5.2 – Anatomy (Structures) of the Urinary System
Kidney(s)
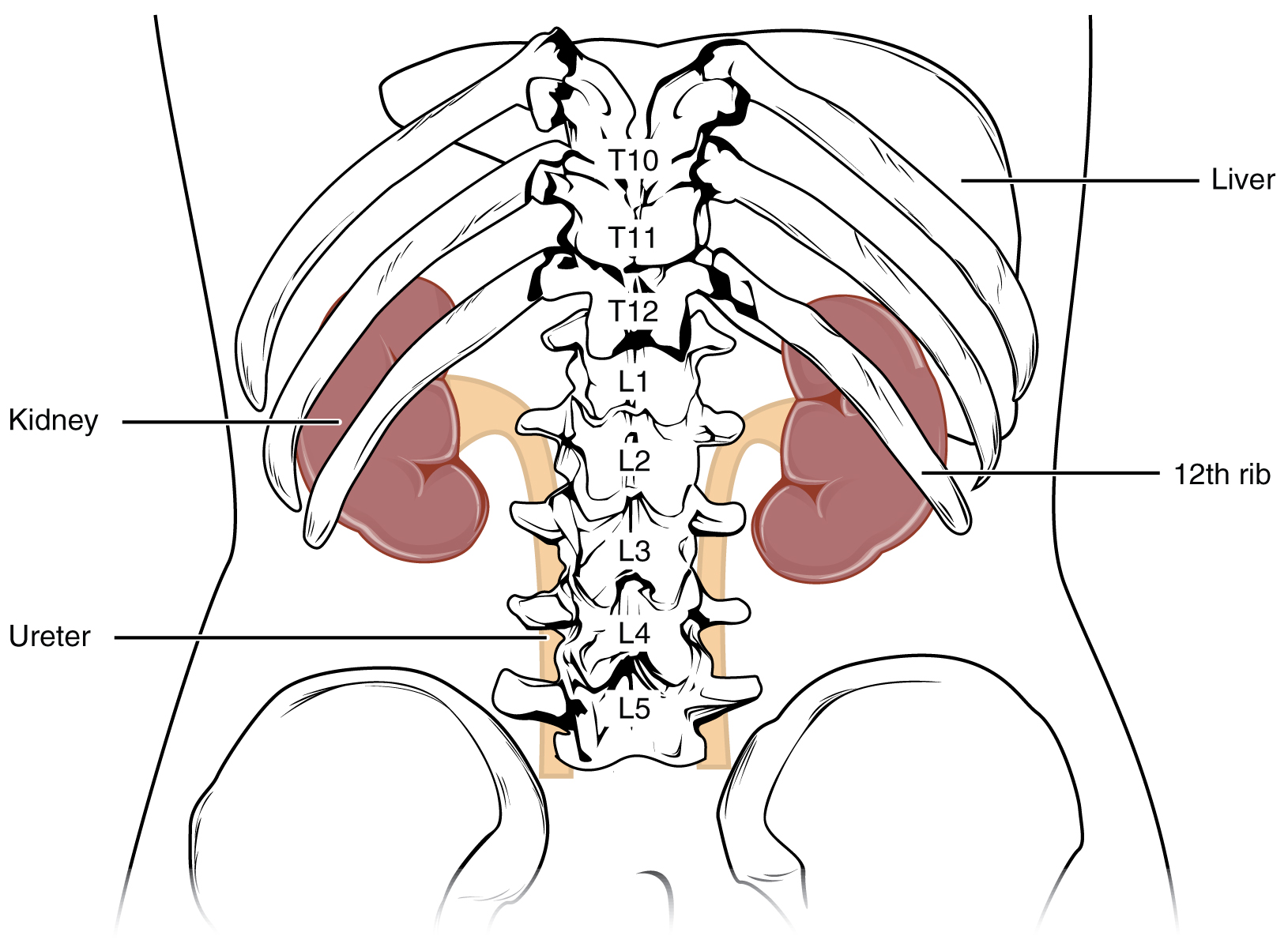
The kidneys lie on either side of the spine in the retroperitoneal space between the parietal peritoneum and the posterior abdominal wall, well protected by muscle, fat, and ribs. They are roughly the size of your fist. The male kidney is typically a bit larger than the female kidney. The kidneys are well vascularized, receiving about twenty-five percent of the cardiac output at rest. Figure 5.1 displays the location of the kidneys.
