10.3 – Physiology of the Blood & Blood Vessels
Physiology of the Blood Vessels
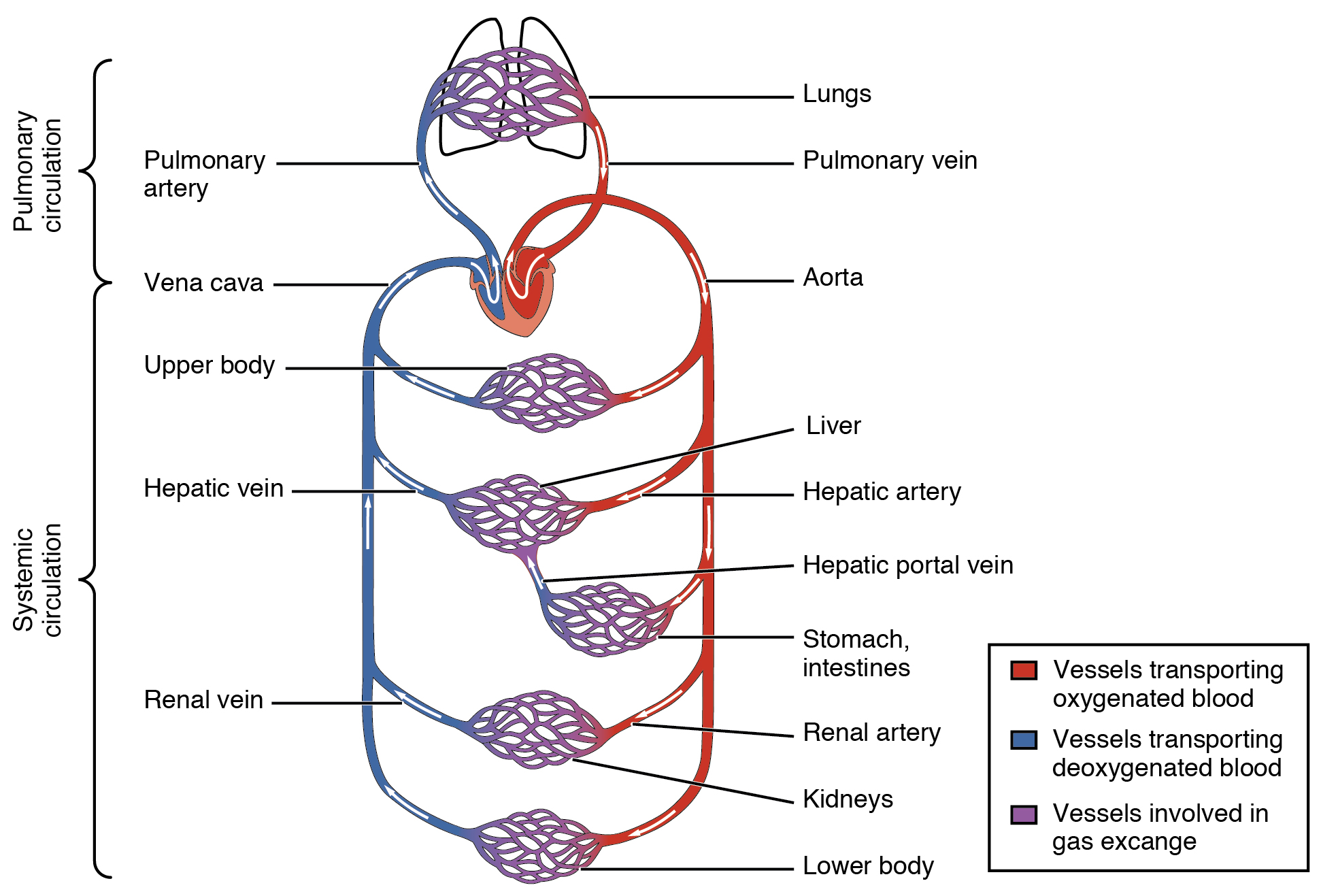
Arteries and veins transport blood in two distinct circuits: the systemic circuit and the pulmonary circuit. Systemic arteries provide blood rich in oxygen to the body’s tissues. The blood returned to the heart through systemic veins has less oxygen, since much of the oxygen carried by the arteries has been delivered to the cells. In contrast, in the pulmonary circuit, arteries carry blood low in oxygen exclusively to the lungs for gas exchange. Pulmonary veins then return freshly oxygenated blood from the lungs to the heart to be pumped back out into systemic circulation.
Blood Pressure
Blood pressure is the force exerted by blood upon the walls of the blood vessels or the chambers of the heart. Blood pressure may be measured in capillaries and veins, as well as the vessels of the pulmonary circulation; however, the general term ‘blood pressure’ refers to the pressure of blood flowing in the arteries of the systemic circulation. Blood pressure is one of the critical parameters measured on virtually every patient in every healthcare setting. The technique used today was developed more than 100 years ago by a pioneering Russian physician, Dr. Nikolai Korotkoff. Turbulent blood flow through the vessels can be heard as a soft ticking while measuring blood pressure; these sounds are known as Korotkoff sounds. Blood pressure is measured in mm Hg and is usually obtained from the brachial artery using a sphygmomanometer and a stethoscope. Blood pressure is recorded as systolic pressure over diastolic pressure.
Did You Know 1?
120/80 mm Hg is a normal, healthy blood pressure. 60-100 beats per minute is a normal, resting, adult pulse.
Five variables influence blood flow and blood pressure:
-
- Cardiac output
- Vessel Compliance
- Volume of the blood
- Viscosity of the blood
- Blood vessel length and diameter
Pulse
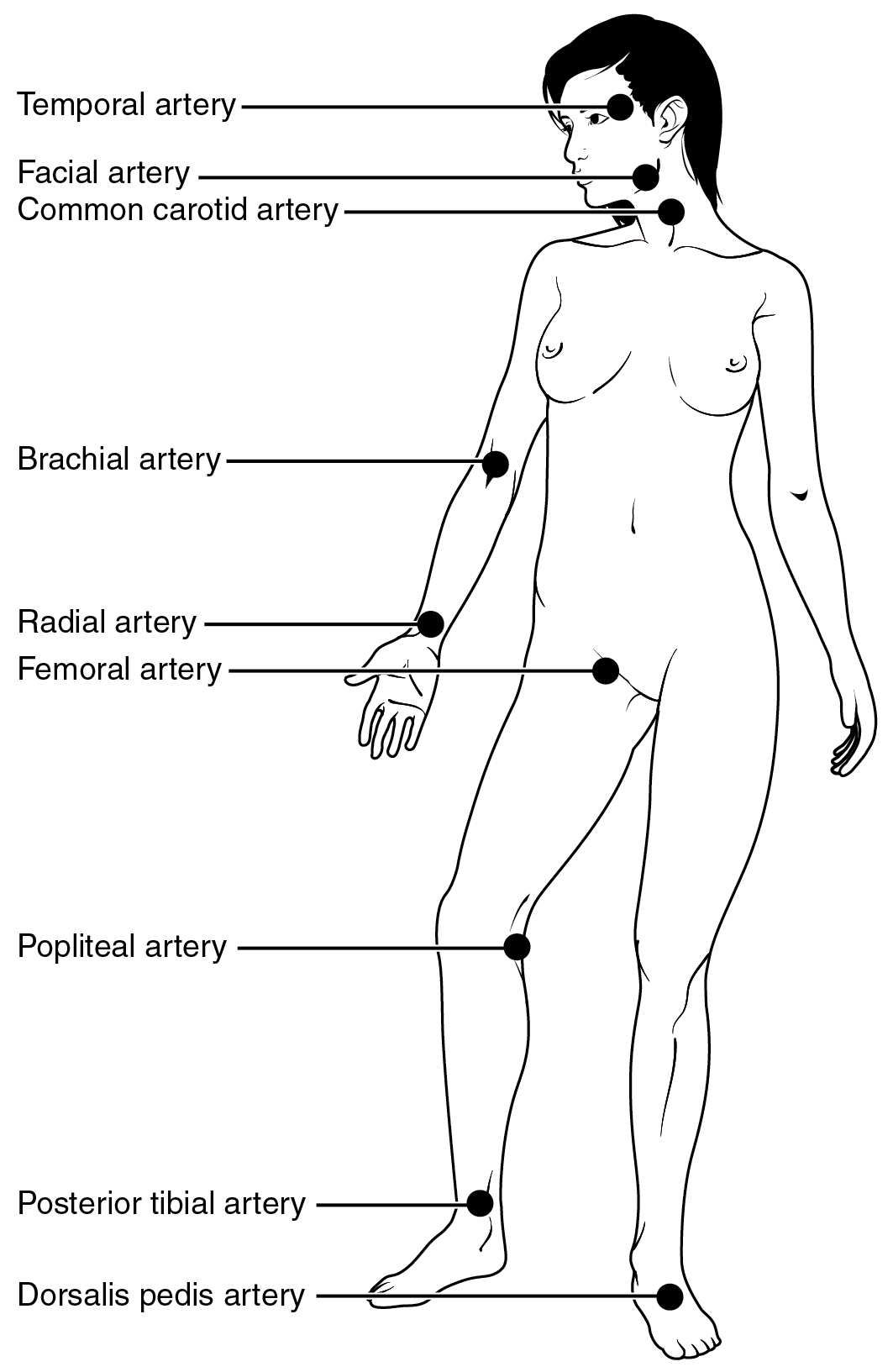
Each time the heart ejects blood forcefully into the circulation, the arteries must expand and then recoil to accommodate the surge of blood moving through them. This expansion and recoiling of the arterial wall is called the pulse and allows us to measure heart rate. Pulse can be palpated manually by placing the tips of the fingers across an artery that runs close to the body surface, such as the radial artery or the common carotid artery. These sites and other pulse sites are shown in the figure below.
