4.3 – Physiology (Function) of the Respiratory System
Blood Supply
The major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation.
- This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes pick up oxygen to be transported to tissues throughout the body.
- The pulmonary artery carries deoxygenated, arterial blood to the alveoli.
- The pulmonary artery branches multiple times as it follows the bronchi and each branch becomes progressively smaller in diameter.
- One arteriole and an accompanying venule supply and drain one pulmonary lobule. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network.
- The pulmonary capillary network consists of tiny vessels with very thin walls that lack smooth muscle fibres.
- The capillaries branch and follow the bronchioles and structure of the alveoli. It is at this point that the capillary wall meets the alveolar wall, creating the respiratory membrane.
- Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.
Nervous Innervation
The blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. Innervation by both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway.
- The parasympathetic system causes bronchoconstriction.
- The sympathetic nervous system stimulates bronchodilation.
Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from autonomic nervous system control. Sensory nerve fibres arise from the vagus nerve, and from the second to fifth thoracic ganglia. The pulmonary plexus is a region on the lung root formed by the entrance of the nerves at the hilum. The nerves then follow the bronchi in the lungs and branch to innervate muscle fibres, glands, and blood vessels.
Pleura of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum.
The pleurae consist of two layers:
- The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures (see Figure 4.11).
- The parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm.
The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.
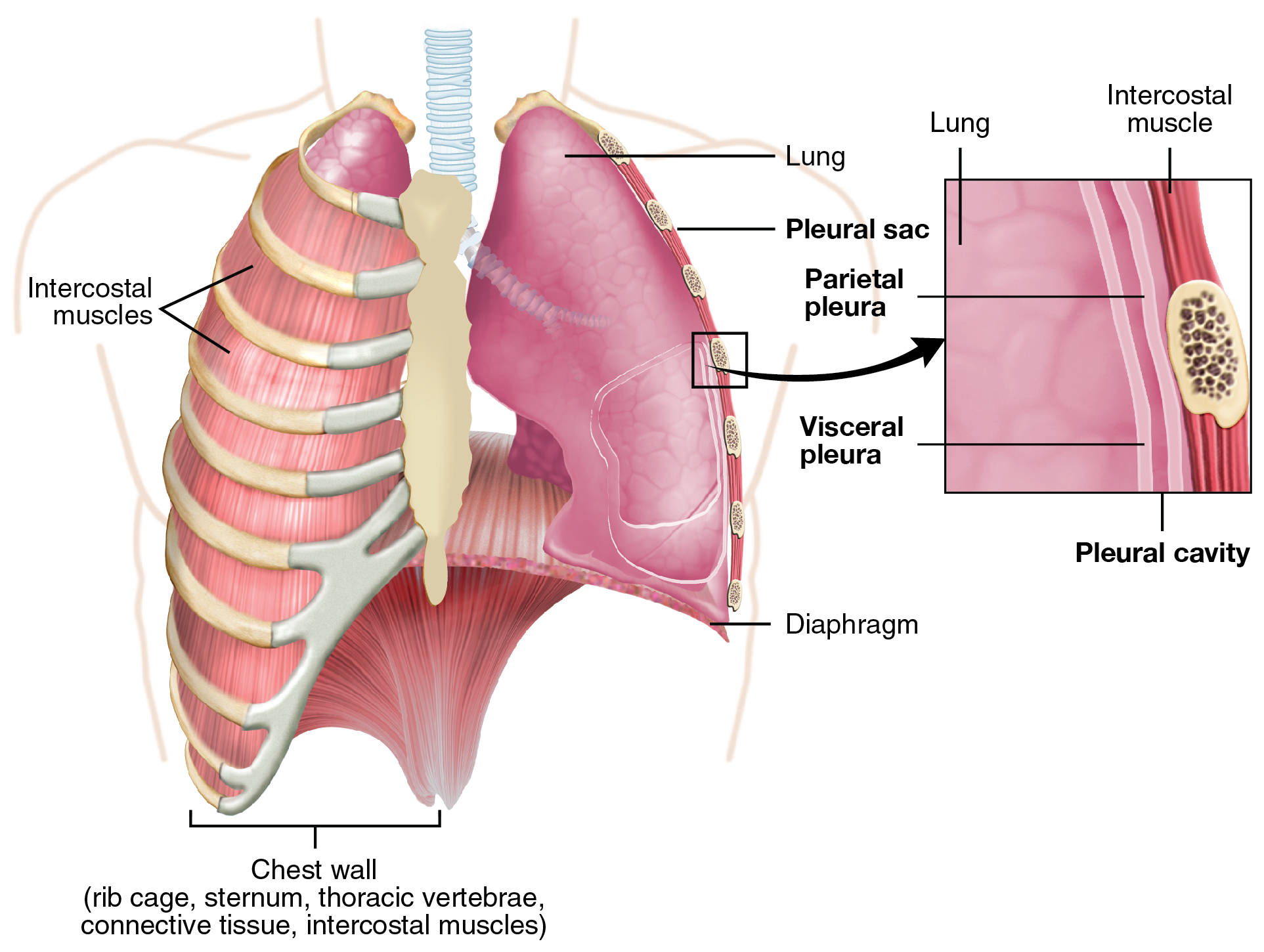
The pleurae perform two major functions:
- Produce pleural fluid that lubricates surfaces, reduces friction to prevent trauma during breathing, and creates surface tension that helps maintain the position of the lungs against the thoracic wall. This adhesive characteristic of the pleural fluid causes the lungs to enlarge when the thoracic wall expands during ventilation, allowing the lungs to fill with air.