Did You Know?
Kidneys’ Internal Structure
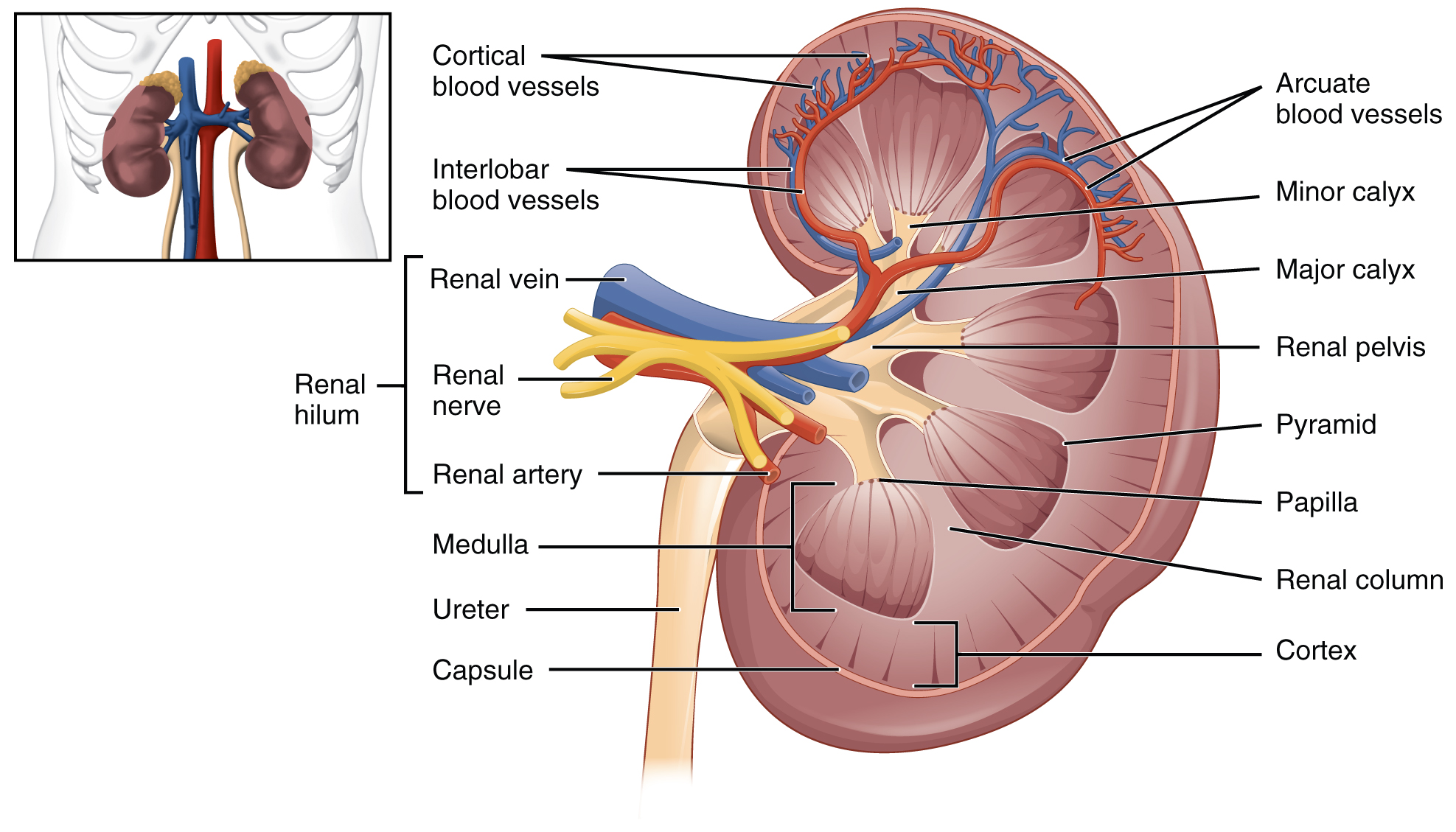
A frontal section through the kidney reveals an outer region called the renal cortex and an inner region called the medulla (see Figure 5.2). The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae. The papillae are bundles of collecting ducts that transport urine made by nephrons to the calyces of the kidney for excretion. The renal columns also serve to divide the kidney into 6–8 lobes and provide a supportive framework for vessels that enter and exit the cortex. The pyramids and renal columns taken together constitute the kidney lobes.
