life. Malnutrition (the condition that occurs when body does not get enough nutrients) is an important contributor to child mortality—malnutrition and environmental infections are inextricably linked. The World Health Organization (WHO) recently concluded that about 50% of the consequences of malnutrition are in fact caused by inadequate water and sanitation provision and poor hygienic practices.
Poor Water and Sanitation Access
With 1.1 billion people lacking access to safe drinking water and 2.6 billion without adequate sanitation, the magnitude of the water and sanitation problem remains significant. Each year contaminated water and poor sanitation contribute to 5.4 billion cases of diarrhea worldwide and 1.6 million deaths, mostly among children under the age of five. Intestinal worms, which thrive in poor sanitary conditions, infect close to 90 percent of children in the developing world and, depending on the severity of the infection may lead to malnutrition, anemia, or stunted growth. About 6 million people are blind from trachoma, a disease caused by the lack of clean water combined with poor hygiene practices.
Indoor Air Pollution
Indoor air pollution—a much less publicized source of poor health—is responsible for more than 1.6 million deaths per year and for 2.7% of global burden of disease. It is estimated that half of the world’s population, mainly in developing countries, uses solid fuels (biomass and coal) for household cooking and space heating. Cooking and heating with such solid fuels on open fires or stoves without chimneys lead to indoor air pollution and subsequently, respiratory infections. Exposure to these health-damaging pollutants is particularly high among women and children in developing countries, who spend the most time inside the household. As many as half of the deaths attributable to indoor use of solid fuel are of children under the age of five.
Malaria
Approximately 40% of the world’s people—mostly those living in the world’s poorest countries—are at risk from malaria. Malaria is an infectious disease spread by mosquitoes but caused by a single-celled parasite called Plasmodium. Every year, more than 200 million people become infected with malaria and about 430,000 die, with most cases and deaths found in Sub-Saharan Africa. However, Asia, Latin America, the Middle East, and parts of Europe are also affected. Pregnant women are especially at high risk of malaria. Non-immune pregnant women risk both acute and severe clinical disease, resulting in fetal loss in up to 60% of such women and maternal deaths in more than 10%, including a 50% mortality rate for those with severe disease. Semi-immune pregnant women with malaria infection risk severe anemia and impaired fetal growth, even if they show no signs of acute clinical disease. An estimated 10,000 women and 200,000 infants die annually as a result of malaria infection during pregnancy.
Emerging Diseases
Emerging and re-emerging diseases have been defined as infectious diseases of humans whose occurrence during the past two decades has substantially increased or threatens to increase in the near future relative to populations affected, geographic distribution, or magnitude of impacts. Examples include Ebola virus, West Nile virus, Zika virus, sudden acute respiratory syndrome (SARS), H1N1 influenza; swine and avian influenza (swine, bird flu), HIV, and a variety of other viral, bacterial, and protozoal diseases.
A variety of environmental factors may contribute to re-emergence of a particular disease, including temperature, moisture, human food or animal feed sources, etc. Disease re-emergence may be caused by the coincidence of several of these environmental and/or social factors to allow optimal conditions for transmission of the disease.
Ebola, previously known as Ebola hemorrhagic fever, is a rare and deadly disease caused by infection with one of the Ebola virus strains. Ebola can cause disease in humans and nonhuman primates. The 2014 Ebola epidemic is the largest in history (with over 28,000 cases and 11,302 deaths), affecting multiple countries in West Africa. There were a small number of cases reported in Nigeria and Mali and a single case reported in Senegal; however, these cases were contained, with no further spread in these countries.
The HIV/AIDS epidemic has spread with ferocious speed. Virtually unknown 20 years ago, HIV has infected more than 60 million people worldwide. Each day, approximately 14,000 new infections occur, more than half of them among young people below age 25. Over 95 percent of PLWHA (People Living With HIV/AIDS) are in low- and middle- income countries. More than 20 million have died from AIDS, over 3 million in 2002 alone. AIDS is now the leading cause of death in Sub-Saharan Africa and the fourth-biggest killer globally. The epidemic has cut life expectancy by more than 10 years in several nations.
It seems likely that a wide variety of infectious diseases have affected human populations for thousands of years emerging when the environmental, host, and agent conditions were favorable. Expanding human populations have increased the potential for transmission of infectious disease as a result of close human proximity and increased likelihood for humans to be in “the wrong place at the right time” for disease to occur (eg, natural disasters or political conflicts). Global travel increases the potential for a carrier of disease to transmit infection thousands of miles away in just a few hours, as evidenced by WHO precautions concerning international travel and health.
