5.3 – Physiology (Function) of the Urinary System
- Remove waste products and medicines from the body.
- Balance the body’s fluids.
- Balance a variety of electrolytes.
- Release hormones to control blood pressure.
- Release a hormone to control red blood cell production.
- Help with bone health by controlling calcium and phosphorus.
Having reviewed the anatomy of the urinary system, now is the time to focus on physiology. You will discover that different parts of the nephron utilize specific processes to produce urine: filtration, reabsorption, and secretion. You will learn how each of these processes works and where they occur along the nephron and collecting ducts. The physiologic goal is to modify the composition of the plasma and, in doing so, produce the waste product: urine.
Nephrons: The Functional Unit
Nephrons take a simple filtrate of the blood and modify it into urine. Many changes take place in the different parts of the nephron before urine is created for disposal. The term “forming urine” will be used hereafter to describe the filtrate as it is modified into true urine. The principal task of the nephron population is to balance the plasma to homeostatic set points and excrete potential toxins in the urine. They do this by accomplishing three principle functions—filtration, reabsorption, and secretion. They also have additional secondary functions that exert control in three areas: blood pressure (via the production of renin), red blood cell production (via the hormone EPO), and calcium absorption (via the conversion of calcidiol into calcitriol, the active form of vitamin D).
Loop of Henle
The descending and ascending portions of the loop of Henle (sometimes referred to as the nephron loop) are, of course, just continuations of the same tubule. They run adjacent and parallel to each other after having made a hairpin turn at the deepest point of their descent. The descending loop of Henle consists of an initial short, thick portion and long, thin portion, whereas the ascending loop consists of an initial short, thin portion followed by a long, thick portion. The descending and ascending thin portions consist of simple squamous epithelium. Different portions of the loop have different permeabilities for solutes and water.
Collecting Ducts
The collecting ducts are continuous with the nephron but are not technically part of it. In fact, each duct collects filtrate from several nephrons for final modification. Collecting ducts merge as they descend deeper in the medulla to form about 30 terminal ducts, which empty at a papilla.
Glomerular Filtration Rate (GFR)
The volume of filtrate formed by both kidneys per minute is termed the glomerular filtration rate (GFR). The heart pumps about 5 L of blood per minute under resting conditions. Approximately 20 percent or one litre enters the kidneys to be filtered. On average, this litre results in the production of about 125 mL/minute filtrate produced in men (range of 90 to 140 mL/minute) and 105 mL/minute filtrate produced in women (range of 80 to 125 mL/minute). This amount equates to a volume of about 180 L/day in men and 150 L/day in women. Ninety-nine percent of this filtrate is returned to the circulation by reabsorption so that only about 1–2 litres of urine are produced per day.
GFR is influenced by the hydrostatic pressure and colloid osmotic pressure on either side of the capillary membrane of the glomerulus. Recall that filtration occurs as pressure forces fluid and solutes through a semipermeable barrier with the solute movement constrained by particle size. Hydrostatic pressure is the pressure produced by a fluid against a surface. If you have fluid on both sides of a barrier, both fluids exert pressure in opposing directions. The net fluid movement will be in the direction of the lower pressure. Osmosis is the movement of solvent (water) across a membrane that is impermeable to a solute in the solution. This creates osmotic pressure which will exist until the solute concentration is the same on both sides of a semipermeable membrane. As long as the concentration differs, water will move. Glomerular filtration occurs when glomerular hydrostatic pressure exceeds the luminal hydrostatic pressure of Bowman’s capsule. There is also an opposing force, the osmotic pressure, which is typically higher in the glomerular capillary. To understand why this is so, look more closely at the microenvironment on either side of the filtration membrane.