Renal Hilum
The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters. The medial-facing hila are tucked into the sweeping convex outline of the cortex. Emerging from the hilum is the renal pelvis, which is formed from the major and minor calyxes in the kidney. The smooth muscle in the renal pelvis funnels urine via peristalsis into the ureter. The renal arteries form directly from the descending aorta, whereas the renal veins return cleansed blood directly to the inferior vena cava. The artery, vein, and renal pelvis are arranged in an anterior-to-posterior order.
Nephrons and Vessels
The renal artery first divides into segmental arteries, followed by further branching to form interlobar arteries that pass through the renal columns to reach the cortex (see Figure 5.3). The interlobar arteries branch into arcuate arteries, cortical radiate arteries, and then into afferent arterioles. The afferent arterioles service about 1.3 million nephrons in each kidney.
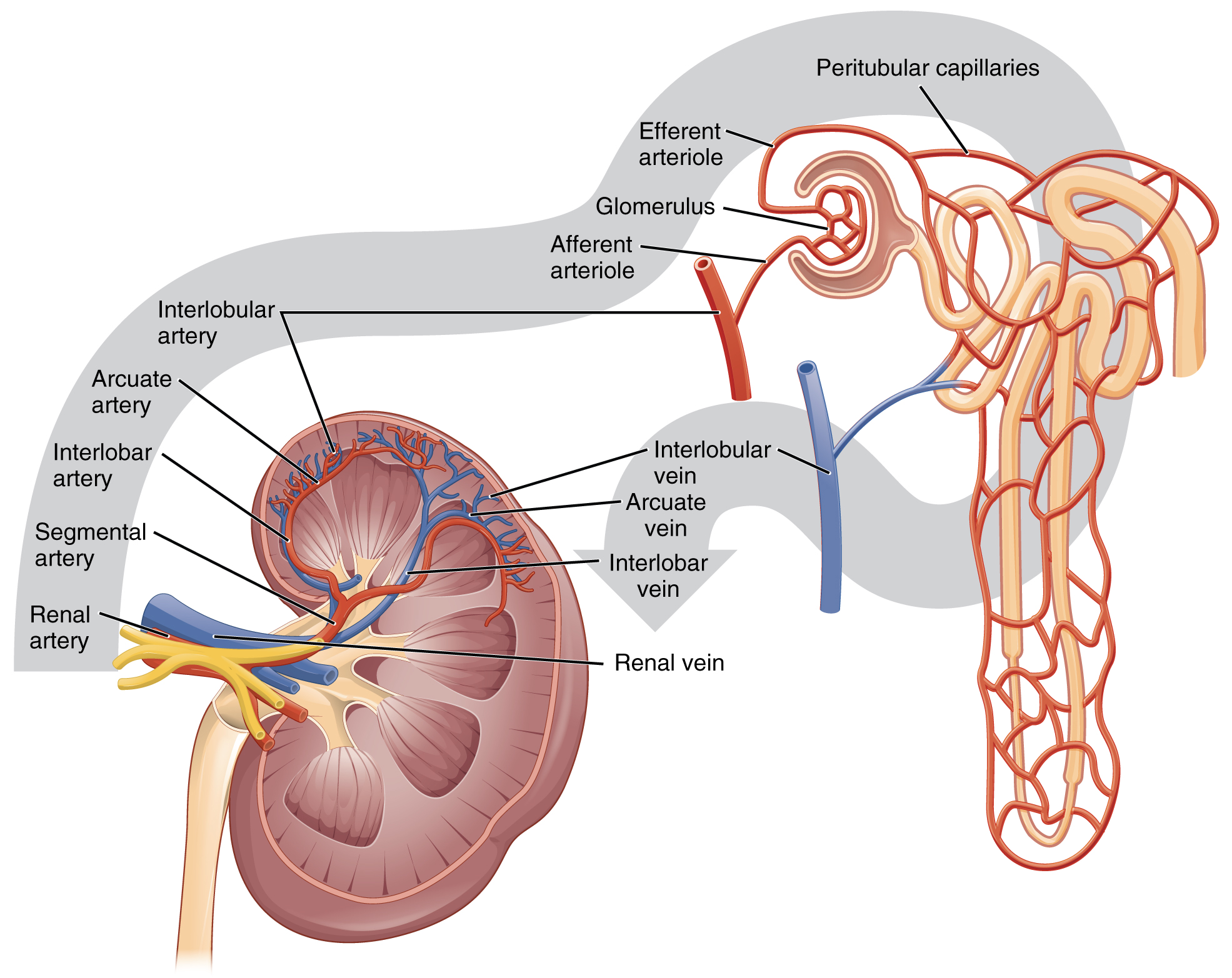
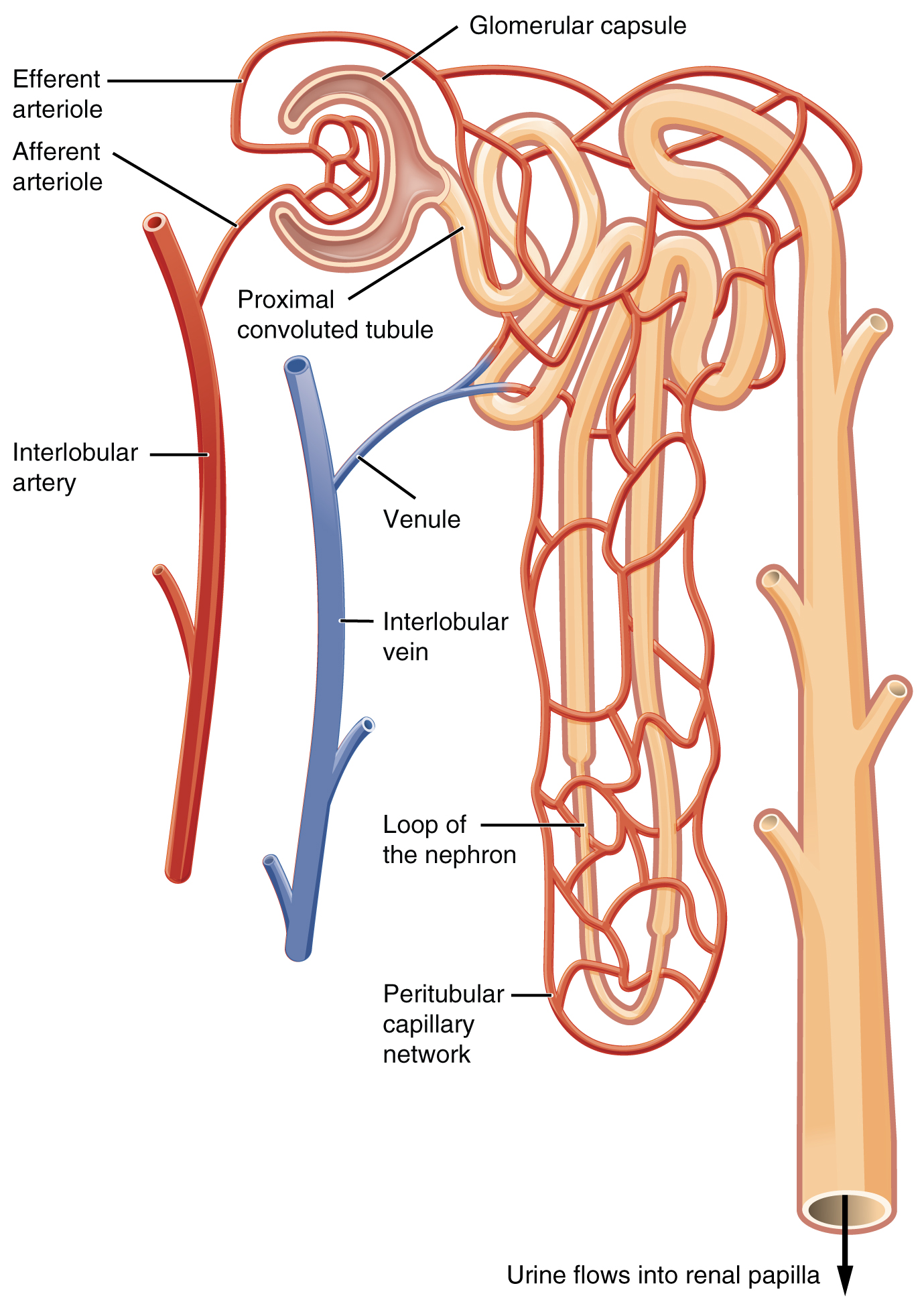
Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation. The afferent arterioles form a tuft of high-pressure capillaries about 200 µm in diameter, the glomerulus. The rest of the nephron consists of a continuous sophisticated tubule whose proximal end surrounds the glomerulus—this is Bowman’s capsule. Together, the glomerulus and Bowman’s capsule form the renal corpuscle. As mentioned earlier, these glomerular capillaries filter the