Antibiotic Resistance
Antibiotics and similar drugs, together called antimicrobial agents, have been used for the last 70 years to treat patients who have infectious diseases. Since the 1940s, these drugs have greatly reduced illness and death from infectious diseases. However, these drugs have been used so widely and for so long that the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective. Antibiotic resistance occurs when bacteria change in a way that reduces the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The bacteria survive and continue to multiply, causing more harm (Figure 3 below).

New forms of antibiotic resistance can cross international boundaries and spread between continents with ease. Many forms of resistance spread with remarkable speed. Each year in the United States, at least 2 million people acquire serious infections with bacteria that are resistant to one or more of the antibiotics designed to treat those infections. At least 23,000 people die each year in the US as a direct result of these antibiotic-resistant infections. Many more die from other conditions that were complicated by an antibiotic-resistant infection. The use of antibiotics is the single most important factor leading to antibiotic resistance around the world.

Antibiotics are among the most commonly prescribed drugs used in human medicine, but up to 50% of all the antibiotics prescribed for people are not needed or are not optimally effective as prescribed.
During recent years, there has been growing concern over methicillin-resistant Staphylococcus aureus (MRSA), a bacterium that is resistant to many antibiotics. In the community, most MRSA infections are skin infections. In medical facilities, MRSA causes life-threatening bloodstream infections, pneumonia and surgical site infections.
Suggested Supplementary Reading:
Koch, B.J. et al. 2017. Food-animal production and the spread of antibiotic resistance: the role of ecology. Frontiers in Ecology and the Environment (15)6: 309-318.
Notable Excerpts:
“Antibiotic use in food animals is correlated with antibiotic resistance among bacteria affecting human populations.” p. 311
“Microbial genes encoding antibiotic resistance have moved between the food-animal and human health sectors, resulting in illnesses that could not be treated by antibiotics.” p. 312
ATTRIBUTION
Essentials of Environmental Science by Kamala Doršner is licensed under CC BY 4.0. Modified from the original by Matthew R. Fisher.
Environmental Toxicology
Environmental toxicology is the scientific study of the health effects associated with exposure to toxic chemicals (Table 1) occurring in the natural, work, and living environments. The term also describes the management of environmental toxins and toxicity, and the development of protections for humans and the environment.
| 2013 RANK |
NAME |
| 1 | ARSENIC |
| 2 | LEAD |
| 3 | MERCURY |
| 4 | VINYL CHLORIDE |
| 5 | POLYCHLORINATED BIPHENYLS |
| 6 | BENZENE |
| 7 | CADMIUM |
| 8 | BENZO(A)PYRENE |
| 9 | POLYCYCLIC AROMATIC HYDROCARBONS |
| 10 | BENZO(B)FLUORANTHENE |
| 11 | CHLOROFORM |
| 12 | AROCLOR 1260 |
| 13 | DDT, P,P’- |
| 14 | AROCLOR 1254 |
| 15 | DIBENZO(A,H)ANTHRACENE |
| 16 | TRICHLOROETHYLENE |
| 17 | CHROMIUM, HEXAVALENT |
| 18 | DIELDRIN |
| 19 | PHOSPHORUS, WHITE |
| 20 | HEXACHLOROBUTADIENE |
Routes of Exposure to Chemicals
In order to cause health problems, chemicals must enter your body. There are three main “routes of exposure,” or ways a chemical can get into your body.
- Breathing (inhalation): Breathing in chemical gases, mists, or dusts that are in the air.
- Skin or eye contact: Getting chemicals on the skin, or in the eyes. They can damage the skin, or be absorbed through the skin into the bloodstream.
- Swallowing (ingestion): This can happen when chemicals have spilled or settled onto food, beverages, cigarettes, beards, or hands.
Once chemicals have entered your body, some can move into your bloodstream and reach internal “target” organs, such as the lungs, liver, kidneys, or nervous system.
What Forms do Chemicals Take?
Chemical substances can take a variety of forms. They can be in the form of solids, liquids, dusts, vapors, gases, fibers, mists and fumes. The form a substance is in has a lot to do with how it gets into your body and what harm it can cause. A chemical can also change forms. For example, liquid solvents can evaporate and give off vapors that you can inhale. Sometimes chemicals are in a form that can’t be seen or smelled, so they can’t be easily detected.
