10.4 – Blood Vessels Diseases, Disorders and Diagnostic Testing
Common Diseases and Disorders of Blood Vessels and/or Blood
Arteriosclerosis
Arteriosclerosis is normally defined as the more generalized loss of compliance, “hardening of the arteries,” whereas atherosclerosis is a more specific term for the build-up of plaque in the walls of the vessel and is a specific type of arteriosclerosis.
When arteriosclerosis causes vessel compliance to be reduced, pressure and resistance within the vessel increase. This is a leading cause of hypertension and coronary heart disease, as it causes the heart to work harder to overcome this resistance. Any artery in the body can be affected by these pathological conditions, and individuals who have pathologies like coronary artery disease may also be at risk for other vascular injuries, like strokes or peripheral arterial disease.
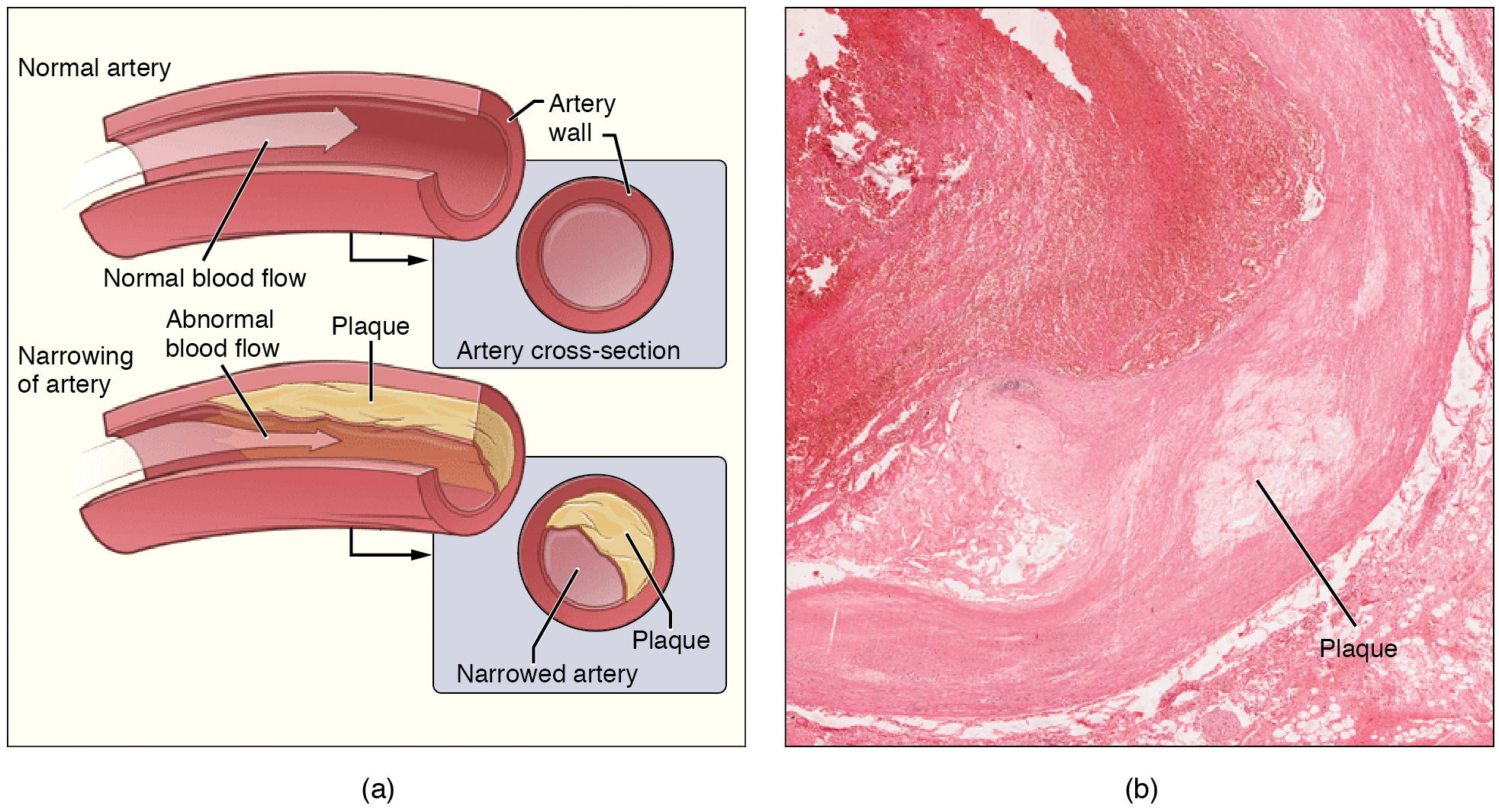
Atherosclerosis is a type of arteriosclerosis in which plaques form when circulating triglycerides, cholesterol and other substances seep between the damaged endothelial lining cells and become trapped within the artery wall, resulting in narrowed arteries and impaired blood flow (see Figure 10.16) (Betts et al., 2013).