blood based on particle size. After passing through the renal corpuscle, the capillaries form a second arteriole, the efferent arteriole (see Figure 5.4). These will next form a capillary network around the more distal portions of the nephron tubule, the peritubular capillaries and vasa recta, before returning to the venous system. As the glomerular filtrate progresses through the nephron, these capillary networks recover most of the solutes and water, and return them to the circulation. Since a capillary bed (the glomerulus) drains into a vessel that in turn forms a second capillary bed, the definition of a portal system is met. This is the only portal system in which an arteriole is found between the first and second capillary beds. Portal systems also link the hypothalamus to the anterior pituitary, and the blood vessels of the digestive viscera to the liver.
Ureter(s)
The kidneys and ureters are completely retroperitoneal, and the bladder has a peritoneal covering only over the dome. As urine is formed, it drains into the calyces of the kidney, which merge to form the funnel-shaped renal pelvis in the hilum of each kidney. The hilum narrows to become the ureter of each kidney. As urine passes through the ureter, it does not passively drain into the bladder but rather is propelled by waves of peristalsis. The ureters are approximately 30 cm long. The inner mucosa is lined with transitional epithelium and scattered goblet cells that secrete protective mucus. The muscular layer of the ureter consists of longitudinal and circular smooth muscles that create the peristaltic contractions to move the urine into the bladder without the aid of gravity. Finally, a loose adventitial layer composed of collagen and fat anchors the ureters between the parietal peritoneum and the posterior abdominal wall.
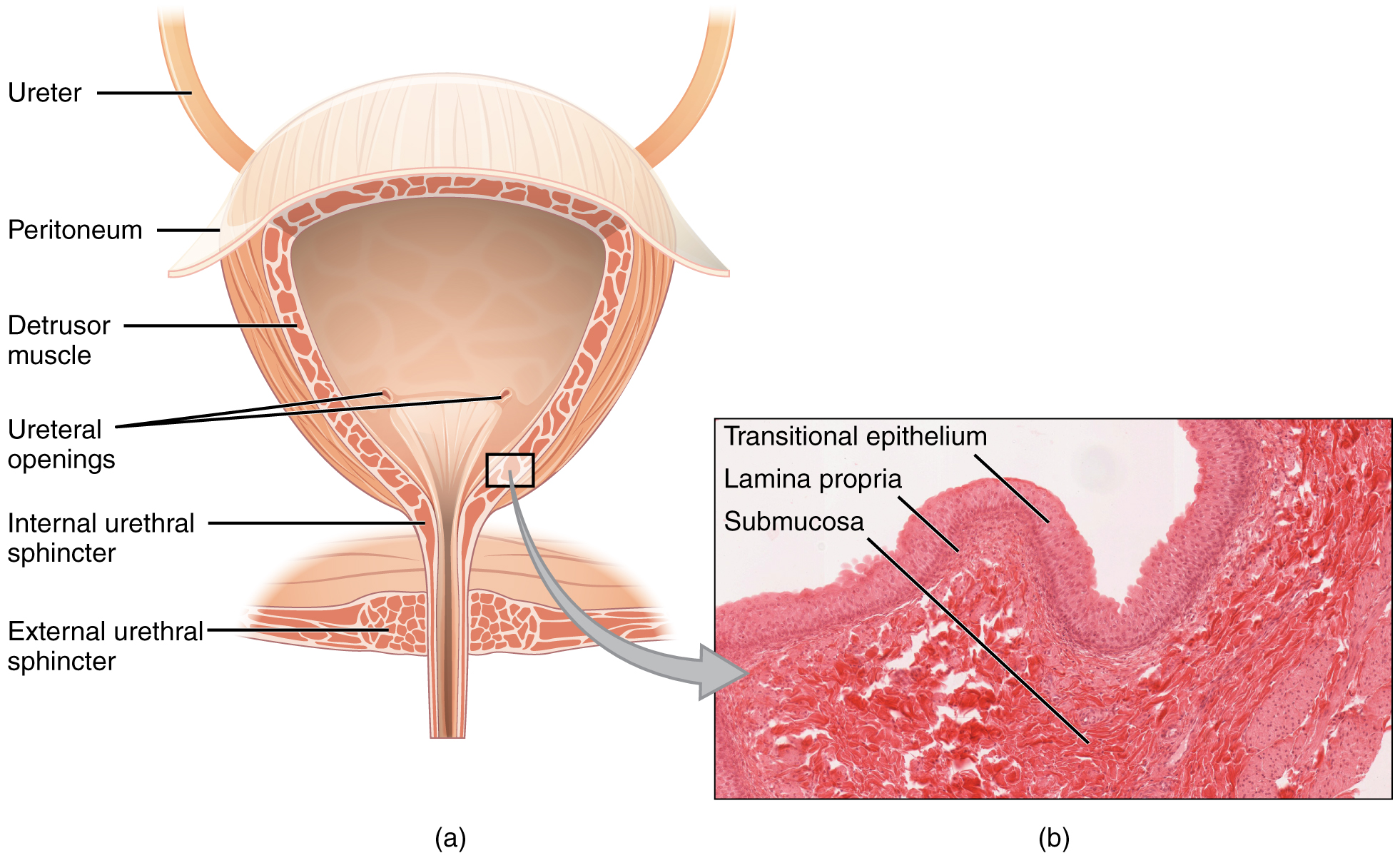
Bladder
The urinary bladder collects urine from both ureters ( see Figure 5.5). The bladder lies anterior to the uterus in females, posterior to the pubic bone and anterior to the rectum. During late pregnancy, its capacity is reduced due to compression by the enlarging uterus, resulting in increased frequency of urination. In males, the anatomy is similar, minus the uterus, and with the addition of the prostate inferior to the bladder. The bladder is partially retroperitoneal (outside the peritoneal cavity) with its peritoneal-covered “dome” projecting into the abdomen when the bladder is distended with urine.
Urethra
The urethra transports urine from the bladder to the outside of the body for disposal. The urethra is the only urologic organ that shows any significant anatomic difference between males and females; all other urine transport structures are identical (see Figure 5.6).
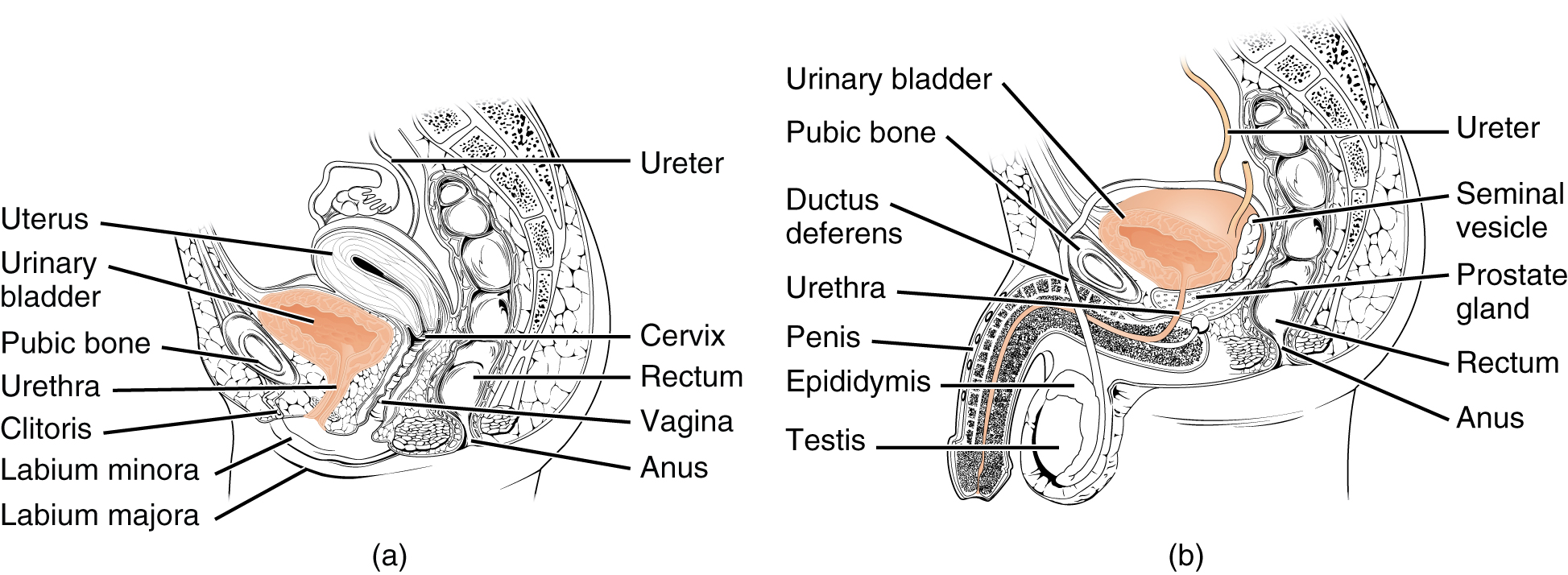