Both the rate and the strength of the pulse are important clinically. A high or irregular pulse rate can be caused by physical activity or other temporary factors, but it may also indicate a heart condition. The pulse strength indicates the strength of ventricular contraction and cardiac output. If the pulse is strong, then systolic pressure is high. If it is weak, systolic pressure has fallen, and medical intervention may be warranted.
The Composition (Anatomy) of Blood and the Functions of the Components
Blood is a connective tissue made up of cellular elements and an extracellular matrix. The cellular elements are referred to as the formed elements and include red blood cells (RBCs), white blood cells (WBCs), and platelets. The extracellular matrix, called plasma, makes blood unique among connective tissues because it is fluid. This fluid, which is mostly water, perpetually suspends the formed elements and enables them to circulate throughout the body within the cardiovascular system.
Did You Know 2?
Blood constitutes approximately 8% of adult body weight.
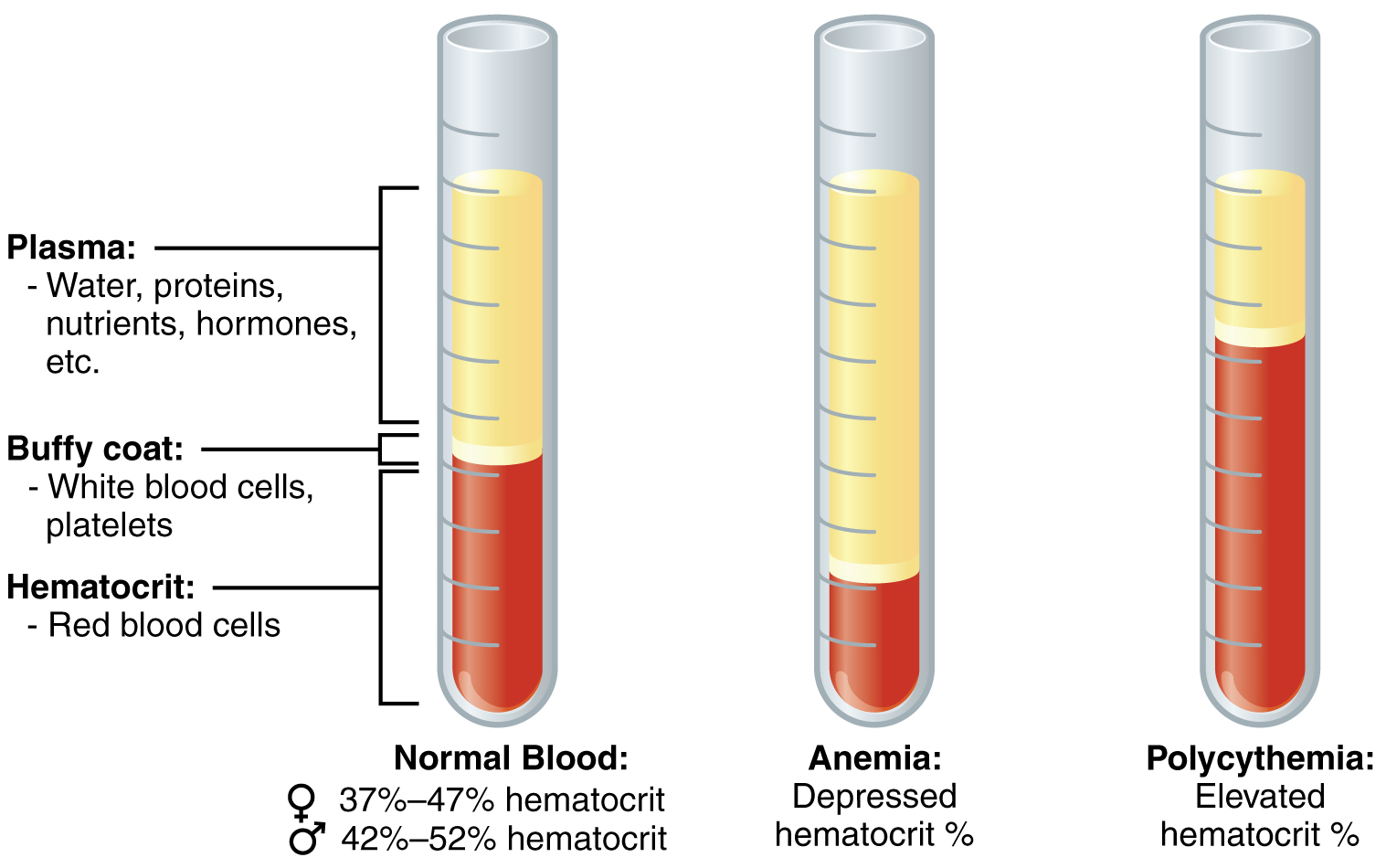
In the laboratory, blood samples are often centrifuged in order to separate the components of blood from one another (see the figure below). Erythrocytes are the heaviest elements in blood and settle at the very bottom of the tube. Above the erythrocyte layer we see the buffy coat, a pale, thin layer of leukocytes and thrombocytes, which together make up less than 1% of the sample of whole blood. Above the buffy coat is the blood plasma, normally a pale, straw-colored fluid, which constitutes the remainder of the sample.
In normal blood, about 45 percent of a sample is erythrocytes, which is referred to as the hematocrit. The hematocrit of any one sample can vary significantly, however, about 36–50 percent, according to gender and other factors. Not counting the buffy coat, which makes up less than 1% of the blood, we can estimate the mean plasma percentage to be the percent of blood that is not erythrocytes: approximately 55%.
The table below provides a useful summary of the components of blood and their functions.
