11.4 – Lymphatic Diseases, Disorders and Diagnostic Testing
The immune response can be under-reactive or over-reactive, leading to a state of disease. The factors that maintain immunological homeostasis are complex and incompletely understood.
Underactive Immune System: Immunodeficiencies
Suppressed immunity can result from inherited genetic defects or by acquiring viruses (Betts et al., 2013).
Inherited Immunodeficiencies/SCID
While many inherited immunodeficiencies exist, the most serious is severe combined immunodeficiency disease (SCID). This complex disease is caused by many different genetic defects which result in impaired B cell and T cell arms of the adaptive immune response. Children with this disease usually die of opportunistic infections within their first year of life unless they receive a bone marrow transplant. Such a procedure had not yet been perfected for David Vetter, the “boy in the bubble,” who was treated for SCID by having to live in a sterile plastic cocoon for the 12 years before his death from infection in 1984. One of the features that make bone marrow transplants work as well as they do is the proliferative capability of hematopoietic stem cells of the bone marrow. Only a small amount of bone marrow from a healthy donor is given intravenously to the recipient. It finds its own way to the bone where it populates it, eventually reconstituting the patient’s immune system, which is usually destroyed beforehand by treatment with radiation or chemotherapeutic drugs (Betts et al., 2013).
New treatments for SCID using gene therapy (inserting nondefective genes into cells taken from the patient and giving them back) have the advantage of not needing the tissue match required for standard transplants. Although not a standard treatment, this approach holds promise, especially for those in whom standard bone marrow transplantation has failed (Betts et al., 2013).
Acquired Immunodeficiency/HIV and AIDS
Although many viruses cause suppression of the immune system, only HIV wipes it out completely. HIV is transmitted through semen, vaginal fluids, and blood, and can be caught by risky sexual behaviors and the sharing of needles by intravenous drug users. There are sometimes, but not always, flu-like symptoms in the first 1 to 2 weeks after infection. The presence of anti-HIV antibodies indicates a positive HIV test. Because seroconversion takes different lengths of time in different individuals, multiple HIV tests are given months apart to confirm or eliminate the possibility of infection.
After seroconversion, the amount of virus circulating in the blood drops and stays at a low level for several years. During this time, the levels of CD4 T cells decline steadily, until at some point, the immune response is so weak that opportunistic disease and eventually death result.
Treatment for the disease consists of drugs that target virally encoded proteins that are necessary for viral replication but are absent from normal human cells. By targeting the virus itself and sparing the cells, this approach has been successful in significantly prolonging the lives of HIV-positive individuals (Betts et al., 2013).
Overactive Immune System: Hypersensitivities and Autoimmune Diseases
Hypersensitivities
Over-reactive immune responses include the hypersensitivities: allergies and inflammatory responses to nonpathogenic environmental substances (Betts et al., 2013). The table below compares different hypersensitivities.
| Type of Hypersensititivy | Details and Explanation |
|---|---|
| Type I |
|
| Type II |
|
| Type III |
|
| Type IV |
|
Autoimmune Responses
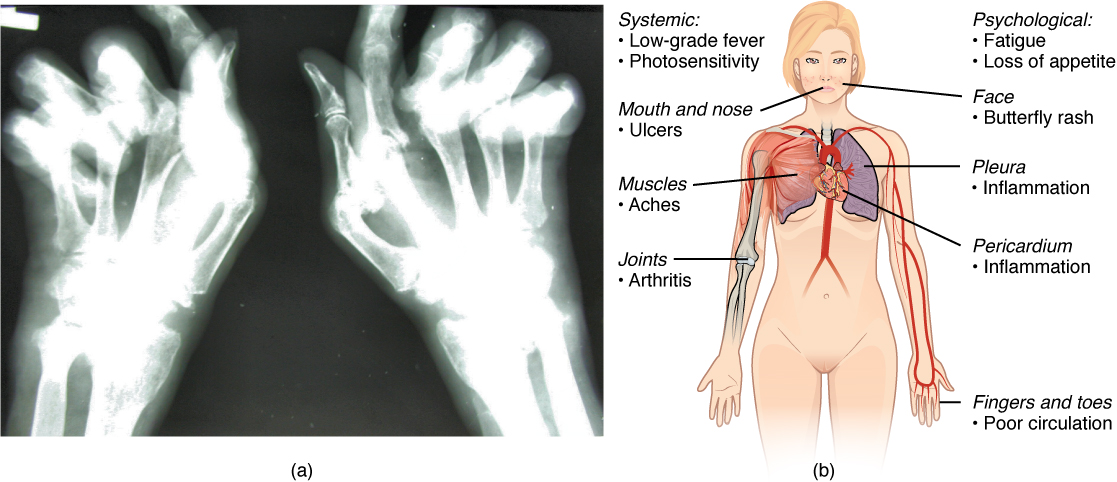
The worst cases of the immune system over-reacting are autoimmune diseases in which the immune systems begin to attack cells of the patient’s own body, causing chronic inflammation and significant damage. The trigger for these diseases is often unknown, although environmental and genetic factors are likely involved. Treatments are usually based on resolving the symptoms using immunosuppressive and anti-inflammatory drugs. Figure 11.15 below provides two examples of autoimmune diseases: rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE)(Betts et al., 2013).