The urethra in both males and females begins inferior and central to the two ureteral openings forming the three points of a triangular-shaped area at the base of the bladder called the trigone (Greek tri- = “triangle” and the root of the word “trigonometry”). The urethra tracks posterior and inferior to the pubic symphysis (see Figure 5.6). In both males and females, the proximal urethra is lined by transitional epithelium, whereas the terminal portion is a nonkeratinized, stratified squamous epithelium. In the male, pseudostratified columnar epithelium lines the urethra between these two cell types. Voiding is regulated by an involuntary autonomic nervous system-controlled internal urinary sphincter, consisting of smooth muscle and voluntary skeletal muscle that forms the external urinary sphincter below it.
Micturition Reflex
Micturition is a less-often used, but proper term for urination or voiding. It results from an interplay of involuntary and voluntary actions by the internal and external urethral sphincters. When bladder volume reaches about 150 mL, an urge to void is sensed but is easily overridden. Voluntary control of urination relies on consciously preventing relaxation of the external urethral sphincter to maintain urinary continence. As the bladder fills, subsequent urges become harder to ignore. Ultimately, voluntary constraint fails with resulting incontinence, which will occur as bladder volume approaches 300 to 400 ml.
- Normal micturition is a result of stretch receptors in the bladder wall that transmit nerve impulses to the sacral region of the spinal cord to generate a spinal reflex. The resulting parasympathetic neural outflow causes contraction of the detrusor muscle and relaxation of the involuntary internal urethral sphincter.
- At the same time, the spinal cord inhibits somatic motor neurons, resulting in the relaxation of the skeletal muscle of the external urethral sphincter.
- The micturition reflex is active in infants but with maturity, children learn to override the reflex by asserting external sphincter control, thereby delaying voiding (potty training). This reflex may be preserved even in the face of spinal cord injury that results in paraplegia or quadriplegia. However, relaxation of the external sphincter may not be possible in all cases, and therefore, periodic catheterization may be necessary for bladder emptying.
Nerves involved in the control of urination include the hypogastric, pelvic, and pudendal. Voluntary micturition requires an intact spinal cord and functional pudendal nerve arising from the sacral micturition center. Since the external urinary sphincter is voluntary skeletal muscle, actions by cholinergic neurons maintain contraction (and thereby continence) during filling of the bladder. At the same time, sympathetic nervous activity via the hypogastric nerves suppresses contraction of the detrusor muscle. With further bladder stretch, afferent signals traveling over sacral pelvic nerves activate parasympathetic neurons. This activates efferent neurons to release acetylcholine at the neuromuscular junctions, producing detrusor contraction and bladder emptying.
Did You Know?