Table 10.3 a &b – Major Blood Components: . This table displays the components of blood and their associated functions. Adapted from Betts et al., 2013. Licensed under CC BY 4.0.
| Subcomponent and % of Component |
Type and % (Where appropriate) | Site of production |
Major function(s) |
|---|---|---|---|
| Water 92 percent | Fluid | Absorbed by intestinal tract or produced by metabolism | Transport medium |
| Plasma protein – Albumin | Albumin 54 – 60 percent | Liver | Maintain osmotic concentration, transport lipid molecules |
| Plasma protein – Alpha Globulins | Globulins (35 – 38 percent overall) | Alpha globulins – liver | Transport, maintain osmotic concentration |
| Plasma protein – Beta globulins | Globulins 35 – 38 percent (35 – 38 percent overall) | Beta globulins – liver | Transport, maintain osmotic concentration |
| Plasma protein – Gamma Globulins | Globulins 35 – 38 percent (35 – 38 percent overall) | Gamma globulins (immunoglobulins) – plasma cells | Immune responses |
| Plasma protein – Fibrinogen | Fibrinogen 4 – 7 percent | Liver | Blood clotting in hemostasis |
| Regulatory proteins < 1 percent | Hormones and enzymes | Various sources | Regulate various body functions |
| Other solutes 1 percent | Nutrients, gases, and wastes | Absorbed by intestinal tract, exchanged in respiratory system, or produced by cells | Numerous and varied |
| Subcomponent and % of Component | Type and % (Where appropriate) | Site of production | Major function(s) |
|---|---|---|---|
| Erythrocytes 99 percent | Erythrocytes | Red bone marrow | Transport gases, primarily oxygen and some carbon dioxide |
|
Leukocytes (overall) |
Granular Leukocytes: neutrophils eosinophils basophils |
Red bone marrow | Nonspecific immunity |
|
Leukocytes (overall) |
Agranular leukocytes: lymphocytes |
Lymphocytes: bone marrow and lyphatic tissue |
Lymphocytes: specific immunity |
|
Leukocytes (overall) |
Agranular leukocytes: monocytes |
Monocytes: redbone marrow | Monocytes: nonspecific immunity |
| Platelets < 1 percent |
n/a | Megakaryocytes: Red Bone Marrow |
Hemostasis |
Concept Check 1
Use the table above to answer these questions:
- What substance makes up most of the plasma?
- What are some general functions of plasma and its components?
- What is the function of erythrocytes?
- What is the overall function of leukocytes? (Hint: which word appears in all 3 chart cells that list leukocyte functions?)
- What is the function of platelets?
Blood Plasma
Like other fluids in the body, plasma is composed primarily of water. In fact, it is about 92% water. Dissolved or suspended within this water is a mixture of substances, most of which are proteins. The major components of plasma and their functions are summarized in the table above.
Formed Elements (Erythrocytes, Leukocytes, Thrombocytes)
Table 10.4a below summarizes the main facts about the formed elements in blood. Table 10.4b shows a more in-depth look at Leukocytes (white blood cells).
| Formed Element |
Major Subtypes |
Number Present per Microliter (µL) and Mean Range | Appearance in a Standard Blood Smear | Summary of Functions | Comments |
|---|---|---|---|---|---|
|
Erythrocytes (red blood cells)  |
n/a | 5.2 million ( 4.4-5.0 million) | Flattened biconcave disk; no nucleus; pale red colour | Transport oxygen and some carbon dioxide between tissues and lungs | Lifespan of approximately 120 days |
| Leukocytes (white blood cells) | n/a | 7000 (5000 – 10,000) | Obvious dark-staining nucleus | All function in body defenses | Exit capillaries and move into tissues; lifespan of usually a few hours or days |
|
Platelets  |
n/a | 350,000 (150,000 – 500,000) | Cellular fragments surrounded by a plasma membrane and containing granules; purple stain | Hemostasis plus release growth factors for repair and healing of tissue | Formed from megakaryocytes that remain in the red bone marrow and shed platelets into circulation |
| Major Subtypes | Number Present per Microliter (µL) and Mean Range | Appearance in a Standard Blood Smear | Summary of Functions | Comments |
|---|---|---|---|---|
| Granulocytes including neutrophils, eosinophils, and basophils | 4360 (1800-9950) | Abundant granules in cytoplasm; nucleus normal lobed | Nonspecific (innate) resistance to disease | Classified according to membrane-bound granules in cytoplasm |
Neutrophils
 |
4150 (1800-7300) | Nuclear lobes increase with age; pale lilac granules | Phagocytic; particularly effective against bacteria. Release cytotoxic chemicals from granules | Most common leukocyte; lifespan of minutes to days |
Eosinophils
 |
165 (0-700) | Nucleus generally two-lobed; bright red-orange granules | Phagocytic cells; particularly effective with antigen-antibody complexes. Release antihistamines. Increase in allergies and parasitic infections | Lifespan of minutes to days |
Basophils
 |
44 (0-150) | Nucleus generally two-lobed but difficult to see due to presence of heavy, dense, dark purple granules | Promotes inflammation | Least common leukocyte; lifespan unknown |
| Agranulocytes including lymphocytes and monocytes | 2640 (1700-4950) | Lack abundant granules in cytoplasm; have a simple-shaped nucleus that may be indented | Body defenses | Group consists of two major cell types from different lineages |
Lymphocytes
 |
2185 (1500-4000) | Spherical cells with a single often large nucleus occupying much of the cell’s volume; stains purple; see in large (natural killer cells) and small (B and T cells) variants | Primarily specific (adaptive) immunity; T cells directly attack other cells (cellular immunity). B cells release antibodies (humoral immunity); natural killer cells are similar to T cells but nonspecific | Initial cells originate in bone marrow, but secondary production occurs in lymphatic tissue; several distinct subtypes; memory cells form after exposure to a pathogen and rapidly increase responses to subsequent exposure; lifespan of many years |
Monocytes
 |
455 (200-950) | Largest leukocyte with an indented or horseshoe-shaped nucleus | Very effective phagocytic cells engulfing pathogens or worn out cells; also serve as antigen-presenting cells (APCs) for other components of the immune system | Produced in red bone marrow; referred to as macrophages after leaving circulation |
Hemopoiesis/Hematopoiesis
The lifespan of the formed elements is very brief. Although one type of leukocyte (memory cells) can survive for years, most erythrocytes, leukocytes, and platelets normally live only a few hours to a few weeks. Thus, the body must form new blood cells and platelets quickly and continuously, a process known as hemopoiesis.
In children, hemopoiesis can occur in the medullary cavity of long bones; in adults, the process is largely restricted to the cranial and pelvic bones, the vertebrae, the sternum, and the proximal epiphyses of the femur and humerus. Throughout adulthood, the liver and spleen maintain their ability to generate the formed elements. This process is referred to as extramedullary hemopoiesis. When a disease such as bone cancer destroys the bone marrow, causing hemopoiesis to fail, extramedullary hemopoiesis may be initiated .
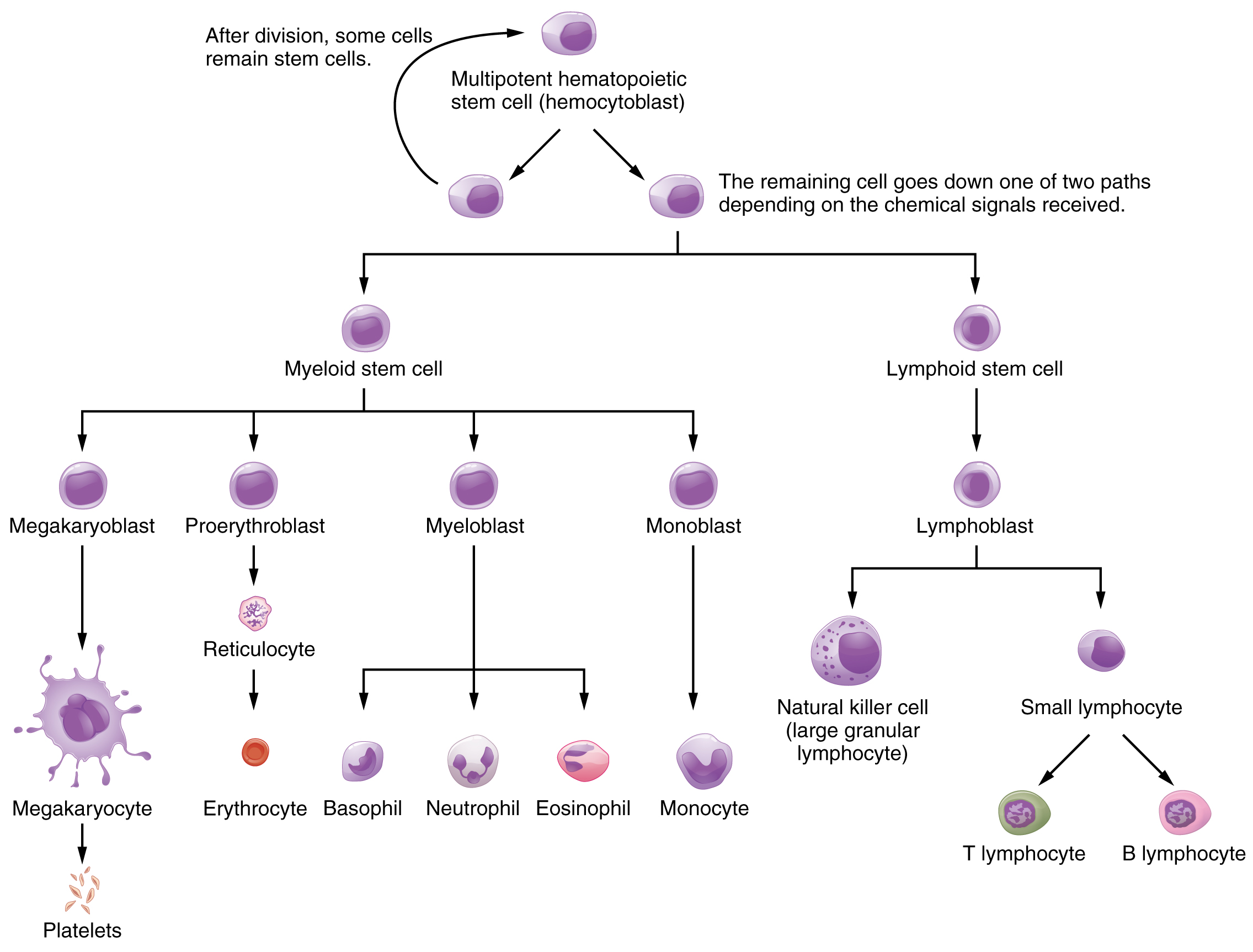
All formed elements arise from stem cells of the red bone marrow, called hemopoietic stem cell, or hemocytoblast. Hemopoiesis begins when the hemopoietic stem cell is exposed to appropriate chemical stimuli collectively called hemopoietic growth factors, which prompt it to divide and differentiate. One daughter cell remains a hemopoietic stem cell, allowing hemopoiesis to continue. The other daughter cell becomes either of two types of more specialized stem cells. Follow the chart below from top to bottom to learn how stem cells become mature formed elements of blood.