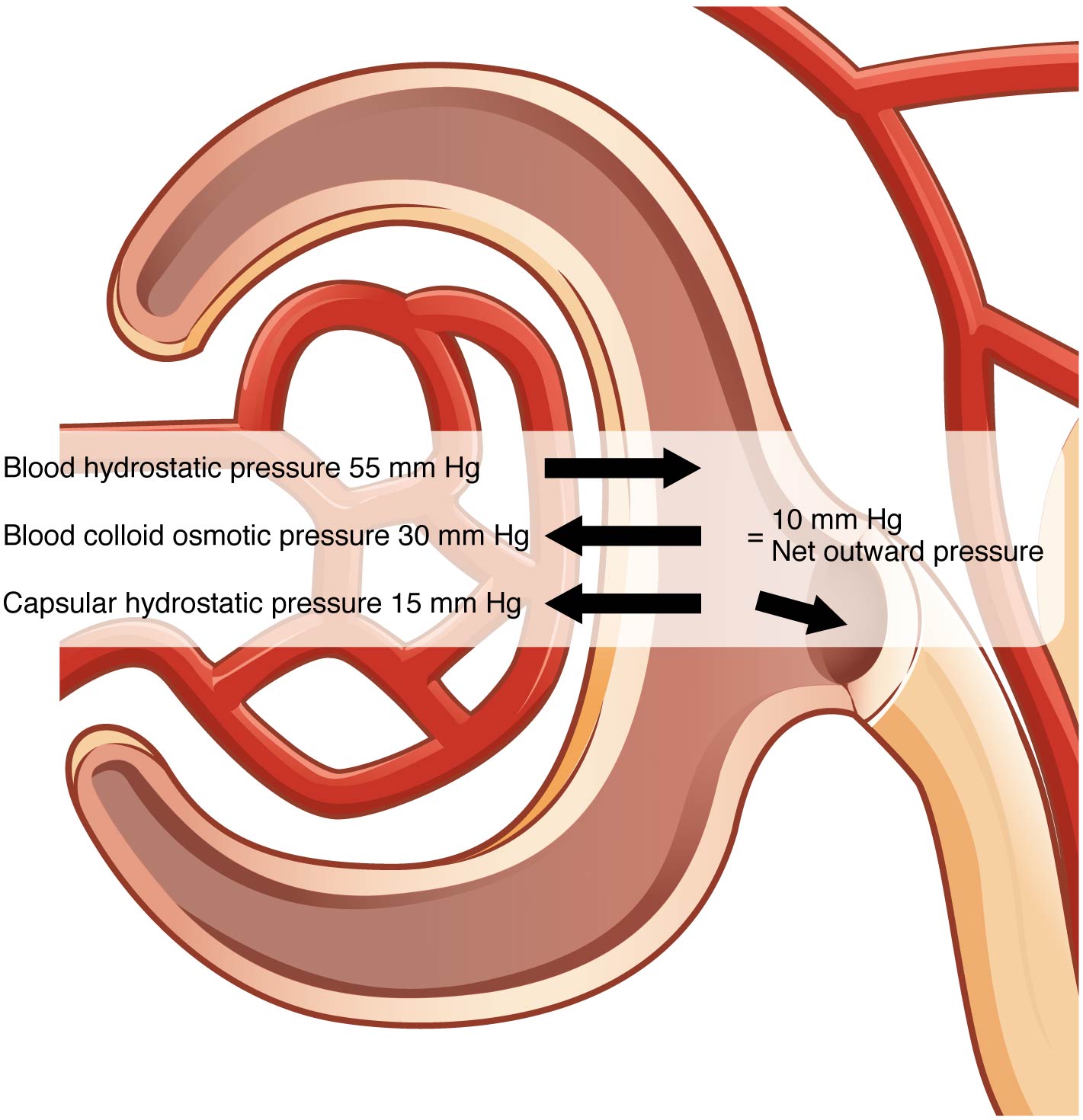
You will find osmotic pressure exerted by the solutes inside the lumen of the capillary as well as inside of Bowman’s capsule. Since the filtration membrane limits the size of particles crossing the membrane, the osmotic pressure inside the glomerular capillary is higher than the osmotic pressure in Bowman’s capsule. Recall that cells and the medium-to-large proteins cannot pass between the podocyte processes or through the fenestrations of the capillary endothelial cells. This means that red and white blood cells, platelets, albumins, and other proteins too large to pass through the filter remain in the capillary, creating an average colloid osmotic pressure of 30 mm Hg within the capillary. The absence of proteins in Bowman’s space (the lumen within Bowman’s capsule) results in an osmotic pressure near zero. Thus, the only pressure moving fluid across the capillary wall into the lumen of Bowman’s space is hydrostatic pressure. Hydrostatic (fluid) pressure is sufficient to push water through the membrane despite the osmotic pressure working against it. The sum of all of the influences, both osmotic and hydrostatic, results in a net filtration pressure (NFP) of about 10 mm Hg (see Figure 5.7).