- The pleurae also create a division between major organs that prevents interference due to the movement of the organs, while preventing the spread of infection.
Pulmonary Ventilation
The difference in pressures drives pulmonary ventilation because air flows down a pressure gradient, that is, air flows from an area of higher pressure to an area of lower pressure.
- Air flows into the lungs largely due to a difference in pressure; atmospheric pressure is greater than intra-alveolar pressure, and intra-alveolar pressure is greater than intrapleural pressure.
- Air flows out of the lungs during expiration based on the same principle; pressure within the lungs becomes greater than the atmospheric pressure.
Pulmonary ventilation comprises two major steps: inspiration and expiration (Figure 4.12). A respiratory cycle is one sequence of inspiration and expiration.
Two muscle groups are used during normal inspiration, the diaphragm and the external intercostal muscles. Additional muscles can be used if a bigger breath is required.
- The diaphragm contracts, it moves inferiorly toward the abdominal cavity, creating a larger thoracic cavity and more space for the lungs.
- The external intercostal muscles contract and moves the ribs upward and outward, causing the rib cage to expand, which increases the volume of the thoracic cavity.
Due to the adhesive force of the pleural fluid, the expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in intra-alveolar pressure, creating a pressure lower than atmospheric pressure. As a result, a pressure gradient is created that drives air into the lungs.
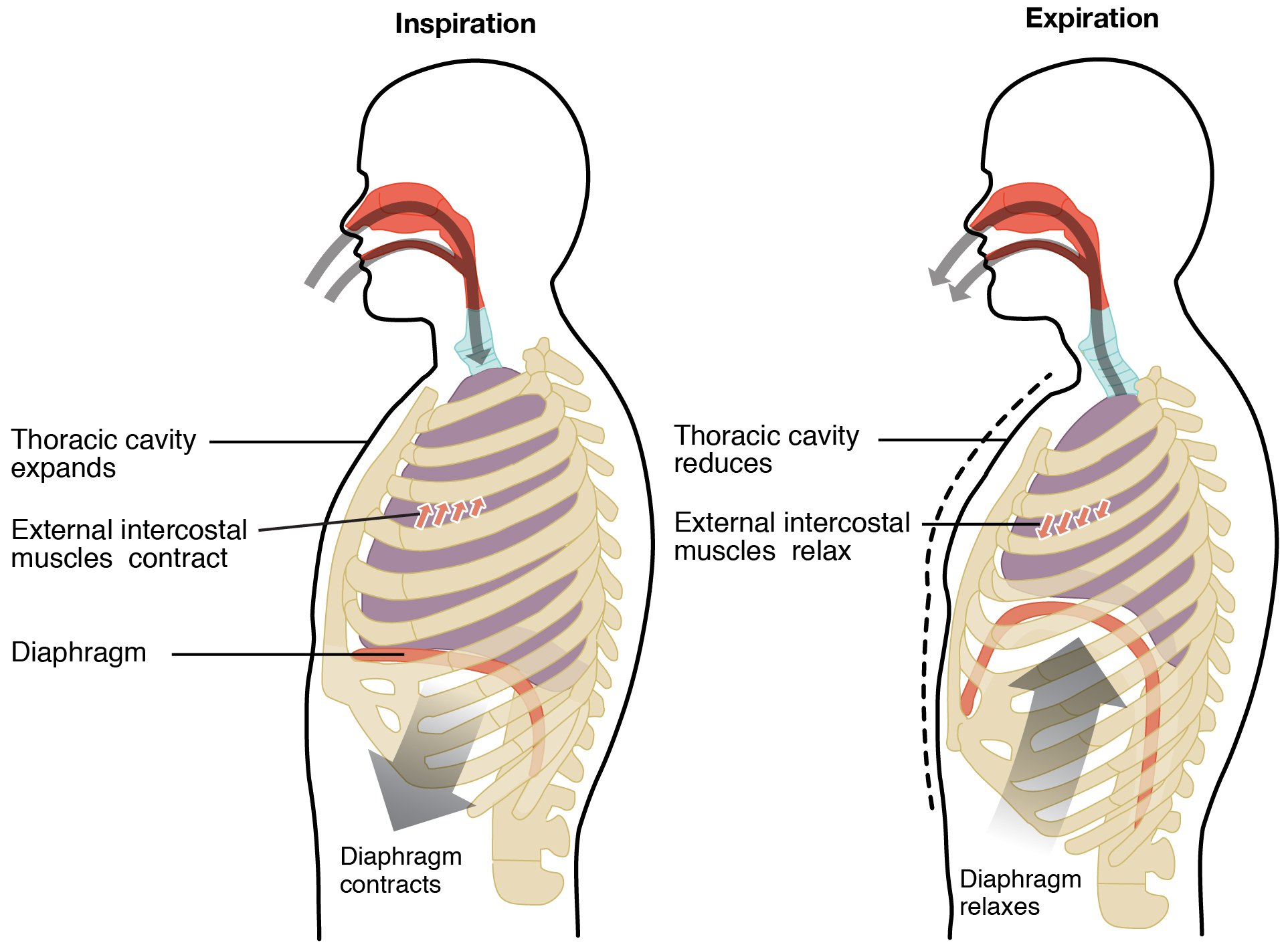
The process of normal expiration is passive, meaning that energy is not required to push air out of the lungs.
- The elasticity of the lung tissue causes the lung to recoil, as the diaphragm and intercostal muscles relax following inspiration.
- The thoracic cavity and lungs decrease in volume, causing an increase in interpulmonary pressure. The interpulmonary pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
There are different types, or modes, of breathing that require a slightly different process to allow inspiration and expiration:
- Quiet breathing, also known as eupnea, is a mode of breathing that occurs at rest and does not require the cognitive thought of the individual. During quiet breathing, the diaphragm and external intercostals must contract.
- Diaphragmatic breathing, also known as deep breathing, requires the diaphragm to contract. As the diaphragm relaxes, air passively leaves the lungs.
- Costal breathing, also known as a shallow breath, requires contraction of the intercostal muscles. As the intercostal muscles relax, air passively leaves the lungs.
- Forced breathing, also known as hyperpnea, is a mode of breathing that can occur during exercise or actions that require the active manipulation of breathing, such as singing.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
- During forced inspiration, muscles of the neck contract and lift the thoracic wall, increasing lung volume.
- During forced expiration, accessory muscles of the abdomen contract, forcing abdominal organs upward against the diaphragm. This helps to push the diaphragm further into the thorax, pushing more air out. In addition, accessory muscles help to compress the rib cage, which also reduces the volume of the thoracic cavity.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
Concept Check
- Breathing normally, place your hand on your stomach take in one full respiratory cycle.
- What type of breathing are you doing?
- Keeping your hand on your stomach, take in one large breath and exhale.
- What type of breathing are you doing?
- Complete 10 jumping jacks, once completed, place your hand on your stomach and take in one full respiratory cycle.
- What type of breathing are you doing?
Respiratory Rate and Control of Ventilation
Breathing usually occurs without thought, although at times you can consciously control it, such as when you swim under water, sing a song, or blow bubbles. The respiratory rate is the total number of breaths that occur each minute. Respiratory rate can be an important indicator of disease, as the rate may increase or decrease during an illness or in a disease condition. The respiratory rate is controlled by the respiratory center located within the medulla oblongata in the brain, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood.
The normal respiratory rate of a child decreases from birth to adolescence:
- A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute.