Erythrocytes
The most abundant formed elements in blood, erythrocytes are basically sacs packed with an oxygen-carrying compound called hemoglobin. Production of erythrocytes in the red bone marrow occurs at the staggering rate of more than 2 million cells per second. For this production to occur, raw materials including iron, copper, zinc B-vitamins, glucose, lipids, and amino acids must be present in adequate amounts. Erythrocytes live only 120 days on average, and thus must be continually replaced. Worn-out erythrocytes are phagocytized by macrophages and their hemoglobin is broken down. The breakdown products are recycled or removed as wastes.
Leukocytes
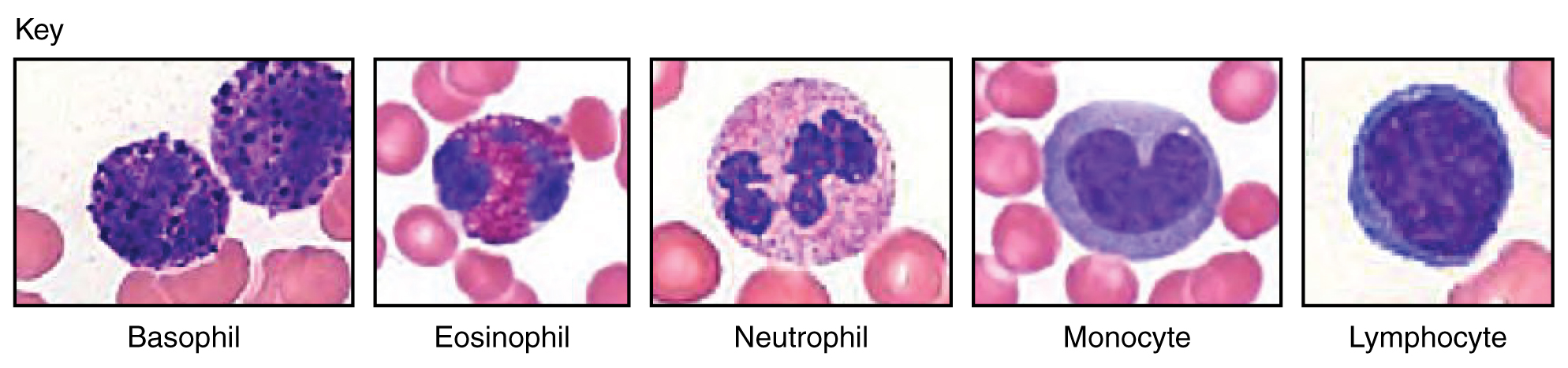
Leukocytes protect the body against invading microorganisms and body cells with mutated DNA, and they clean up debris, thus they are a major component of the body’s defenses against disease. Figure 13.10 shows the different types of leukocytes.
Concept Check 2
- What is hemoglobin?
- Can you name the 5 types of leukocytes?
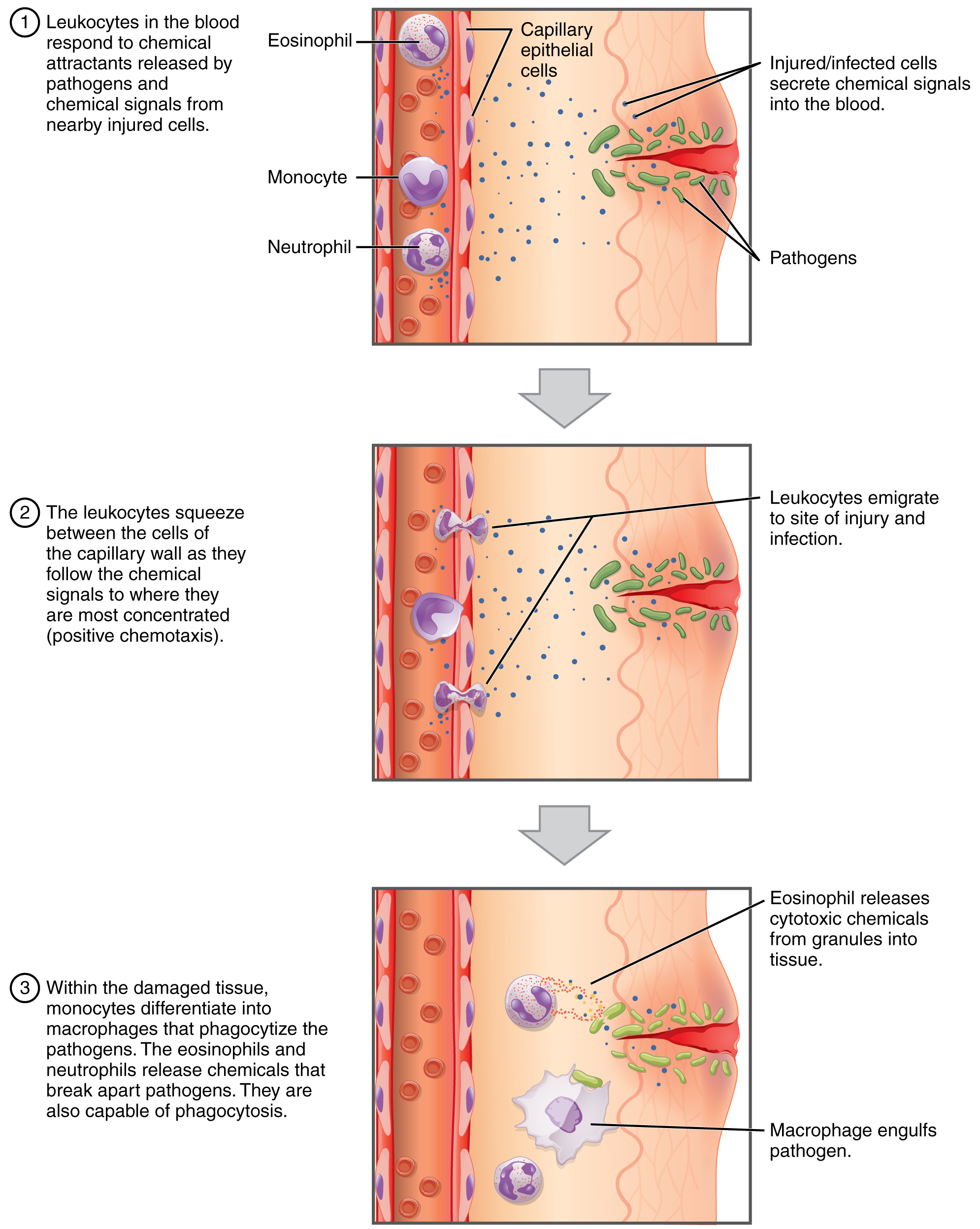
Leukocytes routinely leave the bloodstream to perform their defensive functions in the body’s tissues, where they are often given distinct names, such as macrophage or microglia, depending on their function. As shown in Figure 1 below, they leave the capillaries—the smallest blood vessels—or other small vessels through a process known as emigration or diapedesis in which they squeeze through adjacent cells in a blood vessel wall.