A proper concentration of solutes in the blood is important in maintaining osmotic pressure both in the glomerulus and systemically. There are disorders in which too much protein passes through the filtration slits into the kidney filtrate. This excess protein in the filtrate leads to a deficiency of circulating plasma proteins. In turn, the presence of protein in the urine increases its osmolarity; this holds more water in the filtrate and results in an increase in urine volume. Because there is less circulating protein, principally albumin, the osmotic pressure of the blood falls. Less osmotic pressure pulling water into the capillaries tips the balance towards hydrostatic pressure, which tends to push it out of the capillaries. The net effect is that water is lost from the circulation to interstitial tissues and cells. This “plumps up” the tissues and cells, a condition termed systemic edema.
Reabsorption and Secretion
The renal corpuscle filters the blood to create a filtrate that differs from blood mainly in the absence of cells and large proteins. From this point to the ends of the collecting ducts, the filtrate or forming urine is undergoing modification through secretion and reabsorption before true urine is produced. Here, some substances are reabsorbed, whereas others are secreted. Note the use of the term “reabsorbed.” All of these substances were “absorbed” in the digestive tract—99 percent of the water and most of the solutes filtered by the nephron must be reabsorbed. Water and substances that are reabsorbed are returned to the circulation by the peritubular and vasa recta capillaries.
It is vital that the flow of blood through the kidney is at a suitable rate to allow for filtration. This rate determines how much solute is retained or discarded, how much water is retained or discarded, and ultimately, the osmolarity of blood and the blood pressure of the body.
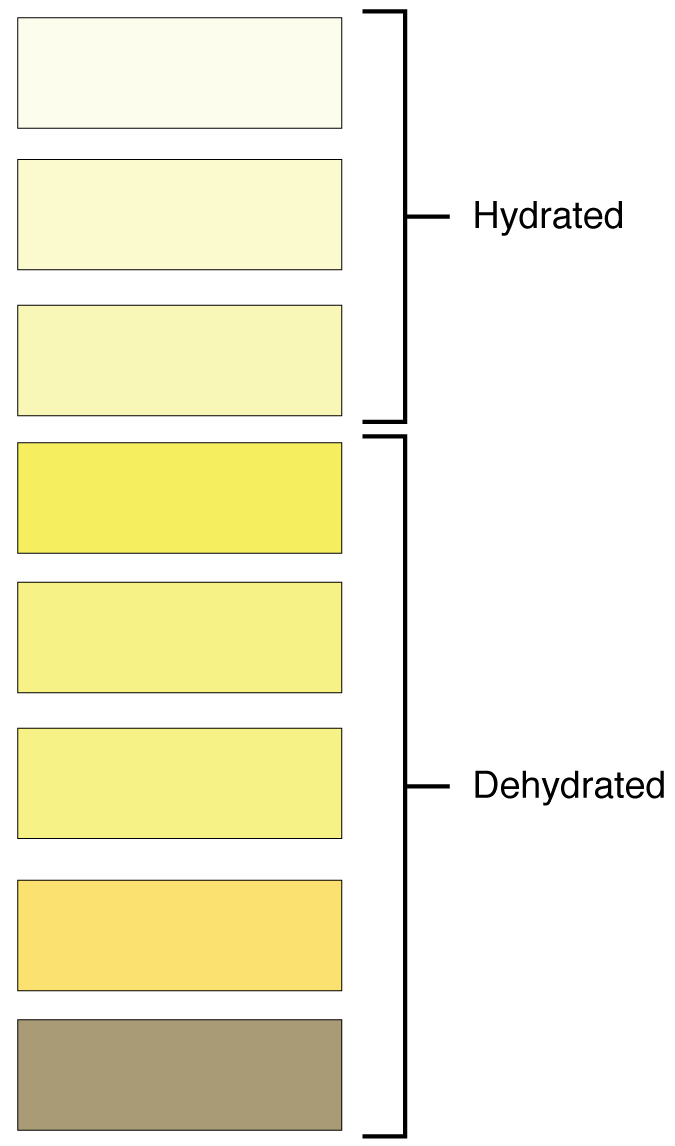
Urinalysis
Urinalysis (urine analysis) often provides clues to renal disease. Normally, only traces of protein are found in urine, and when higher amounts are found, damage to the glomeruli is the likely basis. Unusually large quantities of urine may point to diseases like diabetes mellitus or hypothalamic tumors that cause diabetes insipidus. The color of urine is determined mostly by the breakdown products of red blood cell destruction (see Figure 5.8). The “heme” of hemoglobin is converted by the liver into water-soluble forms that can be excreted into the bile and indirectly into the urine. This yellow pigment is urochrome. Urine color may also be affected by certain foods like beets, berries, and fava beans. A kidney stone or a cancer of the urinary system may produce sufficient bleeding to manifest as pink or even bright red urine. Diseases of the liver or obstructions of bile drainage from the liver impart a dark “tea” or “cola” hue to the urine. Dehydration produces darker, concentrated urine that may also possess the slight odour of ammonia. Most of the ammonia produced from protein breakdown is converted into urea by the liver, so ammonia is rarely detected in fresh urine. The strong ammonia odour you may detect in bathrooms or alleys is due to the breakdown of urea into ammonia by bacteria in the environment. About one in five people detect a distinctive odour in their urine after consuming asparagus; other foods such as onions, garlic, and fish can impart their own aromas. These food-caused odours are harmless.