Overall, there are more than 80 different autoimmune diseases, which are a significant health problem in the elderly. Table 11.5 below lists several of the most common autoimmune diseases, the antigens that are targeted (autoantigen or “self” antigen), and the resulting tissue damage (Betts et al., 2013).
| Disease | Autoantigen | Symptoms |
|---|---|---|
| Celiac disease | Tissue transglutaminase | Damage to small intestine |
| Diabetes mellitus type I | Beta cells of pancreas | Low insulin production; inability to regulate serum glucose |
| Graves’ disease | Thyroid-stimulating hormone receptor (antibody blocks receptor) | Hyperthyroidism |
| Hashimoto’s thyroiditis | Thyroid-stimulating hormone receptor (antibody mimics hormone and stimulates receptor) | Hypothyroidism |
| Lupus erythematosus | Nuclear DNA and proteins | Damage of many body systems |
| Myasthenia gravis | Acetylcholine receptor in neuromuscular junctions | Debilitating muscle weakness |
| Rheumatoid arthritis | Joint capsule antigens | Chronic inflammation of joints |
Lymphoma
Lymphoma was briefly discussed in the previous chapter.
Lymphatic Medical Terms in Use
Medical Terms in Context
Lymphatic System – Medical Report (Text version)
Fill in the following medical reporting using the words listed below:
- itchy
- runny
- allergies
- dander
- medications
- distress
- heart
- drainage
- Dyspnea
- rhinitis
- iron
PATIENT NAME: Sally WESSON
AGE: 43
SEX: Female
DOB: September 26
DATE OF ASSESSMENT: March 20
ATTENDING PHYSICIAN: Trevor Sharpe, MD
CHIEF COMPLAINT: Allergies.
HISTORY: A 43-year-old Asian female states being very tired and irritable. She had presented watery and __________[Blank 1] eyes, itchy throat, sneezing, ___________[Blank 2] and stuffy nose. She has family history of __________[Blank 3]. She always struggled with many different allergies: dust, pollen, cat and dog __________[Blank 4]. She had tried different types of over-the-counter allergy ___________[Blank 5], but they didn’t help to alleviate the symptoms. She is currently taking Reactine 5 mg daily which does not relieve all of her symptoms.
PHYSICAL EXAMINATION: GENERAL: Patient is pale and in moderate ________[Blank 6]. VITAL SIGNS: Weight 160 pounds, B/P 120/80, ________[Blank 7] rate 90 beats per minute, respiratory rate 18 per minute, temperature 98.6 F. HEENT: EYES: Red, watery, itching, burning and swelling. EARS: Normal. NOSE: Mouth breathing, sneezing, runny and itchy nose, post-nasal _________[Blank 8], nasal congestion. THROAT: Itchy and swollen. CHEST: __________[Blank 9] and wheezing.
MEDICATIONS
- Reactine 5 mg ________[Blank 10].
- Escitalopram 20 mg q.d.
- Lorazepam 0.5 mg p.r.n. nightly at bedtime.