Sometimes a plaque can rupture, causing microscopic tears in the artery wall that allow blood to leak into the tissue on the other side. When this happens, platelets rush to the site to clot the blood. This clot can further obstruct the artery and—if it occurs in a coronary or cerebral artery—cause a sudden heart attack or stroke. Alternatively, plaque can break off and travel through the bloodstream as an embolus until it blocks a more distant, smaller artery.
Peripheral arterial disease (PAD, also called peripheral vascular disease, PVD), occurs when atherosclerosis affects arteries in the legs. A major risk factor for both arteriosclerosis and atherosclerosis is advanced age, as the conditions tend to progress over time. There is also a distinct genetic component, and pre-existing hypertension and/or diabetes also greatly increase the risk. However, obesity, poor nutrition, lack of physical activity, and tobacco use all are major risk factors.
Treatment of atherosclerosis includes lifestyle changes, such as weight loss, smoking cessation, regular exercise, and adoption of a diet low in sodium and saturated fats. Medications to reduce cholesterol and blood pressure may be prescribed. For blocked coronary arteries, angioplasty or coronary artery bypass graft (CABG) surgery may be warranted. In an carotid endarterectomy, plaque is surgically removed from the walls of a the carotid artery, which is the main source of oxygenated blood for the brain (Betts et al., 2013).
Edema and Varicose Veins
Despite the presence of valves and the contributions of other anatomical and physiological adaptations that assist in moving blood through veins, over the course of a day, some blood will inevitably pool, especially in the lower limbs, due to the pull of gravity. Any blood that accumulates in a vein will increase the pressure within it, which can then be reflected back into the smaller veins, venules, and eventually even the capillaries. This increased pressure in the capillaries will push of fluids out of the capillaries and into the interstitial fluid, causing a condition called edema.
Most people experience a daily accumulation of tissue fluid, especially if they spend much of their work life on their feet (like most health professionals). However, clinical edema goes beyond normal swelling and requires medical treatment. Edema has many potential causes, including hypertension and heart failure, severe protein deficiency, renal failure, and many others. In order to treat edema, which is a sign rather than a discrete disorder, the underlying cause must be diagnosed and alleviated.

Edema may be accompanied by varicose veins, especially in the superficial veins of the legs (see Figure 10.17). This disorder arises when defective valves allow blood to accumulate within the veins, causing them to distend, twist, and become visible on the surface of the skin. Varicose veins may occur in both sexes, but are more common in women and are often related to pregnancy. More than simple cosmetic blemishes, varicose veins are often painful and sometimes itchy or throbbing. Without treatment, they tend to grow worse over time. The use of support hose, as well as elevating the feet and legs whenever possible, may be helpful in alleviating this condition (Betts, et al., 2013).
Hypertension
Hypertension is defined as chronic and persistent blood pressure measurements of 140/90 mm Hg or above. Pressures between 120/80 and 140/90 mm Hg are defined as prehypertension. Hypertension is typically a silent disorder and patients may fail to recognize the seriousness of their condition and fail to follow their treatment plan, putting them at risk for a heart attack or stroke. Hypertension may also lead to an aneurysm, peripheral arterial disease, chronic kidney disease, or heart failure (Betts et al., 2013).