Once they have exited the capillaries, some leukocytes will take up fixed positions in lymphatic tissue, bone marrow, the spleen, the thymus, or other organs. Others will move about through the tissue spaces, sometimes wandering freely, and sometimes moving toward the direction in which they are drawn by chemical signals, a mechanism known as positive chemotaxis.
Lymphocytes
Lymphocytes are one of the types of leukocytes and will be discussed in more detail here, since they tie into the next chapter which discussed the body’s defenses The three major groups of lymphocytes include natural killer cells, B cells, and T cells.
-
- Natural killer (NK) cells are capable of recognizing cells that do not express “self” proteins on their plasma membrane or that contain foreign or abnormal markers. These “non-self” cells include cancer cells, cells infected with a virus, and other cells with atypical surface proteins.
- B lymphocytes (B cells) and T lymphocytes (T cells), play prominent roles in defending the body against specific pathogens (disease-causing microorganisms) and are involved in specific immunity. B cells undergo a maturation process in the bone marrow, whereas T cells undergo maturation in the thymus. This site of the maturation process gives rise to the name B and T cells.
- Plasma cells, a type of B cell, produce the antibodies or immunoglobulins that bind to specific foreign or abnormal components of plasma membranes.
- T cells provide immunity by physically attacking foreign or diseased cells.
- Memory cells are a variety of both B and T cells that form after exposure to a pathogen and mount rapid responses upon subsequent exposures. Unlike other leukocytes, memory cells live for many years.
Platelets
After entering the circulation, approximately one-third of the newly-formed platelets migrate to the spleen for storage for later release in response to any rupture in a blood vessel. They then become activated to perform their primary function, which is to limit blood loss. Platelets remain only about 10 days, then are phagocytized by macrophages.
Platelets are key players in hemostasis, the process by which the body seals a ruptured blood vessel and prevents further loss of blood. Although rupture of larger vessels usually requires medical intervention, hemostasis is quite effective in dealing with small, simple wounds. There are three steps to the process: vascular spasm, the formation of a platelet plug, and coagulation (blood clotting). Failure of any of these steps will result in hemorrhage. The figure below summarizes the steps of hemostatis.
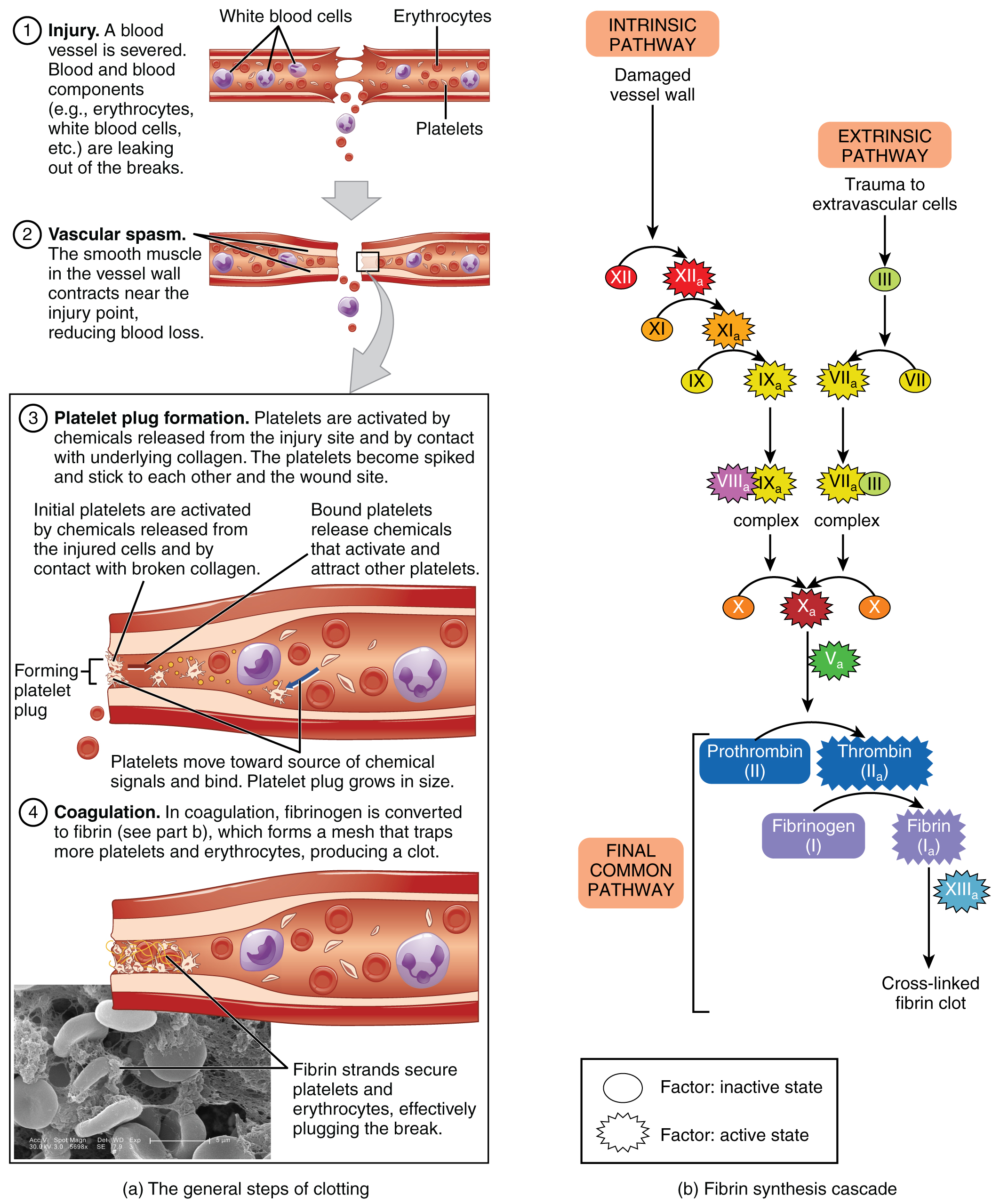
Fibrinolysis is the process in which a clot is degraded in a healing vessel. An anticoagulant is any substance that opposes coagulation. Several circulating plasma anticoagulants play a role in limiting the coagulation process to the region of injury and restoring a normal, clot-free condition of blood.
Concept Check 3
- Can you explain what happens in each step of hemostasis?
- Describe an anticoagulant.
Physiology of Blood
Although carrying oxygen and nutrients to cells and removing wastes from cells is the main function of blood, it is important to realize that blood also serves in defense, distribution of heat, and maintenance of homeostasis.
Transportation
- Nutrients from the foods you eat are absorbed in the digestive tract. Most of these travel in the bloodstream directly to the liver, where they are processed and released back into the bloodstream for delivery to body cells.
- Oxygen from the air you breathe diffuses into the blood, which moves from the lungs to the heart, which then pumps it out to the rest of the body.
- Endocrine glands scattered throughout the body release their products, called hormones, into the bloodstream, which carries them to distant target cells.
- Blood also picks up cellular wastes and byproducts, and transports them to various organs for removal. For instance, blood moves carbon dioxide to the lungs for exhalation from the body, and various waste products are transported to the kidneys and liver for excretion from the body in the form of urine or bile.
Defense
- Leukocytes protect the organism from disease-causing bacteria, cells with mutated DNA that could multiply to become cancerous, or body cells infected with viruses.