- By the time a child is about 10 years old, the normal rate is closer to 18 to 30.
- By adolescence, the normal respiratory rate is similar to that of adults, 12 to 18 breaths per minute.
Did You Know?
Respiratory rate is the total number of breaths that occur each minute.
Watch Respiratory System, Part 2: Crash Course Anatomy & Physiology #32 (10:30 min) on YouTube
Media 4.3: CrashCourse. (2015, August 31). Respiratory System, Part 2: Crash Course Anatomy & Physiology #32. [Video]. YouTube. https://youtu.be/Cqt4LjHnMEA
Respiratory System Words Not Easily Broken Down
Respiratory System Word Not Easily Broken Down (Text version)
- Epistaxis
- nosebleed (rhinorrhagia)
- influenza (flu)
- highly contagious viral infection effecting the respiratory tract
- pleural effusion
- fluid in the pleural space
(caused by disease or trauma)
- fluid in the pleural space
- pulmonary edema
- fluid accumulation in alveoli and bronchioles
(related to heart failure)
- fluid accumulation in alveoli and bronchioles
- pulmonary embolism (PE)
- blockage of pulmonary circulation to the lungs
- upper respiratory infection
- infection of the nasal cavity, sinuses, pharynx and larynx
- stethoscope
- instrument used to hear internal body sounds
- asphyxia
- deprivation of oxygen to tissues, suffocation
- aspirate
- suction of fluid, inhalation of fluid
- mucus
- slimy liquid secreted by mucous membranes
- nebulizer
- device that creates a mist for giving respiratory treatment or medication
- nosocomial infection
- infection acquired in hospital
- sputum
- mucous secretion from lungs, bronchi, and trachea that is expelled through the mouth
- ventilator
- mechanical device that assist with breathing
Activity Source: Respiratory System Word Not Easily Broken Down by Kimberlee Carter, licensed under CC BY 4.0./ Text version added.
Common Respiratory Abbreviations
Learn more about common respiratory abbreviations below.
Common Respiratory Abbreviations
- ABGs (arterial blood gases)
- AFB (acid-fast bacilli)
- ARDS (acute respiratory distress syndrome)
- C&S (culture and sensitivity)
- CAP (community-acquired pneumonia)
- CF (cystic fibrosis)
- CO2 (carbon dioxide)
- COPD (chronic obstructive pulmonary disease)
- CPAP (continuous positive airway pressure)
- CT (computed tomography, computerized tomography)
- CXR (chest x-ray)
- flu (influenza)
- IPF (idiopathic pulmonary fibrosis)
- LLL (left lower lobe)
- LTB (laryngotracheobronchitis)
- LUL (left upper lobe)
- O2 (oxygen)
- OSA (obstructive sleep apnea)
- PE (pulmonary embolism)
- PFM (peak flow meter)
- PFTs (pulmonary function tests)
- RLL (right lower lobe)
- RML (right middle lobe)
- RUL (right upper lobe)
- SOB (shortness of breath)
- TB (tuberculosis)
- URI (upper respiratory infection)
- BiPAP (bilevel positive airway pressure)
- CPT (chest physiotherapy)
- DPI (dry powder inhaler)
- IPPB (intermittent positive-pressure breathing)
- MDI (metered-dose inhaler)
- NIPPV (non-invasive positive-pressure ventilator)
- PEP (positive expiratory pressure)
- SVN (small-volume nebulizer)
- VAP (ventilator-associated pneumonia)
Activity source: Respiratory System Abbreviations by Kimberlee Carter, licensed under CC BY 4.0./ Converted to text.
Image Descriptions
Figure 4.11 image description: This figure shows the lungs and the chest wall, which protects the lungs, in the left panel. In the right panel, a magnified image shows the pleural cavity and a pleural sac. [Return to Figure 4.11].
Figure 4.12 image description: The left panel of this image shows a person inhaling air and the location of the thoracic muscles. The right panel shows the person exhaling air and the contraction of the thoracic cavity. [Return to Figure 4.12].
Attribution
Except where otherwise noted, this chapter is adapted from “Respiratory System” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Respiratory System chapter content into sub-chapters.
red blood cells
artery that arises from the pulmonary trunk
A concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs
rest and relaxation phase
flight or fight response
unconsciously regulates
inhalation or process of breathing air into the lungs
exhalation or the process of causing air to leave the lungs
normal breathing
forced breathing or breathing that is excessive