What Health Effects Can Chemicals Cause?
An acute effect of a contaminant (The term “contaminant” means hazardous substances, pollutants, pollution, and chemicals) is one that occurs rapidly after exposure to a large amount of that substance. A chronic effect of a contaminant results from exposure to small amounts of a substance over a long period of time. In such a case, the effect may not be immediately obvious. Chronic effect are difficult to measure, as the effects may not be seen for years. Long-term exposure to cigarette smoking, low level radiation exposure, and moderate alcohol use are all thought to produce chronic effects.
For centuries, scientists have known that just about any substance is toxic in sufficient quantities. For example, small amounts of selenium are required by living organisms for proper functioning, but large amounts may cause cancer. The effect of a certain chemical on an individual depends on the dose (amount) of the chemical. This relationship is often illustrated by a dose-response curve which shows the relationship between dose and the response of the individual. Lethal doses in humans have been determined for many substances from information gathered from records of homicides, accidental poisonings, and testing on animals.
A dose that is lethal to 50% of a population of test animals is called the lethal dose-50% or LD-50. Determination of the LD-50 is required for new synthetic chemicals in order to give a measure of their toxicity. A dose that causes 50% of a population to exhibit any significant response (e.g., hair loss, stunted development) is referred to as the effective dose-50% or ED-50. Some toxins have a threshold amount below which there is no apparent effect on the exposed population.
Environmental Contaminants
The contamination of the air, water, or soil with potentially harmful substances can affect any person or community. Contaminants (Table 2) are often chemicals found in the environment in amounts higher than what would be there naturally. We can be exposed to these contaminants from a variety of residential, commercial, and industrial sources. Sometimes harmful environmental contaminants occur biologically, such as mold or a toxic algae bloom.
| Contaminant | Definition |
| Carcinogen | An agent which may produce cancer (uncontrolled cell growth), either by itself or in conjunction with another substance. Examples include formaldehyde, asbestos, radon, vinyl chloride, and tobacco. |
| Teratogen |
A substance which can cause physical defects in a developing embryo. Examples include alcohol and cigarette smoke. |
| Mutagen | A material that induces genetic changes (mutations) in the DNA. Examples include radioactive substances, x-rays and ultraviolet radiation. |
| Neurotoxicant |
A substance that can cause an adverse effect on the chemistry, structure or function of the nervous system. Examples include lead and mercury. |
|
Endocrine disruptor |
A chemical that may interfere with the body’s endocrine system and produce adverse developmental, reproductive, neurological, and immune effects in both humans and wildlife. A wide range of substances, both natural and man-made, are thought to cause endocrine disruption, including pharmaceuticals, dioxin and dioxin-like compounds, arsenic, polychlorinated biphenyls (PCBs), DDT and other pesticides, and plasticizers such as bisphenol A (BPA). |
An Overview of Some Common Contaminants
Arsenic is a naturally occurring element that is normally present throughout our environment in water, soil, dust, air, and food. Levels of arsenic can regionally vary due to farming and industrial activity as well as natural geological processes. The arsenic from farming and smelting tends to bind strongly to soil and is expected to remain near the surface of the land for hundreds of years as a long-term source of exposure. Wood that has been treated with chromated copper arsenate (CCA) is commonly found in decks and railing in existing homes and outdoor structures such as playground equipment. Some underground aquifers are located in rock or soil that has naturally high arsenic content.
Most arsenic gets into the body through ingestion of food or water. Arsenic in drinking water is a problem in many countries around the world, including Bangladesh, Chile, China, Vietnam, Taiwan, India, and the United States. Arsenic may also be found in foods, including rice and some fish, where it is present due to uptake from soil and water. It can also enter the body by breathing dust containing arsenic. Researchers are finding that arsenic, even at low levels, can interfere with the body’s endocrine system. Arsenic is also a known human carcinogen associated with skin, lung, bladder, kidney, and liver cancer.
Mercury is a naturally occurring metal, a useful chemical in some products, and a potential health risk. Mercury exists in several forms; the types people are usually exposed to are methylmercury and elemental mercury. Elemental mercury at room temperature is a shiny, silver-white liquid which can produce a harmful odorless vapor. Methylmercury, an organic compound, can build up in the bodies of long-living, predatory fish. To keep mercury out of the fish we eat and the air we breathe, it’s important to take mercury-containing products to a hazardous waste facility for disposal. Common products sold today that contain small amounts of mercury include fluorescent lights and button-cell batteries.