Hemorrhage
Minor blood loss is managed by hemostasis and repair. Hemorrhage is a loss of blood that cannot be controlled by hemostatic mechanisms. Initially, the body responds to hemorrhage by initiating mechanisms aimed at increasing blood pressure and maintaining blood flow. Ultimately, however, blood volume will need to be restored, either through physiological processes or through medical intervention. If blood loss is less than 20 percent of total blood volume, fast-acting homeostatic mechanisms causing increased cardiac output and vasoconstriction would usually return blood pressure to normal and redirect the remaining blood to the tissues. Blood volume will then need to be restored via slower-acting homeostatic mechanisms to increase body fluids and erythrocyte production (Betts et al., 2013).
Circulatory Shock
The loss of too much blood may lead to circulatory shock, a life-threatening condition in which the circulatory system is unable to maintain blood flow to adequately supply sufficient oxygen and other nutrients to the tissues to maintain cellular metabolism. It should not be confused with emotional or psychological shock. Typically, the patient in circulatory shock will demonstrate an increased heart rate but decreased blood pressure. Urine output will fall dramatically, and the patient may appear confused or lose consciousness. Unfortunately, shock is an example of a positive-feedback loop that, if uncorrected, may lead to the death of the patient (Betts et al., 2013).
There are several recognized forms of shock:
- Hypovolemic shock in adults is typically caused by hemorrhage, although in children it may be caused by fluid losses related to severe vomiting or diarrhea.
- Cardiogenic shock results from the inability of the heart to maintain cardiac output. Most often, it results from a myocardial infarction (heart attack), but it may also be caused by arrhythmias, valve disorders, cardiomyopathies, cardiac failure, or simply insufficient flow of blood through the cardiac vessels.
- Vascular shock occurs when arterioles lose their normal muscular tone and dilate dramatically. It may arise from a variety of causes, and treatments almost always involve fluid replacement and medications, called inotropic or pressor agents, which restore tone to the muscles of the vessels.
- Anaphylactic shock is a severe allergic response that causes the widespread release of histamines, triggering vasodilation throughout the body.
- Obstructive shock, as the name would suggest, occurs when a significant portion of the vascular system is blocked. It is not always recognized as a distinct condition and may be grouped with cardiogenic shock, including pulmonary embolism and cardiac tamponade. Treatments depend upon the underlying cause and, in addition to administering fluids intravenously, often include the administration of anticoagulants, removal of fluid from the pericardial cavity, or air from the thoracic cavity, and surgery as required. The most common cause is a pulmonary embolism. Other causes include stenosis of the aortic valve, cardiac tamponade, and a pneumothorax (Betts et al., 2013).
Blood Disorders
Erythrocyte Disorders
Changes in the levels of RBCs can have significant effects on the body’s ability to effectively deliver oxygen to the tissues (Betts et al., 2013).
Did You Know?
‘O2 sat’ or ‘percent sat’ is the percent saturation, that is, the percentage of hemoglobin sites occupied by oxygen in a patient’s blood.
Anemia
The size, shape, and number of erythrocytes, and the number of hemoglobin molecules can have a major impact on a person’s health. When the number of RBCs or hemoglobin is deficient, the general condition is called anemia. There are more than 400 types of anemia.
Anemia can be broken down into three major groups: those caused by blood loss, those caused by faulty or decreased RBC production, and those caused by excessive destruction of RBCs. In addition to these causes, various disease processes also can lead to anemias. These include chronic kidney diseases often associated with a decreased production of EPO, hypothyroidism, some forms of cancer, lupus, and rheumatoid arthritis (Betts, et al., 2013).
Blood Loss Anemias:
Causes:
- Bleeding from wounds or other lesions, including ulcers, hemorrhoids, inflammation of the stomach (gastritis), and some cancers of the gastrointestinal tract.
- The excessive use of aspirin or other nonsteroidal anti-inflammatory drugs such as ibuprofen can trigger ulceration and gastritis.
- Excessive menstruation and loss of blood during childbirth.