- When damage to the vessels results in bleeding, blood platelets and certain proteins dissolved in the plasma, interact to block the ruptured areas of the blood vessels involved. This protects the body from further blood loss.
Homeostasis
- If you were exercising on a warm day, your rising core body temperature would trigger several homeostatic mechanisms, including increased transport of blood from your core to your body periphery, which is typically cooler. As blood passes through the vessels of the skin, heat would be dissipated to the environment, and the blood returning to your body core would be cooler. In contrast, on a cold day, blood is diverted away from the skin to maintain a warmer body core. In extreme cases, this may result in frostbite.
- Blood helps to regulate the water content of body cells.
- Blood also helps to maintain the chemical balance of the body. Proteins and other compounds in blood act as buffers, which thereby help to regulate the pH of body tissues. The pH of blood ranges from 7.35 to 7.45.
Concept Check 4
These three terms all sound similar. Can you explain them by breaking down the word parts?
- Hemostasis
- Homeostasis
- Hemopoiesis
Blood Types
In order to understand blood types, it is important to understand several terms that relate to the body’s immune functions (discussed in detail in the next chapter).
- Antigens are substances that the body does not recognize as belonging to itself (“self”) and that therefore trigger a defensive response from the leukocytes of the immune system. Many people have antigens on the surfaces of their red blood cells. More than 50 antigens have been identified on erythrocyte membranes, but the most significant in terms of their potential harm to patients are classified in two groups: the ABO blood group and the Rh blood group.
- Antibodies are proteins which are produced by plasma cells in response to a “non-self” antigen being present in the body. Antibodies attach to the antigens on the plasma membranes of the erythrocytes in a blood transfusion and cause them to adhere to one another.
- Agglutination refers to the resulting clumps of red blood cells that are formed in such an antigen-antibody reaction. These clumps can block small blood vessels, thereby cutting of the supply of oxygen and nutrients to the tissues.
- Hemolysis, or the breakdown of the erythrocyte’s cell membrane, takes place as the clumps of red cells start to degrade. The resulting release of the cell’s contents, mainly hemoglobin, into the bloodstream can cause kidney failure.
ABO Blood Group
ABO blood types are genetically determined. Each type is determined by the presence or absence of certain antigens on the individual’s red blood cell membrane, as well as the presence or absence of certain antibodies. Normally the body must be exposed to a foreign antigen before an antibody can be produced. This is not the case for the ABO blood group, in which some blood types come preloaded with their own set of antibodies against another type. The table below shows the ABO blood group as well as the universal donor and recipient in relation to blood transfusions.
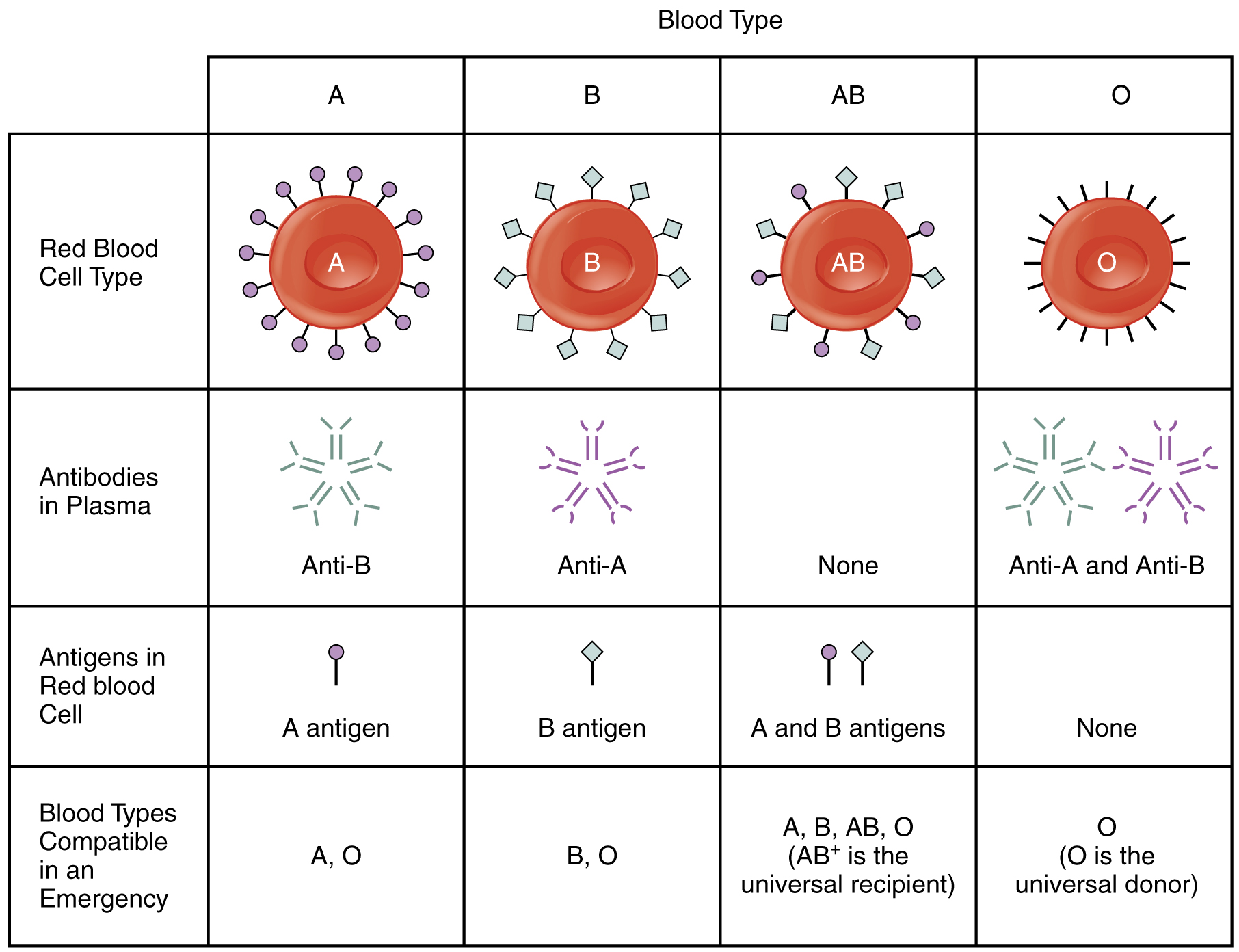
- Blood Type A
- People whose erythrocytes have A antigens on their erythrocyte membrane surface.
- People who have type A blood, without any prior exposure to incompatible blood, have preformed anti-B antibodies circulating in their blood. These antibodies will cause a serious immune reaction if they encounter blood that has B antigens.
- Blood Type B
- People whose erythrocytes have B antigens.
- People with type B blood have preformed anti-A antibodies.
- Blood Type AB
- People can also have both A and B antigens on their erythrocytes, in which case they are blood type AB.
- Individuals with type AB blood, do not have preformed antibodies to either A or B antigens.
- Blood Type O
- People with neither A nor B antigens are designated blood type O.
- People with type O blood have both anti-A and anti-B antibodies circulating in their blood plasma.
Rh Blood Group
The Rh blood group is classified according to the presence or absence of a second erythrocyte antigen identified as Rh. Those who have the Rh D antigen present on their erythrocytes are described as Rh positive (Rh+) and those who lack it are Rh negative (Rh−). Note that the Rh group is distinct from the ABO group, so any individual, no matter their ABO blood type, may have or lack this Rh antigen. When identifying a patient’s blood type, the Rh group is designated by adding the word positive or negative to the ABO type. For example, A positive (A+) means ABO group A blood with the Rh antigen present, and AB negative (AB−) means ABO group AB blood without the Rh antigen.