Although fish and shellfish have many nutritional benefits, consuming large quantities of fish increases a person’s exposure to mercury. Pregnant women who eat fish high in mercury on a regular basis run the risk of permanently damaging their developing fetuses. Children born to these mothers may exhibit motor difficulties, sensory problems and cognitive deficits. Figure 1 identifies the typical (average) amounts of mercury in commonly consumed commercial and sport-caught fish.

Bisphenol A (BPA) is a chemical produced in large quantities for use primarily in the production of polycarbonate plastics and epoxy resins. Polycarbonate plastics have many applications including use in some food and drink packaging, e.g., water and infant bottles, compact discs, impact-resistant safety equipment, and medical devices. Epoxy resins are used as lacquers to coat metal products such as food cans, bottle tops, and water supply pipes. Some dental sealants and composites may also contribute to BPA exposure. The primary source of exposure to BPA for most people is through the diet. Bisphenol A can leach into food from the protective internal epoxy resin coatings of canned foods and from consumer products such as polycarbonate tableware, food storage containers, water bottles, and baby bottles. The degree to which BPA leaches from polycarbonate bottles into liquid may depend more on the temperature of the liquid or bottle, than the age of the container. BPA can also be found in breast milk.
What can I do to prevent exposure to BPA?
Some animal studies suggest that infants and children may be the most vulnerable to the effects of BPA. Parents and caregivers, can make the personal choice to reduce exposures of their infants and children to BPA:
- Don’t microwave polycarbonate plastic food containers. Polycarbonate is strong and durable, but over time it may break down from over use at high temperatures.
- Plastic containers have recycle codes on the bottom. Some, but not all, plastics that are marked with recycle codes 3 or 7 may be made with BPA.
- Reduce your use of canned foods.
- When possible, opt for glass, porcelain or stainless steel containers, particularly for hot food or liquids.
- Use baby bottles that are BPA free.
Phthalates are a group of chemicals used to soften and increase the flexibility of plastic and vinyl. Polyvinyl chloride is made softer and more flexible by the addition of phthalates. Phthalates are used in hundreds of consumer products. Phthalates are used in cosmetics and personal care products, including perfume, hair spray, soap, shampoo, nail polish, and skin moisturizers. They are used in consumer products such as flexible plastic and vinyl toys, shower curtains, wallpaper, vinyl miniblinds, food packaging, and plastic wrap. Exposure to low levels of phthalates may come from eating food packaged in plastic that contains phthalates or breathing dust in rooms with vinyl miniblinds, wallpaper, or recently installed flooring that contain phthalates. We can be exposed to phthalates by drinking water that contains phthalates. Phthalates are suspected to be endocrine disruptors.
Lead is a metal that occurs naturally in the rocks and soil of the earth’s crust. It is also produced from burning fossil fuels such as coal, oil, gasoline, and natural gas; mining; and manufacturing. Lead has no distinctive taste or smell. The chemical symbol for elemental lead is Pb. Lead is used to produce batteries, pipes, roofing, scientific electronic equipment, military tracking systems, medical devices, and products to shield X-rays and nuclear radiation. It is used in ceramic glazes and crystal glassware. Because of health concerns, lead and lead compounds were banned from house paint in 1978; from solder used on water pipes in 1986; from gasoline in 1995; from solder used on food cans in 1996; and from tin-coated foil on wine bottles in 1996. The U.S. Food and Drug Administration has set a limit on the amount of lead that can be used in ceramics.
Lead and lead compounds are listed as “reasonably anticipated to be a human carcinogen”. It can affect almost every organ and system in your body. It can be equally harmful if breathed or swallowed. The part of the body most sensitive to lead exposure is the central nervous system, especially in children, who are more vulnerable to lead poisoning than adults. A child who swallows large amounts of lead can develop brain damage that can cause convulsions and death; the child can also develop blood anemia, kidney damage, colic, and muscle weakness. Repeated low levels of exposure to lead can alter a child’s normal mental and physical growth and result in learning or behavioral problems. Exposure to high levels of lead for pregnant women can cause miscarriage, premature births, and smaller babies. Repeated or chronic exposure can cause lead to accumulate in your body, leading to lead poisoning.