Anemias Caused by Faulty or Decreased RBC Production:
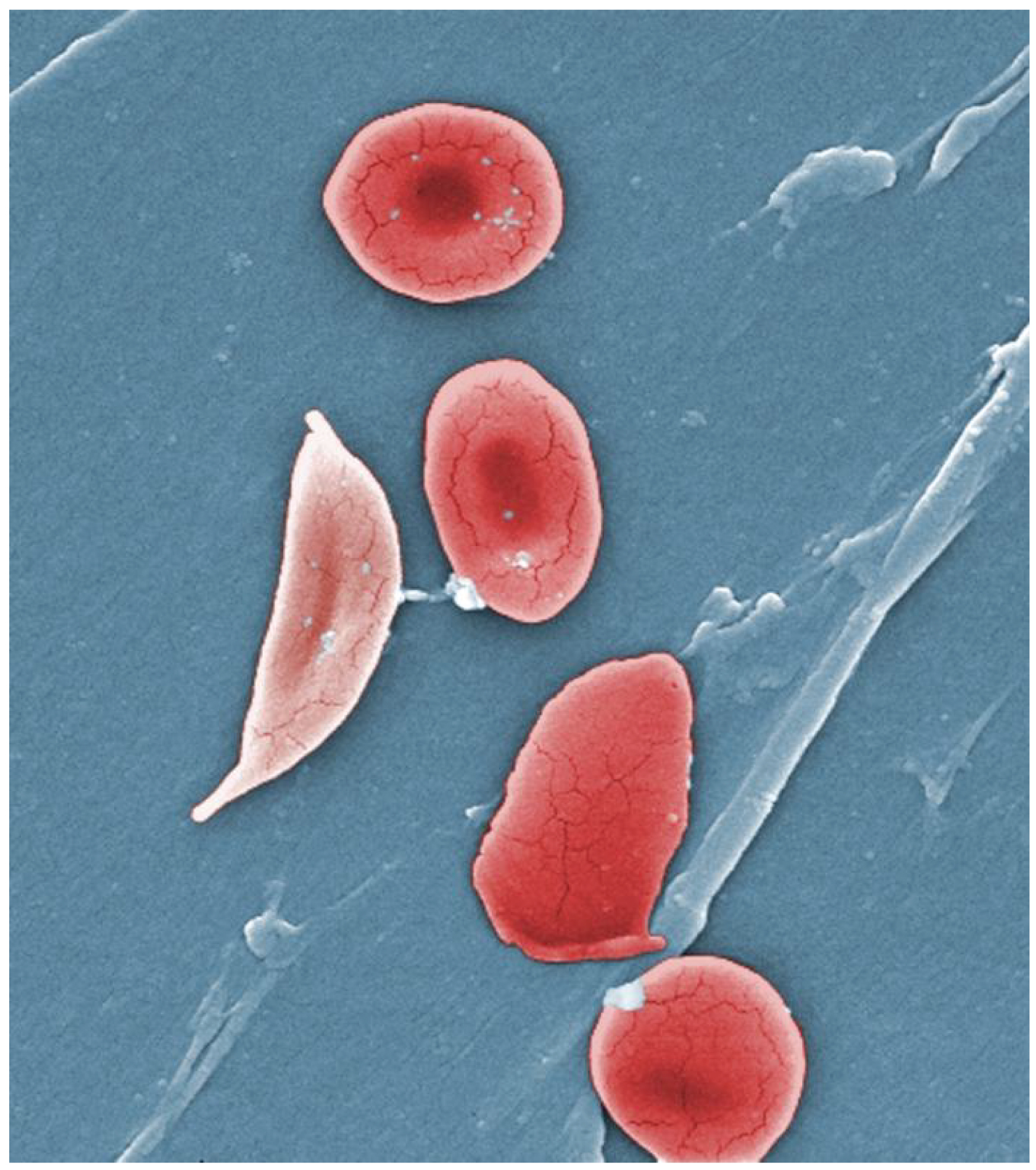
- Sickle cell anemia
-
- A genetic disorder involving the production of an abnormal type of hemoglobin which delivers less oxygen to tissues and causes erythrocytes to assume a sickle (or crescent) shape.
- Iron deficiency anemia
- The most common type of anemia and results when the amount of available iron is insufficient to allow production of sufficient heme.
- Vitamin deficiency anemia (Generally insufficient vitamin B12 and folate).
- Megaloblastic anemia involves a deficiency of vitamin B12 and/or folate, often due to inadequate dietary intake.