The kidneys must produce a minimum urine volume of about 500 mL/day to rid the body of wastes. Output below this level may be caused by severe dehydration or renal disease and is termed oliguria. The virtual absence of urine production is termed anuria. Excessive urine production is polyuria, which may be due to diabetes mellitus or diabetes insipidus. In diabetes mellitus, blood glucose levels exceed the number of available sodium-glucose transporters in the kidney, and glucose appears in the urine. The osmotic nature of glucose attracts water, leading to its loss in the urine. In the case of diabetes insipidus, insufficient pituitary antidiuretic hormone (ADH) release or insufficient numbers of ADH receptors in the collecting ducts means that too few water channels are inserted into the cell membranes that line the collecting ducts of the kidney. Insufficient numbers of water channels (aquaporins) reduce water absorption, resulting in high volumes of very dilute urine.
Concept Check
- Contrast the following terms: oliguria, anuria and polyuria. What are the differences between these terms as they describe urinary output?
- Explain how urine colour varies based on food consumed and/or hydration levels.
Endocrine Urinary Function
Several hormones have specific, important roles in regulating kidney function. They act to stimulate or inhibit blood flow. Some of these are endocrine, acting from a distance, whereas others are paracrine, acting locally.
Renin–Angiotensin–Aldosterone
Renin is an enzyme that is produced by the granular cells of the afferent arteriole. It enzymatically converts angiotensinogen (made by the liver, freely circulating) into angiotensin I. Its release is stimulated by prostaglandins to decreased extracellular fluid volume.
Angiotensin II is a potent vasoconstrictor that plays an immediate role in the regulation of blood pressure. It acts systemically to cause vasoconstriction as well as constriction of both the afferent and efferent arterioles of the glomerulus. In instances of blood loss or dehydration, it reduces both GFR and renal blood flow, thereby limiting fluid loss and preserving blood volume. Its release is usually stimulated by decreases in blood pressure, and so the preservation of adequate blood pressure is its primary role.
Aldosterone, often called the “salt-retaining hormone,” is released from the adrenal cortex in response to angiotensin II or directly in response to increased plasma potassium. It promotes sodium reabsorption by the nephron, promoting the retention of water.
Antidiuretic Hormone (ADH)
Diuretics are drugs that can increase water loss by interfering with the recapture of solutes and water from the forming urine. They are often prescribed to lower blood pressure. ADH, released by the posterior pituitary, works to do the exact opposite. It promotes the recovery of water, decreases urine volume, and maintains plasma osmolarity and blood pressure. It does so by stimulating the movement of aquaporin proteins into the apical cell membrane of principal cells of the collecting ducts to form water channels, allowing the transcellular movement of water from the lumen of the collecting duct into the interstitial space in the medulla of the kidney by osmosis. From there, it enters the vasa recta capillaries to return to the circulation. Water is attracted by the high osmotic environment of the deep kidney medulla.
Parathyroid Hormone
Parathyroid hormone (PTH) is produced by the parathyroid glands in response to decreased circulating calcium levels.
Maintaining Homeostasis
Homeostasis requires that volume and osmolarity be preserved. Blood volume is important in maintaining sufficient blood pressure, and there are nonrenal mechanisms involved in its preservation, including vasoconstriction, which can act within seconds of a drop in pressure. Thirst mechanisms are also activated to promote the consumption of water lost through respiration, evaporation, or urination. Hormonal mechanisms are activated to recover volume while maintaining a normal osmotic environment. These mechanisms act principally on the kidney.