Hemolytic Disease of the Newborn (HDN)
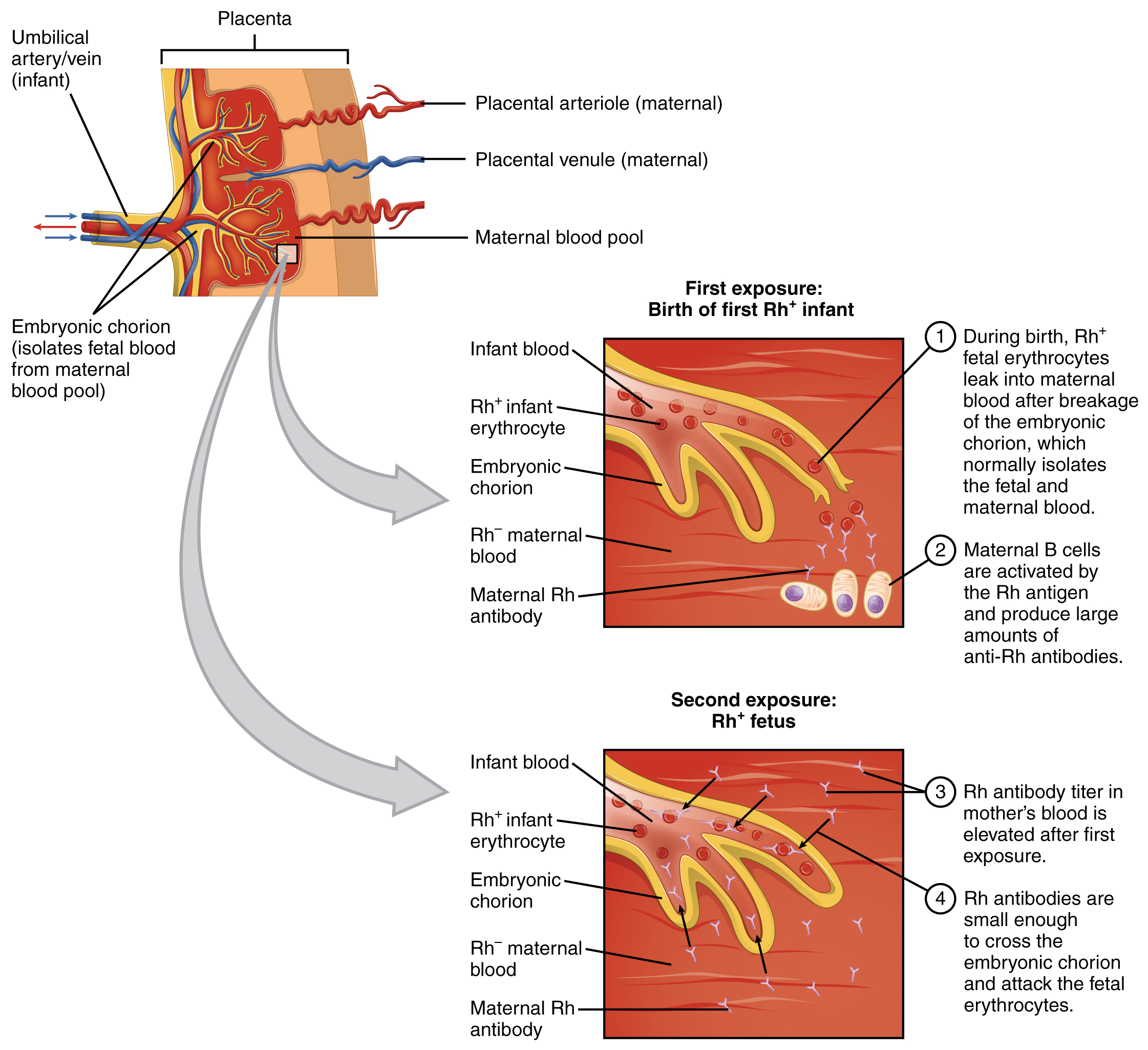
Antibodies to the Rh antigen are produced only in Rh− individuals after exposure to the antigen. This process, called sensitization, occurs following a transfusion with Rh-incompatible blood or, more commonly, with the birth of an Rh+ baby to an Rh− mother.
- In a first pregnancy, problems are rare, since the baby’s Rh+ cells rarely cross the placenta. However, during or immediately after birth, the Rh− mother can be exposed to the baby’s Rh+ cells (Figure below). Research has shown that this occurs in about 13−14 percent of such pregnancies. After exposure, the mother’s immune system begins to generate anti-Rh antibodies.
- In a second pregnancy, if a mother should conceive a Rh+ baby, the Rh antibodies she has produced can cross the placenta into the fetal bloodstream and destroy the fetal RBCs. This condition is known as hemolytic disease of the newborn (HDN) or erythroblastosis fetalis. This may cause anemia in mild cases, but the agglutination and hemolysis can be so severe that without treatment the fetus may die in the womb or shortly after birth.
- A drug known as RhoGAM, short for Rh immune globulin, can temporarily prevent the development of Rh antibodies in the Rh− mother, thereby averting this potentially serious disease for the fetus. RhoGAM antibodies destroy any fetal Rh+ erythrocytes that may cross the placental barrier. RhoGAM is normally administered to Rh− mothers during weeks 26−28 of pregnancy and within 72 hours following birth.
Blood Transfusions
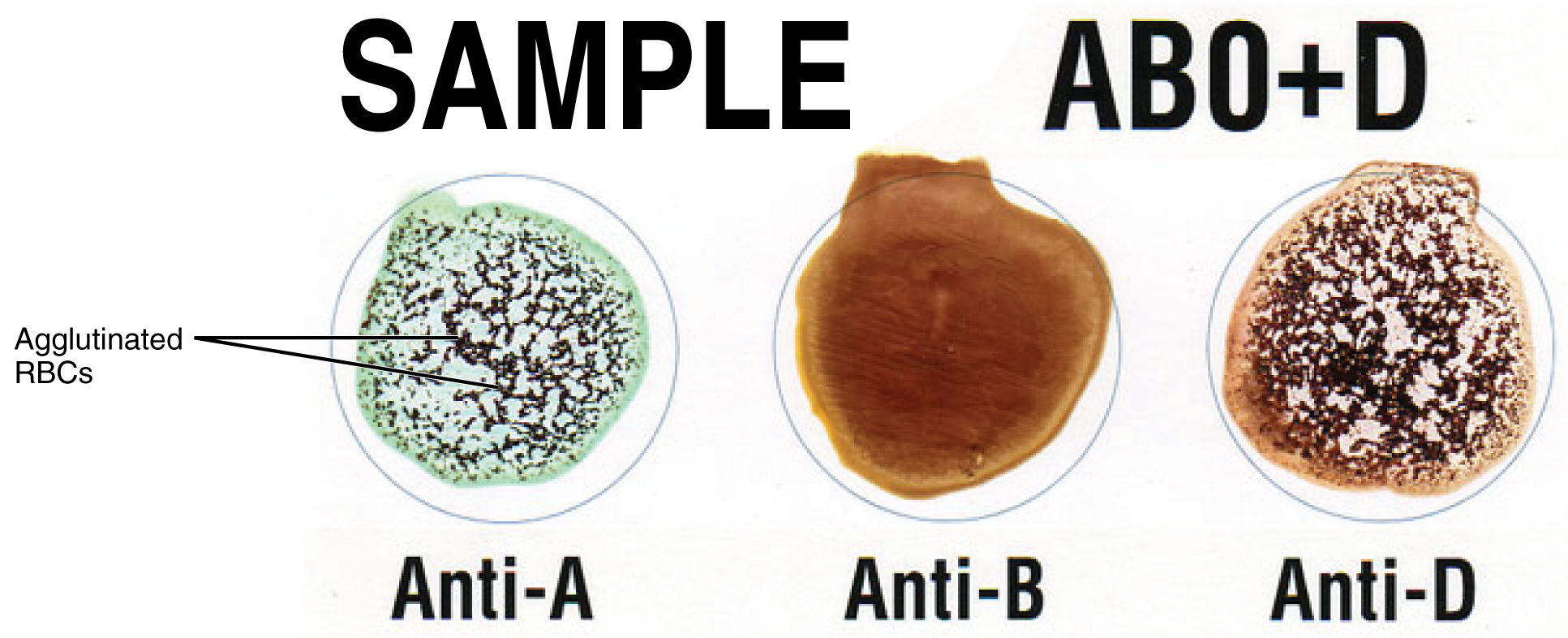
Figure 10.15 is an example of a commercially produced “bedside” card which enables quick typing of both a recipient’s and donor’s blood before transfusion. The card contains three reaction sites or wells. One is coated with an anti-A antibody, one with an anti-B antibody, and one with an anti-D antibody (tests for the presence of Rh factor D). Mixing a drop of blood and saline into each well enables the blood to interact with a preparation of type-specific antibodies, also called anti-seras. Agglutination of RBCs in a given site indicates a positive identification of the blood antigens, in this case A and Rh antigens for blood type A+. To avoid serious and potentially fatal immune reactions, the donor’s and recipient’s blood types must match
To avoid transfusion reactions, it is best to transfuse only matching blood types; that is, a type B+ recipient should ideally receive blood only from a type B+ donor and so on. That said, in emergency situations, when acute hemorrhage threatens the patient’s life, there may not be time for cross matching to identify blood type. In these cases, blood from a universal donor may be transfused.