- Pernicious anemia is caused by poor absorption of vitamin B12 and is often seen in patients with Crohn's disease, surgical removal of the intestines or stomach (common in some weight loss surgeries), intestinal parasites, and AIDS.
- Aplastic anemia is the condition in which myeloid stem cells are defective or replaced by cancer cells, resulting in insufficient quantities of RBCs being produced. This condition by be inherited or it may be triggered by radiation, medication, chemotherapy, or infection.
- Thalassemia is an inherited condition typically occurring in individuals from the Middle East, the Mediterranean, Africa, and Southeast Asia, in which maturation of the RBCs does not proceed normally. The most severe form is called Cooley’s anemia (Betts et al., 2013).
Polycythemia
Polycythemia is an elevated RBC count and is detected in a patient’s elevated hematocrit percentage in a complete blood cell testing. It can occur transiently in a person who is dehydrated; when water intake is inadequate or water losses are excessive, the plasma volume falls. As a result, the hematocrit rises. A mild form of polycythemia is chronic but normal in people living at high altitudes. Some elite athletes train at high elevations specifically to induce this phenomenon. Finally, a type of bone marrow disease called polycythemia vera causes an excessive production of immature erythrocytes. Polycythemia vera can dangerously elevate the viscosity of blood, raising blood pressure and making it more difficult for the heart to pump blood throughout the body. It is a relatively rare disease that occurs more often in men than women, and is more likely to be present in elderly patients those over 60 years of age (Betts et al., 2013).
Platelet Disorders/Clotting Disorders
Thrombocytosis
Thrombocytosis is a condition in which there are too many platelets. This may trigger thrombosis, a potentially fatal disorder. A thrombus (plural = thrombi) is an aggregation of platelets, erythrocytes, and even WBCs typically trapped within a mass of fibrin strands. While the formation of a clot is a normal step in hemostasis, thrombi can form within an intact or only slightly damaged blood vessel, adhering to the vessel wall and decreasing or obstructing the flow of blood (Betts et al., 2013).
Thrombophilia
Thrombophilia, also called hypercoagulation, is a condition in which there is a tendency to form thrombosis. This may be an inherited disorder or may be caused by other conditions including lupus, immune reactions to heparin, polycythemia vera, thrombocytosis, sickle cell disease, pregnancy, and even obesity.
When a portion of a thrombus breaks free from the vessel wall and enters the circulation, it is referred to as an embolus. An embolus that is carried through the bloodstream can be large enough to block a vessel critical to a major organ. When it becomes trapped, an embolus is called an embolism. In the heart, brain, or lungs, an embolism may accordingly cause a heart attack, a stroke, or a pulmonary embolism (Betts et al., 2013).
Thrombocytopenia
Thrombocytopenia is a condition in which there is an insufficient number of platelets, possibly leading to ineffective blood clotting and excessive bleeding (Betts et al., 2013).
Hemophilia
Hemophilia is a group of related genetic disorders in which certain plasma clotting factors are lacking, inadequate or nonfunctional. Patients with hemophilia bleed from even minor internal and external wounds and leak blood into joint spaces after exercise and into urine and stool. Regular infusions of clotting factors isolated from healthy donors can help prevent bleeding in hemophiliac patients. At some point, genetic therapy will become a viable option (Betts et al., 2013).
Leukocyte Disorders
Leukopenia
Leukopenia is a condition in which too few leukocytes are produced. If this condition is pronounced, the individual may be unable to ward off disease (Betts et al., 2013).
Leukocytosis
Leukocytosis is excessive leukocyte proliferation. Although leukocyte counts are high, the cells themselves are often nonfunctional, leaving the individual at increased risk for disease (Betts et al., 2013).
Leukemia
Leukemia is a cancer involving an abundance of leukocytes. It may involve only one specific type of leukocyte from either the myeloid line (myelocytic leukemia) or the lymphoid line (lymphocytic leukemia). In chronic leukemia, mature leukocytes accumulate and fail to die. In acute leukemia, there is an overproduction of young, immature leukocytes. In both conditions, the cells do not function properly (Betts et al., 2013).
Lymphoma
Lymphoma is a form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. As in leukemia, the malignant leukocytes do not function properly, and the patient is vulnerable to infection. Some forms of lymphoma tend to progress slowly and respond well to treatment. Others tend to progress quickly and require aggressive treatment, without which they are rapidly fatal (Betts et al., 2013).