Formaldehyde is a colorless, flammable gas or liquid that has a pungent, suffocating odor. It is a volatile organic compound, which is an organic compound that easily becomes a vapor or gas. It is also naturally produced in small, harmless amounts in the human body. The primary way we can be exposed to formaldehyde is by breathing air containing it. Releases of formaldehyde into the air occur from industries using or manufacturing formaldehyde, wood products (such as particle-board, plywood, and furniture), automobile exhaust, cigarette smoke, paints and varnishes, and carpets and permanent press fabrics. Nail polish, and commercially applied floor finish emit formaldehyde.
In general, indoor environments consistently have higher concentrations than outdoor environments, because many building materials, consumer products, and fabrics emit formaldehyde. Levels of formaldehyde measured in indoor air range from 0.02–4 parts per million (ppm). Formaldehyde levels in outdoor air range from 0.001 to 0.02 ppm in urban areas.
Radiation
Radiation is energy given off by atoms and is all around us. We are exposed to radiation every day from natural sources like soil, rocks, and the sun. We are also exposed to radiation from man-made sources like medical X-rays and smoke detectors. We’re even exposed to low levels of radiation on cross-country flights, from watching television, and even from some construction materials. You cannot see, smell or taste radiation. Some types of radioactive materials are more dangerous than others. So it’s important to carefully manage radiation and radioactive substances to protect health and the environment.
Radon is a colorless, odorless radioactive gas. It comes from the natural decay of uranium or thorium found in nearly all soils. It typically moves up through the ground and into the home through cracks in floors, walls and foundations. It can also be released from building materials or from well water. Radon breaks down quickly, giving off radioactive particles. Long-term exposure to these particles can lead to lung cancer. Radon is the leading cause of lung cancer among nonsmokers, according to the U.S. Environmental Protection Agency, and the second leading cause behind smoking.
Bioremediation
Bioremediation is a waste management technique that involves the use of organisms such as plants, bacteria, and fungi to remove or neutralize pollutants from a contaminated site. According to the United States EPA, bioremediation is a “treatment that uses naturally occurring organisms to break down hazardous substances into less toxic or non toxic substances”.
Bioremediation is widely used to treat human sewage and has also been used to remove agricultural chemicals (pesticides and fertilizers) that leach from soil into groundwater. Certain toxic metals, such as selenium and arsenic compounds, can also be removed from water by bioremediation. Mercury is an example of a toxic metal that can be removed from an environment by bioremediation. Mercury is an active ingredient of some pesticides and is also a byproduct of certain industries, such as battery production. Mercury is usually present in very low concentrations in natural environments but it is highly toxic because it accumulates in living tissues. Several species of bacteria can carry out the biotransformation of toxic mercury into nontoxic forms. These bacteria, such as Pseudomonas aeruginosa, can convert Hg2+ to Hg, which is less toxic to humans.
Probably one of the most useful and interesting examples of the use of prokaryotes for bioremediation purposes is the cleanup of oil spills. The importance of prokaryotes to petroleum bioremediation has been demonstrated in several oil spills in recent years, such as the Exxon Valdez spill in Alaska (1989) (Figure 1), the Prestige oil spill in Spain (2002), the spill into the Mediterranean from a Lebanon power plant (2006,) and more recently, the BP oil spill in the Gulf of Mexico (2010). To clean up these spills, bioremediation is promoted by adding inorganic nutrients that help bacteria already present in the environment to grow. Hydrocarbon-degrading bacteria feed on the hydrocarbons in the oil droplet, breaking them into inorganic compounds. Some species, such as Alcanivorax borkumensis, produce surfactants that solubilize the oil, while other bacteria degrade the oil into carbon dioxide. In the case of oil spills in the ocean, ongoing, natural bioremediation tends to occur, inasmuch as there are oil-consuming bacteria in the ocean prior to the spill. Under ideal conditions, it has been reported that up to 80 percent of the nonvolatile components in oil can be degraded within 1 year of the spill. Researchers have genetically engineered other bacteria to consume petroleum products; indeed, the first patent application for a bioremediation application in the U.S. was for a genetically modified oil-eating bacterium.

There are a number of cost/efficiency advantages to bioremediation, which can be employed in areas that are inaccessible without excavation. For example, hydrocarbon spills (specifically, oil spills) or certain chlorinated solvents may contaminate groundwater, which can be easier to treat using bioremediation than more conventional approaches. This is typically much less expensive than excavation followed by disposal elsewhere, incineration, or other off-site treatment strategies. It also reduces or eliminates the need for “pump and treat”, a practice common at sites where hydrocarbons have contaminated clean groundwater. Using prokaryotes for bioremediation of hydrocarbons also has the advantage of breaking down contaminants at the molecular level, as opposed to simply chemically dispersing the contaminant.