Blood Vessel Medical Terms Word Parts
Blood Vessel Medical Terms Not Easily Broken into Word Parts
Cardiovascular System – Blood Terms Not Easily broken down (Text Version)
Practice the following cardiovascular blood terms by breaking into word parts and pronouncing.
- phlebotomist
- A specially trained person who draws blood or injects IV fluids
- anaphylaxis
- exaggerated reaction to a previously encountered antigen may start out as mild reaction but can quickly become severe resulting in anaphylactic shock
- anemia
- reduction in number of erythrocytes
- immunodeficiency
- deficient immune response caused by immune system dysfunction brought on by disease or immune suppressive drugs.
- ischemia
- condition of deficient blood flow due to a constriction or obstruction of a blood vessel
- sepsis
- toxic condition due to spread of bacteria or their toxins from an infection
Activity source: “Cardiovascular System – Blood Terms Not Easily Broken Down” by Kimberlee Carter, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. / Text version added.
Image Descriptions
Figure 10.5 image description: This diagram shows how oxygenated and deoxygenated blood flow through the major organs in the body. Pulmonary circulation involves the lungs, pulmonary artery and vein, vena cava, and aorta. Systemic circulation involves the upper body, hepatic vein, renal vein, aorta, liver, hepatic artery, hepatic portal vein, stomach, intestines, renal artery, kidneys, and lower body. [Return to Figure 10.5].
Figure 10.6 image description: The pulse points as shown on a woman’s body. Labels read (from top) temporal artery, facial artery, common carotid artery, brachial artery, radial artery, femoral artery, popliteal artery, posterior tibial artery, dorsalis pedis artery. [Return to Figure 10.6].
Figure 10.7 image description: This figure shows three test tubes with a red and yellow liquid in them. The left panel shows normal blood, the center panel shows anemic blood and the right panel shows polycythemic blood. Labels indicate plasma (water, proteins, nutrients, hormones etc.), buffy coat (white blood cells, platelets), and hematocrit (red blood cells). [Return to Figure 10.7].
Figure 10.8 image description: This flowchart shows the pathways in which a multipotent hemotopoietic stem cell differentiates into the different cell types found in blood. From the top (multipotent hematopoietic stem cell can divide and some cells remain stem cells, while the remaining cell goes down one of two paths depending on the chemical signals received: myleoid stem cell or lymphoid stem cell. A myeloid stem cell then can become either a megakaryoblast (which then turns into a magakaryocyte, then becomes platelets), or it can become a proerythroblas (which then becomes a reticulocyte, then becoming an erythrocite), or it can become a myeloblast (which then becomes either a basophil, neutrophil, eosinophil), or it can become a monoblast (which then becomes a monocyte). If the cell becomes a lymphoid stem cell, it then becomes a lymphoblas, which then becomes either a natural killer cell or a small lymphocyte (either T or B lymphocyte). [Return to Figure 10.8].
Figure 10.11 image description: This figure shows how leukocytes respond to chemical signals from injured cells. The top panel shows chemical signals sent out by the injured cells (text labels read: 1) Leukocytes in the blood respond to chemical attractants released by pathogens and chemical signals from nearby injured cells). The middle panel shows leukocytes migrating to the injured cells (text labels read: 2) the leukocytes squeeze between the capillary wall as they follow the chemical signals to where they are most concentrated (positive chemotaxis)). The bottom panel shows macrophages phagocytosing the pathogens (text label reads: 3) Within the damaged tissue, monocytes differentiate into macrophages that phagocytize the pathogens. The eosinophils and neutrophils release chemicals that break apart pathogens. They are also capable of phagocytosis). [Return to Figure 10.11].
Figure 10.12 image description: This figure details the steps in the clotting of blood. Each step is shown along with a detailed text box describing the steps on the left. On the right, a signaling pathway shows the different chemical signals involved in the clotting process. The steps described: 1. Injury: a blood vessel is severed. Blood and blood components (e.g. erythrocytes, white blood cells, etc.) are leaking out of the breaks. 2. Vascular spasm: the smooth muscle in the vessel wall contracts near the injury point reducing blood loss. 3. Platelet plug formation: platelets are activated by chemicals released from the injury site and by contact with underlying collagen. The platelets become spiked and stick to each other and the wound site. Initial platelets are activated by chemicals released from the injured cells and by contact with broken collagen. Bound platelets release chemicals that activate and attract other platelets. Platelets move toward source of chemical signals and bind. Platelet plug grows in size. 4. Coagulation. In coagulation, fibrinogen is converted to fibrin (see part b), which forms a mesh that traps more platelets and erythrocytes, producing a clot. Part B Fibryn synthesis cascade: Intrinsic pathway (damaged vessel wall), Extrinsic pathway (trauma to extravascular cells), final common pathway (cross-linked fibrin clot). [Return to Figure 10.12].
Attribution
Except where otherwise noted, this chapter is adapted from “Cardiovascular System – Blood Vessels and Blood” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Cardiovascular System – Blood Vessels and Blood chapter content into sub-chapters.
large artery in the upper arm near the biceps muscle
a blood pressure cuff attached to a measuring device, or gauge
The systolic pressure is the higher value (typically around 120 mm Hg) and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole.
The diastolic pressure is the lower value (usually about 80 mm Hg) and represents the arterial pressure of blood during ventricular relaxation, or diastole.
Cardiac output is the measurement of blood flow from the heart through the ventricles, and is usually measured in liters per minute. Any factor that causes cardiac output to increase, by elevating heart rate or stroke volume or both, will elevate blood pressure and promote blood flow.
Compliance is the ability of any compartment to expand to accommodate increased content. The greater the compliance of an artery, the more effectively it is able to expand to accommodate surges in blood flow without increased resistance or blood pressure.
Viscosity is the thickness of fluids that affects their ability to flow
The number of times the heart contracts in one minute.
A centrifuge is a common piece of laboratory equipment used to spin test tubes at a high speed in order to separate components in a liquid by weight.
red blood cells
also spelled leucocyte, these are white blood cells
also called platelets, these are cell fragments that aid in blood clotting
A lab test which measures the percentage red blood cells in a sample of whole blood. It represents how much of the person's blood is made up of red blood cells, by volume.
Blood clotting cells also called thrombocytes.
also called hematopoiesis; from the Greek root haima- = “blood”; -poiesis = “production”
the ends of long bones, singular is epiphysis
hemopoiesis outside the medullary cavity of adult bones
Chemical messengers which promote the proliferation and differentiation of formed elements and include erythropoietin, thrombopoietin, colony-stimulating factors, and interleukins.
also phagocytosed, this is the process by which certain cells are able to 'eat' other cells or substances by engulfing them
a type of leukocyte (usually a monocyte) that has the ability to ingest and destroy other cells or pathogens
dia- = “through”; -pedan = “to leap”
Movement in response to chemicals; a phenomenon in which injured or infected cells and nearby leukocytes emit the equivalent of a chemical “911” call, attracting more leukocytes to the site.
excessive or uncontrolled bleeding from the blood vessels
pH is a measure of how acidic or alkaline a substance is, as determined by the number of free hydrogen ions in the substance.
A substance that provokes an immune response. This happens because the immune system sees the antigen as foreign, or 'non-self" (does not belong in that body)
also called immunoglobulins, proteins produced by B lymphocytes in response to a non-self antigen
A type of B lymphocyte that produces antibodies which bind to specific foreign or abnormal antigens, in order to destroy them
Breaking apart of the erythrocyte cell membrane, allowing its contents to leak out
proteins that will mount an immune response against B antigens
the organ of gas and nutrient exchange between the baby and the mother