Other Conditions Related to Abnormal Leukocyte Counts
| Cell Type |
Conditions Reltaed to High Counts | Conditions Related to Low Counts |
|---|---|---|
| Neutrophil | Infection, inflammation, burns, unusual stress | Drug toxicity, other disorders |
| Eosinophil | Allergies, parasitic worm infestations, some autoimmune diseases | Drug toxicity, stress |
| Basophil | Allergies, parasitic infections, hypothyroidism | Pregnancy, stress, hyperthyroidism |
| Lymphocyte | Viral infections, some cancers | chronic illness, immunosuppression (due to HIV or steroid therapy) |
| Monocyte | Viral or fungal infections, tuberculosis, some forms of leukemia, other chronic diseases | Bone marrow suppression |
Bone Marrow Biopsy/Bone Marrow Transplant
Sometimes, a healthcare provider will order a bone marrow biopsy, a diagnostic test of a sample of red bone marrow, or a bone marrow transplant, a treatment in which a donor’s healthy bone marrow—and its stem cells—replaces the faulty bone marrow of a patient. These tests and procedures are often used to assist in the diagnosis and treatment of various severe forms of anemia, such as thalassemia major and sickle cell anemia, as well as some types of cancer, specifically leukemia.
In the past, bone marrow sampling or transplant was very painful, as the procedure involved inserting a large-bore needle into the region near the iliac crest of the pelvic bones. Now, direct sampling of bone marrow can often be avoided as stem cells can be isolated in just a few hours from a sample of a patient’s blood. The isolated stem cells are then grown in culture using the appropriate hemopoietic growth factors, and analyzed or sometimes frozen for later use.
For an individual requiring a transplant, a matching donor is essential to prevent the immune system from destroying the donor cells—a phenomenon known as tissue rejection. To treat patients with bone marrow transplants, it is first necessary to destroy the patient’s own diseased marrow through radiation and/or chemotherapy. Donor bone marrow stem cells are then infused into the recipient’s bloodstream, so that they can establish themselves in the recipient’s bone marrow (Betts et al., 2013).
Check Your Knowledge of Cardiovascular System Terms and Abbreviations
Common Cardiovascular System – Blood, Abbreviations
Many terms and phrases related to the cardiovascular system – blood are abbreviated. Learn these common abbreviations by expanding the list below.
Cardiovascular System – Blood Abbreviations
- aPTT (activated partial thromboplastin time
- CBC and Diff (complete blood count and differential)
- CPK (creatine phosphokinase)
- Hct (hematocrit)
- Hgb (hemoglobin)
- PT (prothrombin time)
- RBC (red blood cell, erythrocyte)
- WBC (white blood cell, leukocyte)
Activity source: Cardiovascular System – Blood Abbreviations by Kimberlee Carter, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. / Converted to text.
Cardiovascular System – Consultation Report
Cardiovascular System – Consultation Report (Text version)
Fill in the consultation report with using the following words:
- Angiogram
- defect
- palpitations
- infection
- blood pressure
- coronary
PATIENT NAME: Jack MIRANDA
AGE: 74
SEX: Male
DATE OF CONSULTATION: March 26, 2020
CONSULTING PHYSICIAN: Kevin Palmer, MD, Cardiology
REASON FOR CONSULTATION: Coronary artery disease.
PAST MEDICAL HISTORY
- Coronary artery disease. He had an NST MI in July 2015. _________[Blank 1] showed three-vessel disease and had PCT of RCA OM1. LAD had 60% stenosis which was no significant by FFR and medical management was recommended. He had a Grade 2 left ventricular function after the MI, but it improved a year later. His last echocardiogram in 2019 showed preserved ejection fraction at 60 with no significant valvular abnormalities and no significant wall motion abnormalities. He had an exercise Myoview in 2018 where he could achieve a workload of 9 Mets without symptoms or electrical changes. Perfusion images showed a wall fixed inferior _________[Blank 2] in keeping with his
previous inferior MI. - Hypertension.
- Hypercholesterolemia.
- Ex-smoker quit in 2016.