- Fenofibrate 145 mg q.h.s.
ASSESSMENT
- Patient has severe seasonal allergic ___________[Blank 11].
- Possible anemia.
PLAN
- Recommended Reactive 10 mg q.d.
- Referred to an allergist to provide patient more options for allergy treatments.
- Ordered a blood work to check her ________[Blank 12] and cholesterol levels.
- Follow up in 4 days to review her blood work results.
_________________________________
Trevor Sharpe, MD
Check your answers:[1]
Activity source: “Lymphatic System – Medical Report” by Sheila Bellefeuille & Heather Scudder, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. /Text version added.
Lymphatic System – Medical Report
Lymphatic System – Medical Report (Text version)
Fill in the following medical report using the words listed below:
- stones
- fatigued
- fever
- tonsillitis
- temperature
- cervical
- dysphagia
- erythema
- crypts
- tonsillolith
- pseudomembranes
- tonsillectomy
- gargles
PATIENT NAME: Celine CAMERON
AGE: 16
SEX: Female
DOB: March 25
DATE OF ASSESSMENT: August 4
ATTENDING PHYSICIAN: Grant Talbot, MD, Pediatrics
HISTORY: This is a 16-year-old female today with complaints of throat pain. She has been struggling with inflamed tonsils for the last 2 weeks. The patient claims that tonsil ________[Blank 1] are forming and that a white film has appeared over their tonsils. She has been feeling very _________[Blank 2], has developed a mild ________[Blank 3] and occasionally feel nauseous.
The client has a family history of _________[Blank 4] resulting in tonsillectomy. She mentioned that her grandmother experienced recurrent tonsillitis around the same age. The condition of tonsillitis has occurred on 2 other occasions in the past 5 months.
PHYSICAL AND EXAMINATION: Ms. Cameron is in no acute distress. She appears fatigued. VITAL SIGNS: Blood Pressure 132/83, __________[Blank 5] is slightly elevated at 99.6, pulse 67. She is in generally in good condition. Throat palpation was performed. There is significant enlargement of the __________[Blank 6] lymph nodes. She appears to be experiencing ________[Blank 7]. Throat was examined and revealed swelling, ________[Blank 8] and tonsillar ________[Blank 9] visible. A ________[Blank 10] was seen to be forming within one of the crypts. Celine’s claims of ________[Blank 11] were also confirmed. She denies any symptoms such as a nasal discharge, cough, or abdominal pain. Throat was swabbed.
ASSESSMENT: Ms. Cameron appears to be experiencing recurrent tonsillitis correlated to exaggerated tonsillar crypts. Possible ___________[Blank 12] may be required.
PLAN
- Patient was given a referral to an ENT specialist and may require tonsillectomy.
- The patient was instructed to follow a diet of soft, smooth foods and soothing liquids.
- It was suggested that the patient use saltwater ________[Blank 13] in the mornings and before bed.
- A prescription of Amoxicillin 400 mg p.o. p.c.
___________________________________
Grant Talbot, MD, Pediatrics
Check your answers: [2]
Activity source: “Lymphatic System – Medical Report” by Sheila Bellefeuille and Healther Scudder, licensed under CC BY- 4.0 from “Lymphatic and Immune Systems” In Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. / Converted to Text.
Lymphatic System – Medical Report
Lymphatic System – Medical Report (Text version)
Fill in the following medical report using the words listed below:
- dysphagia
- prescribed
- lymph
- enlarged
- ibuprofen
- erythromycin
- tonsillectomy
- surgery
PATIENT NAME: Jason MACDONALD
AGE: 7
SEX: Male
DOB: August 19
DATE OF ASSESSMENT: November 15
ATTENDING PHYSICIAN: Grant Talbot, MD, Pediatrics
DIAGNOSIS: Tonsillitis
HISTORY: This 7-year-old white male has been seen by me on several occasions over the last two years. He has complained of pharyngitis, ________[Blank 1], and fever. I have ___________[Blank 2] erythromycin in the past.
PHYSICAL EXAMINATION: When I examined Jason today, he once again had the same complaints as in the past. I also noticed that the ________[Blank 3] nodes in his neck were __________[Blank 4] and tender. He had a temperature of 39 degrees.