Attribution
“Bioremediation” is licensed under CC BY 4.0. “Prokaryotic Diversity” by OpenStax is licensed under CC BY 4.0. Modified from originals by Matthew R. Fisher.
Case Study: The Love Canal Disaster
One of the most famous and important examples of groundwater pollution in the U.S. is the Love Canal tragedy in Niagara Falls, New York. It is important because the pollution disaster at Love Canal, along with similar pollution calamities at that time (Times Beach, Missouri and Valley of Drums, Kentucky), helped to create Superfund, a federal program instituted in 1980 and designed to identify and clean up the worst of the hazardous chemical waste sites in the U.S.

Love Canal is a neighborhood in Niagara Falls named after a large ditch (approximately 15 m wide, 3–12 m deep, and 1600 m long) that was dug in the 1890s for hydroelectric power. The ditch was abandoned before it actually generated any power and went mostly unused for decades, except for swimming by local residents. In the 1920s Niagara Falls began dumping urban waste into Love Canal, and in the 1940s the U.S. Army dumped waste from World War II there, including waste from the frantic effort to build a nuclear bomb. Hooker Chemical purchased the land in 1942 and lined it with clay. Then, the company put into Love Canal an estimated 21,000 tons of hazardous chemical waste, including the carcinogens benzene, dioxin, and PCBs in large metal barrels and covered them with more clay. In 1953, Hooker sold the land to the Niagara Falls school board for $1, and included a clause in the sales contract that both described the land use (filled with chemical waste) and absolved them from any future damage claims from the buried waste. The school board promptly built a public school on the site and sold the surrounding land for a housing project that built 200 or so homes along the canal banks and another 1,000 in the neighborhood (Figure 1). During construction, the canal’s clay cap and walls were breached, damaging some of the metal barrels.
Eventually, the chemical waste seeped into people’s basements, and the metal barrels worked their way to the surface. Trees and gardens began to die; bicycle tires and the rubber soles of children’s shoes disintegrated in noxious puddles. From the 1950s to the late 1970s, residents repeatedly complained of strange odors and substances that surfaced in their yards. City officials investigated the area, but did not act to solve the problem. Local residents allegedly experienced major health problems including high rates of miscarriages, birth defects, and chromosome damage, but studies by the New York State Health Department disputed that. Finally, in 1978 President Carter declared a state of emergency at Love Canal, making it the first human-caused environmental problem to be designated that way. The Love Canal incident became a symbol of improperly stored chemical waste. Clean up of Love Canal, which was funded by Superfund and completely finished in 2004, involved removing contaminated soil, installing drainage pipes to capture contaminated groundwater for treatment, and covering it with clay and plastic. In 1995, Occidental Chemical (the modern name for Hooker Chemical) paid $102 million to Superfund for cleanup and $27 million to Federal Emergency Management Association for the relocation of more than 1,000 families. New York State paid $98 million to EPA and the US government paid $8 million for pollution by the Army. The total clean up cost was estimated to be $275 million.
The Love Canal tragedy helped to create Superfund, which has analyzed tens of thousands of hazardous waste sites in the U.S. and cleaned up hundreds of the worst ones. Nevertheless, over 1,000 major hazardous waste sites with a significant risk to human health or the environment are still in the process of being cleaned.
Attribution
Essentials of Environmental Science by Kamala Doršner is licensed under CC BY 4.0. Modified from the original by Matthew R. Fisher.
Conclusions
Environmental health is concerned with preventing disease, death and disability by reducing exposure to adverse environmental conditions and promoting behavioral change. It focuses on the direct and indirect causes of diseases and injuries, and taps resources inside and outside the health care system to help improve health outcomes. Environmental health risks can be grouped into two broad categories. Traditional hazards related to poverty and lack of development affect developing countries and poor people most. Modern hazards, caused by development that lacks environmental safeguards, such as urban (outdoor) air pollution and exposure to agro-industrial chemicals and waste, prevail in industrialized countries, where exposure to traditional hazards is low. Each year contaminated water and poor sanitation contribute to 5.4 billion cases of diarrhea worldwide and 1.6 million deaths, mostly among children under the age of five. Indoor air pollution—a much less publicized source of poor health—is responsible for more than 1.6 million deaths per year and for 2.7 percent of global burden of disease.