- Rare alcohol.
- Gout.
- Chronic lymphocytic leukemia.
MEDICATIONS
Aspirin 81 mg q.d.
Bisoprolol 5 mg q.d.
Candesartan 60 mg q.d.
Atorvastatin 80 mg q.d.
Ezetrol 10 mg q.d.
Allopurinol 300 mg q.d.
HISTORY: Overall, he has been feeling well. He denies any exertional symptoms with usual activity. He walks his dog 20 minutes a day and denies any chest pain, shortness of breath. He denies orthopnea, _____________[Blank 3], dizziness presyncope, or syncope.
He was recently hospitalized with a respiratory ___________[Blank 4]. He was treated with antibiotics and was discharged 2 days later. He has been feeling better and has gone back to his usual activities.
In regards to his CLL, he has been stable with usual lymphocyte count around 30. No other cytopenia. No splenomegaly. He is being followed with a surveillance strategy with regular CBCs by hematologist.
PHYSICAL EXAMINATION: On physical exam he is alert and oriented in no acute distress, hemodynamically stable, __________[Blank 5] 120/70, heart rate 60 with regular rhythm, there is no evidence of volume overload, lungs are clear. Lab work showed white cell count of 30 with lymphocytes, 25 hemoglobin, 122 platelets, 340 creatinine, 70 EGFR, 75 sodium, 144 potassium, 5.6, A1c 5.4L, DL 1.2.
SUMMARY: Mr. Miranda seems to be stable from the cardiac point of view. He has a history of ________________[Blank 6] artery disease with previous MI treated with PCI of RCA and OM1. He has a residual 60% stenosis of LAD that was not significant by FFR. He is on antiplatelet agents, high intensity statin therapy, and the combination of ARB’s and beta-blockers. As long as his functional capacity remains stable, we do not need to do a follow up. Exercise treadmill test but should his symptoms change, this should be considered.
PLAN: His blood pressure is well controlled. His LDL is within the goal. There is no history of diabetes. He quit smoking 2016. I made no changed to his current treatment plan and advised him to come back in a year’s time and earlier, should symptoms change.
__________________________
Kevin Palmer, MD, Cardiology
Check your answers: [1]
Activity source: Neurological System – History and Physical Examination by Sheila Bellefeuille & Heather Scudder, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. / Text version added.
Medical Specialties and Procedures Related to the Blood Vessels and Blood
Vascular Surgeons
Vascular surgery is a specialty in which the physician treats diseases of the blood and lymphatic vessels. This includes repair and replacement of diseased or damaged vessels, removal of plaque from vessels, minimally invasive procedures, including the insertion of venous catheters, and traditional surgery (Betts et al., 2013; Canadian Society for Vascular Surgery, n.d.). For more information, please visit the Canadian Society for Vascular Surgery website [New Tab].
Hematologists
Hematologists are specialist physicians that diagnose and treat blood disorders. These physicians must be well-versed in a wide array of laboratory procedures, basic medical disciplines, and clinical medicine (Canadian Medical Association, 2019). To learn more about hematologists, visit the Canadian Medical Association’s specialty profile on hematology [PDF].
Diagnostic Vascular Technologist
Also known as Canadian Registered Vascular Sonographers (CRVS®), these specialists are technologists that image the vascular system (Sonography Canada, 2021). To learn more, visit the Sonography Canada Credentials web page [New Tab].
Phlebotomist
Phlebotomists are professionals trained to draw blood (phleb- = “a blood vessel”; -tomy = “to cut”). When more than a few drops of blood are required, phlebotomists perform a venipuncture, typically of a surface vein in the arm. They perform a capillary stick on a finger, an earlobe, or the heel of an infant when only a small quantity of blood is required. An arterial stick is collected from an artery and used to analyze blood gases. After collection, the blood may be analyzed by medical laboratories or perhaps used for transfusions, donations, or research (Betts et al., 2013).
Image Descriptions
Figure 10.16 image description: The left panel (a) shows the cross-section of a normal and a narrowed artery. A normal artery has no plaque along the artery walls which means there is normal blood flow. In a narrow artery, plague forms on the arterial walls causing abnormal blood flow. The right panel (b) shows a micrograph of an artery with plaque in it. [Return to Figure 10.16].