Diuretics and Fluid Volume
A diuretic is a compound that increases urine volume. Three familiar drinks contain diuretic compounds: coffee, tea, and alcohol. The caffeine in coffee and tea works by promoting vasodilation in the nephron, which increases GFR. Alcohol increases GFR by inhibiting ADH release from the posterior pituitary, resulting in less water recovery by the collecting duct. In cases of high blood pressure, diuretics may be prescribed to reduce blood volume and, thereby, reduce blood pressure. The most frequently prescribed anti-hypertensive diuretic is hydrochlorothiazide.
Regulation of Nitrogen Wastes
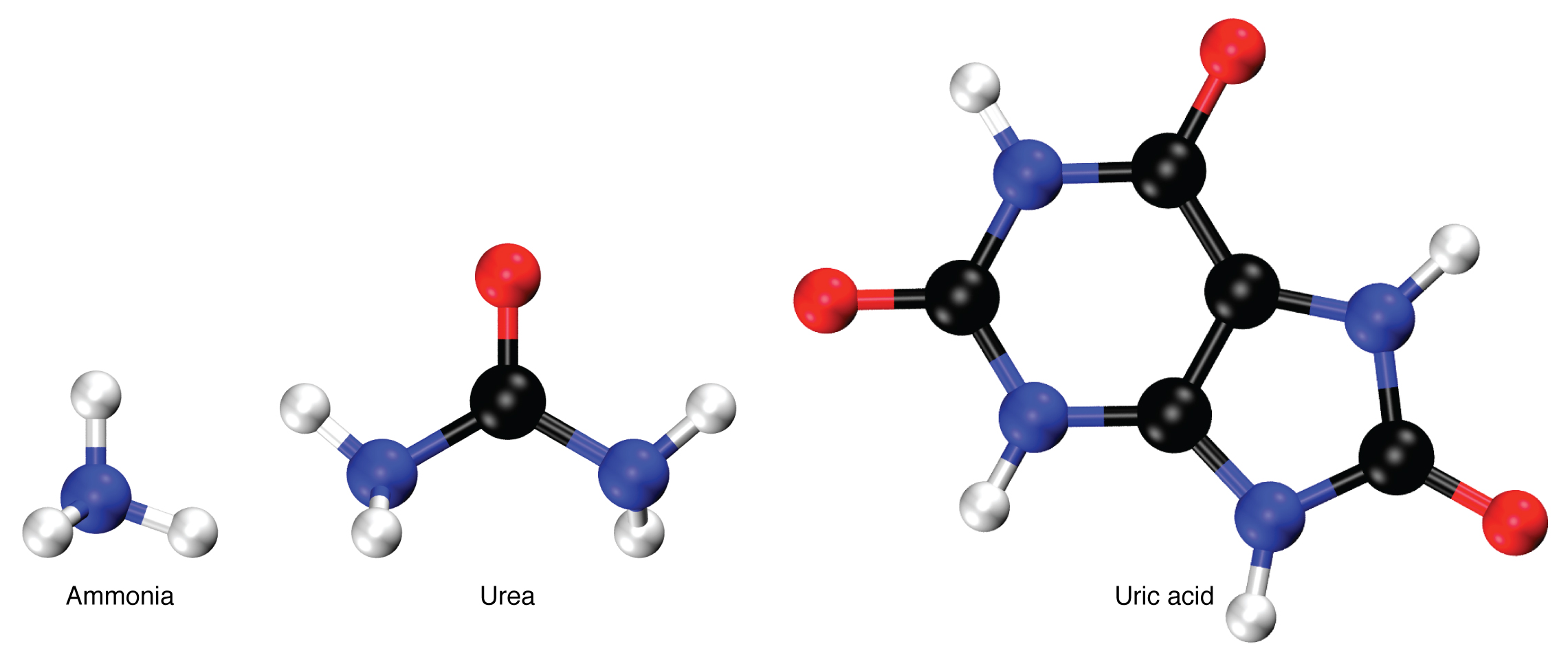
Nitrogen wastes are produced by the breakdown of proteins during normal metabolism. Proteins are broken down into amino acids, which in turn are deaminated by having their nitrogen groups removed. Deamination converts the amino (NH2) groups into ammonia (NH3), ammonium ion (NH4+), urea, or uric acid (Figure 5.9). Ammonia is extremely toxic, so most of it is very rapidly converted into urea in the liver. Human urinary wastes typically contain primarily urea with small amounts of ammonium and very little uric acid.