TREATMENT: I gave Jason _________[Blank 5] for his fever and prescribed _________[Blank 6] again.
PLAN: It is my recommendation that Jason undergo a _________[Blank 7]. Jason’s parents are in agreement. I will make the arrangements for Jason’s ___________[Blank 8].
_________________________
Grant Talbot, MD, Pediatrics
Check your answers: [3]
Activity source: “Lymphatic System – Medical Report” by Heather Scudder, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. /Text version added.
Medical Specialties and Procedures Related to the Lymphatic and Immune Systems
Clinical Immunology/Allergy is a medical specialty that diagnoses and treats diseases of the immune system (Canadian Medical Association, 2019). For more information, please visit the Canadian Medical Association Specialty Profiles Clinical Immunology page [PDF].
Skin testing (for allergies) is done by a clinical immunologist/allergist to identify allergens in Type I hypersensitivity. In skin testing, allergen extracts are injected into the epidermis, and a positive result of the wheal and flare response usually occurs within 30 minutes. The soft center is due to fluid leaking from the blood vessels and the redness is caused by the increased blood flow to the area that results from the dilation of local blood vessels at the site (Betts et al., 2013).
Image Descriptions
Figure 11.15 image description: The left panel of this figure shows an x-ray image of a person’s hand with rheumatoid arthritis, and the right panel of this figure shows a woman’s body with labels showing the different responses in the body when the patient suffers from lupus. Labels (from top, clockwise) read: psychological: fatigue, loss of appetite, face butterfly rash, pleura inflammation, pericardium inflammation, fingers and toes poor circulation, joints arthritis, muscles aches, mouth and nose ulcers, systemic: low-grade fever photosensitivity. [Return to Figure 11.15].
Attribution
Except where otherwise noted, this chapter is adapted from “Lymphatic and Immune Systems” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Lymphatic and Immune Systems chapter content into sub-chapters.
- 1. itchy, 2. runny, 3. allergies, 4. dander, 5. medication, 6. distress, 7. heart 8. drainage, 9.Dyspnea, 10. daily, 11.rhinitis, 12. iron ↵
- 1. stones, 2.fatigue, 3.fever 4. tonsillitis, 5. temperature, 6. cervical, 7. dysphagia, 8. erthema, 9. crypts, 10. tonsillolith, 11. pseudomembranes, 12. tonsillectomy, 13. gargles ↵
- 1. dysphagia, 2. prescribed, 3. lymph, 4. enlarged, 5. ibuprofen, 6. erythromycin, 7. tonsillectomy, 8. surgery ↵
Human Immunodeficiency Virus. An infectious disease, usually transmitted via blood or sexual fluids. It attacks the immune system and can lead to full-blown AIDS
Seroconversion is the reciprocal relationship between virus levels in the blood and antibody levels. As the antibody levels rise, the virus levels decline, and this is a sign that the immune response is being at least partially effective. Partially, because in many diseases, seroconversion does not necessarily mean a patient is getting well.(Betts et al., 2013)
CD4 is the receptor that HIV uses to get inside T cells and reproduce. CD4+ helper T cells play an important role in T cell immune responses and antibody responses. (Betts et al., 2013)
Reacting to something that would not normally evoke a reaction
antigens that evoke type 1 hypersensitivity (allergy) responses
Also called anaphylaxis. An inhaled, ingested or injected (bee sting) allergen causes a significant drop in blood pressure along with contractions of smooth muscles of the airways
HDN: Hemolytic Disease of the Newborn. Discussed in the chapter about Blood, this is a immune reaction between maternal and fetal blood due to the Rh antigen.
SLE is an autoimmune disease in which the immune system recognizes its own cell antigens as being "non-self" and mounts an immune response against them. As a result, many body tissues and vital organs become chronically inflamed and damaged. (https://www.cdc.gov/lupus/facts/detailed.html#sle)
a firm, raised reddened patch of skin
Lymphoma is a form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. These leukocytes do not function properly, and the patient is vulnerable to infection. (Betts. et al., 2013)
a soft, pale swelling at the site surrounded by a red zone (Betts et al., 2013)