Figure 10.18 image description: This photograph shows red blood cells of a person suffering from sickle cell anemia. Instead of being discoid shaped like healthy blood cells, sickle red blood cells are shaped like a sickle. [Return to Figure 10.18].
Attribution
Except where otherwise noted, this chapter is adapted from “Cardiovascular System – Blood Vessels and Blood” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Cardiovascular System – Blood Vessels and Blood chapter content into sub-chapters.
- 1) Angiogram 2) defect 3) palpitations 4) infection 5) blood pressure 6) coronary ↵
hardening of arteries
Compliance is the ability of any compartment to expand to accommodate increased content. The greater the compliance of an artery, the more effectively it is able to expand to accommodate surges in blood flow without increased resistance or blood pressure.
a hardening of the arteries that involves the accumulation of plaque
a fatty material including cholesterol, connective tissue, white blood cells, and some smooth muscle cells
High blood pressure
also called coronary artery disease (CAD); the blood vessels that supply blood to the myocardium become hardened and narrowed, impairing the delivery of oxygen to the heart muscle
a freely moving piece of a substance (plaque or blood clot) that travels through the circulation until it blocks a smaller blood vessel, cutting of the supply of oxygen to the tissue
a balloon-tip catheter is fed through a blood vessel up to the site of the narrowing, the balloon is inflated to re-open the artery. A stent is sometimes placed at the site to reinforce the arterial wall and to prevent re-occlusion.
In a coronary bypass procedure, a non-vital superficial vessel from another part of the body (often the great saphenous vein) or a synthetic vessel is inserted to create a path around the blocked area of a coronary artery.
large artery in the neck
swelling
a disease or disorder that often lacks signs or symptoms
Weakening of the wall of a blood vessel, causing it to thin and balloon out, and possibly eventually burst, resulting in internal bleeding
obstruction of vessels in peripheral regions of the body
the process by which the body seals a ruptured blood vessel to prevent further blood loss
hypo=below, lower than normal, volemic=pertaining to volume (in this case, the volume of blood in the body)
Cardio=pertaining to the heart
genic=originating from, created by
Cardiogenic means originating from the heart
A piece of a blood clot or other substance has broken free from its original location and traveled through the bloodstream to lodge in a smaller vessel in the lungs. This causes an obstruction in that vessel and hypoxia to the tissues supplied by that vessel.
The pericardial sac surrounding the heart has filled with blood or other fluid and the resulting pressure is preventing the heart from beating effectively
An excessive amount of air is present in the thoracic cavity, outside of the lungs, putting pressure on the lungs and interfering with venous return, pulmonary function, and delivery of oxygen to the tissues
Erythropoietin is a hormone produced by the kidneys that plays an important role in the homeostasis of red blood cells levels in the body
Underactive thyroid gland, insufficient production of thyroid hormones (T3 and T4)
An autoimmune disease in which the body mounts an immune response against its own tissues, causing chronic inflammation and tissue damage
An autoimmune disorder in which the body mounts an immune response against its own joint tissues, causing inflammation and damage to the joints
A type of inflammatory bowel disease
Acquired immunodeficiency syndrome, caused by infection with the HIV virus
A lab test which measures the percentage red blood cells in a sample of whole blood. It represents how much of the person's blood is made up of red blood cells, by volume.
Viscosity is the thickness of fluids that affects their ability to flow
formation of unwanted blood clots
A type of bone marrow disease that causes an excessive production of immature erythrocytes
A condition in which there are too many platelets
Also called sickle cell anemia: A genetic disorder involving the production of an abnormal type of hemoglobin which delivers less oxygen to tissues and causes erythrocytes to assume a sickle (or crescent) shape
An inherited condition typically occurring in individuals from the Middle East, the Mediterranean, African, and Southeast Asia, in which maturation of the RBCs does not proceed normally. The most severe form is called Cooley’s anemia.
Chemical messengers which promote the proliferation and differentiation of formed elements and include erythropoietin, thrombopoietin, colony-stimulating factors, and interleukins.
Also called organ rejection. The recipient's immune system recognizes the transplanted tissue, the graft, as non-self and mounts an immune response against it, ultimately destroying it.