Elimination of Drugs and Hormones
Water-soluble drugs may be excreted in the urine and are influenced by one or all of the following processes: glomerular filtration, tubular secretion, or tubular reabsorption. Drugs that are structurally small can be filtered by the glomerulus with the filtrate. Large drug molecules such as heparin or those that are bound to plasma proteins cannot be filtered and are not readily eliminated. Some drugs can be eliminated by carrier proteins that enable secretion of the drug into the tubule lumen. There are specific carriers that eliminate basic (such as dopamine or histamine) or acidic drugs (such as penicillin or indomethacin). As is the case with other substances, drugs may be both filtered and reabsorbed passively along a concentration gradient.
Watch Urinary System, Part 2: Crash Course Anatomy & Physiology #39 (10 min) on YouTube
Media 5.3: CrashCourse. (2015, October 19). Urinary system, part 2: Crash Course anatomy & physiology #39 [Video]. YouTube. https://youtu.be/DlqyyyvTI3k
Urinary System Medical Terms and Abbreviations
Urinary System Medical Terms Not Easily Broken into Word Parts
Urinary System Medical Terms Not Easily Broken into Word Parts (Text version)
- deamination
- dē-am-ĭ-NĀ-shŏn
- The removal of an amino group from a molecule.
- distended
- dis-TEN-ded (Original Term)
- stretch out
- enuresis
- en-ū-RĒ-sĭs (Original Term)
- involuntary urination
- hemodialysis (HD)
- hē-mō-dī-ĂL-ĭ-sĭs
- procedure for removing impurities from the blood due to an inability of the kidney to function
- hydrostatic
- hī-drō-STAT-ik
- Relating to the equilibrium of liquids and the pressure exerted by liquid at rest
- incontinence
- in-KONT-ĭn-ĕns (Original Term)
- inability to control the bladder and/or bowels
- micturate
- MĬK-tū-rāt (Original Term)
- to pass urine
- sphincter
- SFĬNK-tĕr
- A circular muscle constricting an orifice
- stricture
- STRIK-chŭr (Original Term)
- abnormal narrowing
- urinal
- Ū-rĭn-ăl (Original Term)
- receptacle for urine
- void
- VOYD (Original Term)
- empty or evacuate waste material, urinate
Activity Source: Urinary System Medical Terms not easily broken into word parts from Medical Terminology. by Grimm et al., licensed under CC BY 4.0. / Some H5P audio re-recorded by David McCuaig and text version added.
Urinary System Abbreviations
Learn these common abbreviations by expanding the list below.
Urinary System Abbreviations
- ARF (acute renal failure)
- BUN (blood urea nitrogen)
- cath (catheter, catheterization)
- CKD (chronic kidney disease)
- ESRD (end-stage renal disease)
- ESWL (extracorporeal shock wave lithotripsy)
- HD (hemodialysis)
- OAB (overactive bladder)
- SG (specific gravity)
- UA (urinalysis)
- UTI (urinary tract infection)
- VCUG (voiding cystourethrogram or void cystourethrogram)
Activity source: Urinary System Abbreviations by Kimberlee Carter from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0.
Image Descriptions
Figure 5.7 image description: This figure shows the different pressures acting across the glomerulus including blood hydrostatic pressure, blood colloid osmotic pressure, capsular hydrostatic pressure. [Return to Figure 5.7].
Figure 5.8 image description: This color chart shows 8 different shades of yellow and associates each shade with stages of hydration (lightest 3 shades) or dehydration (remaining 5 darker shades). [Return to Figure 5.8].
Attribution
Except where otherwise noted, this chapter is adapted from “Urinary System” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Urinary System chapter content into sub-chapters.
Relating to the equilibrium of liquids and the pressure exerted by liquid at rest.
A process by which molecules of a solvent tend to pass through a membrane from a less concentrated solution into a more concentrated one.
a region of the forebrain below the thalamus
Any of a group of compounds with varying hormone-like effects.
Relating to or denoting an apex.
biological process that results in stable equilibrium
The removal of an amino group from a molecule.