Check Your Knowledge of Urinary Systems
Concept Check
- Describe two organs or structures essential to the urinary system.
- Identify the structure within the kidneys which filters blood.
- Name a commonly used term for the micturition reflex.
Anatomy Labeling Activity
Urinary System Bladder Anatomy (Text Version)
Label the diagram correctly with the following words:
- Peritoneum
- Detrusor muscle
- External urethral sphincter
- Ureter
- Internal urethral sphincter
- Ureteral opening
Urinary System Bladder Anatomy Diagram (Text Version)
This figure shows the cross section of the bladder, and the major parts are identified from top to bottom. The tube leading to the bladder is known as the ________[Blank 1]. Surrounding the bladder is a membranous cover called the ________[Blank 2]. The walls of the bladder are formed by _________[Blank 3], which allows the bladder to contract to excrete urine or relax to hold urine The right panel shows a micrograph of the bladder. The _________[Blank 4] are found inside the bladder wall allowing for the ureters to enter and deposit urine formed from the kidneys. In the lower portion of the bladder is two sphincter muscles the internal one is the __________[Blank 5] and the __________[Blank 6]. These sphincter muscles open and close controlling the flow of urine out of the bladder and into the urethra to be carried to the outside of the body.
Check your answers: [1]
Activity source: Urinary System Bladder Anatomy by Kimberlee Carter, from Building a Medical Terminology Foundation, illustration from Anatomy and Physiology (OpenStax), licensed under CC BY 4.0./ Text version added.
Image Descriptions
Figure 5.1 image description: This illustration shows an anterior view of the abdominal area. The liver is prominently positioned in the upper right quadrant, partially overlapping the right kidney. The 12th rib is visible, arching above the upper portion of the kidneys. The ureters are shown descending from the kidneys, running vertically down towards the bladder [Return to image 5.1]
Figure 5.2 image description: This illustration shows a frontal section through a kidney. Working clockwise from the top of the image is the arcuate blood vessels. The minor and major calyx is shown followed by the renal pelvis, pyramid, and papilla. The renal column is connective tissue radiating downward towards the renal cortex. The capsule is a tough outer layer surrounding the kidney. The ureter extends from the kidney towards the bladder. The medulla is the inner component of the kidney. The hilum is a small opening structure, allowing for the renal artery, renal nerve and renal artery to enter and exit the kidney. Above the renal vein is the interlobar blood vessels followed by the cortical blood vessels [Return to Figure 5.2].
Figure 5.3 image description: The illustration is an anatomical view of the human kidney and its blood supply system. Displayed is the internal structure of the kidney, including the renal artery, interlobar artery, arcuate artery, interlobular artery, and afferent arterioles leading to the glomerulus. The glomerulus is connected to efferent arterioles, which lead to peritubular capillaries. The illustration also depicts the flow of blood from these vessels into the renal vein.[Return to Figure 5.3].
Attribution
Except where otherwise noted, this chapter is adapted from “Urinary System” In Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Urinary System chapter content into sub-chapters.
-
↵
Check your Answer: Urinary System Bladder Anatomy Diagram (Text Version)
This figure shows the cross section of the bladder, and the major parts are identified from top to bottom. The tube leading to the bladder is known as the ureter. Surrounding the bladder is a membranous cover called the peritoneum. The walls of the bladder are formed by detrusor muscle, which allows the bladder to contract to excrete urine or relax to hold urine The right panel shows a micrograph of the bladder. The ureteral openings are found inside the bladder wall allowing for the ureters to enter and deposit urine formed from the kidneys. In the lower portion of the bladder is two sphincter muscles the internal one is the internal urethral sphincter and the external urethral sphincter. These sphincter muscles open and close controlling the flow of urine out of the bladder and into the urethra to be carried to the outside of the body.
An inner region of specific structure such as the kidneys
Renal pyramids are kidney tissues that are shaped like cones.
The apex of the renal pyramid
Waste is eliminated from an organism. In vertebrates this is primarily carried out by the lungs, kidneys and skin.
a cuplike cavity or structure
The outermost layer of the wall of a blood vessel
Consisting of closely packed cells which appear to be arranged in layers.
Excrete (waste matter)
unconsciously regulates
A muscle which forms a layer of the wall of the bladder