Emerging and reemerging diseases have been defined as infectious diseases of humans whose occurrence during the past two decades has substantially increased or threatens to increase in the near future relative to populations affected, geographic distribution, or magnitude of impacts. Antibiotic resistance is a global problem. New forms of antibiotic resistance can cross international boundaries and spread between continents. Environmental toxicology is the scientific study of the health effects associated with exposure to toxic chemicals and systems occurring in the natural, work, and living environments; the management of environmental toxins and toxicity; and the development of protections for humans, animals, and plants. Environmental contaminants are chemicals found in the environment in amounts higher than what would be there naturally. We can be exposed to these contaminants from a variety of residential, commercial, and industrial sources.
Questions for Review
- Define environmental health.
- Define the following terms: carcinogenic, mutagenic, teratogenic, endocrine disruptor.
- Describe the difference between acute and chronic effect.
- Give two examples of emerging diseases.
- Define modern hazards.
- What are the three main routes of exposure a chemical can get into our body?
- What are the two types of mercury people are usually exposed to?
Questions for Discussion
- What are the key differences between science and a less objective belief system, such as religion?
- What factors result in scientific controversies about environmental issues? Contrast these with environmental controversies that exist because of differing values and world views.
- Explain why there are no scientific “laws” to explain the structure and function of ecosystems.
- Many natural phenomena are highly variable, particularly ones that are biological or ecological. What are the implications of this variability for understanding and predicting the causes and consequences of environmental changes? How do environmental scientists cope with this challenge of a variable natural world?
Exploring Issues
- Devise an environmental question of interest to yourself. Suggest useful hypotheses to investigate, identify the null hypotheses, and outline experiments that you might conduct to provide answers to this question.
- During a research project investigating mercury, an environmental scientist performed a series of chemical analyses of fish caught in Lake Canuck. The sampling program involved seven species of fish obtained from various habitats within the lake. A total of 360 fish of various sizes and sexes were analyzed. It was discovered that 30% of the fish had residue levels greater than 0.5 ppm of mercury, the upper level of contamination recommended by Health Canada for fish eaten by humans. The scientist reported these results to a governmental regulator, who was alarmed by the high mercury residues because of Lake Canuck’s popularity as a place where people fish for food. The regulator asked the scientist to recommend whether it was safe to eat any fish from the lake or whether to avoid only certain sizes, sexes, species, or habitats. What sorts of data analyses should the scientist perform to develop useful recommendations? What other scientific and non-scientific aspects should be considered?
References Cited and Further Reading
EPA. (n.d.). Attachment 6: Useful terms and definitions for explaining risk. Accessed August 31, 2015 at http://www.epa.gov/superfund/community/pdfs/toolkit/risk_communication-attachment6.pdf. Modified from original.
OSHA. (n.d.). Understanding chemical hazards. Accessed August 25, 2015 fromhttps://www.osha.gov/dte/grant_materials/fy11/sh-22240-11/ChemicalHazards.pdf. Modified from original.
Theis, T. & Tomkin, J. (Eds.). (2015). Sustainability: A comprehensive foundation. Retrieved from http://cnx.org/contents/1741effd-9cda-4b2b-a91e-003e6f587263@43.5. Available under Creative Commons Attribution 4.0 International License. (CC BY 4.0). Modified from original.
University of California College Prep. (2012). AP environmental science. Retrieved from http://cnx.org/content/col10548/1.2/. Available under Creative Commons Attribution 4.0 International License. (CC BY 4.0). Modified from original.
World Bank. (2003). Environmental health. Washington, DC. World Bank. Retrieved from https://openknowledge.worldbank.org/handle/10986/9734. Available under Creative Commons Attribution License 3.0 (CC BY 3.0). Modified from Original.
World Bank. (2008). Environmental health and child survival : Epidemiology, economics, experiences. Washington, DC: World Bank. World Bank. Retrieved from https://openknowledge.worldbank.org/handle/10986/6534. Available under Creative Commons Attribution License 3.0 (CC BY 3.0). Modified from original.
World Bank. (2009). Environmental health and child survival. Retrieved from https://openknowledge.worldbank.org/handle/10986/11719. Available under Creative Commons Attribution License 3.0 (CC BY 3.0). Modified from original.

