9.4 – Heart Diseases, Disorders and Diagnostic Testing
Cardiomyopathy
The heart of a well-trained athlete can be considerably larger than the average person’s heart. This is because exercise results in an increase in muscle cells called hypertrophy. Hearts of athletes can pump blood more effectively at lower rates than those of non-athletes. However, when an enlarged heart is not the result of exercise, it may be due to hypertrophic cardiomyopathy. The cause of an abnormally enlarged heart muscle is unknown, but the condition is often undiagnosed and can cause sudden death in apparently otherwise healthy young people (Betts et al., 2013).
Other types of cardiomyopathy include:
- Dilated cardiomyopathy, which also has an unknown cause and is seen in people of any age. In this disorder, one of the ventricles of the heart is larger than normal.
- Arrhythmogenic cardiomyopathy, an inherited condition which results in irregular heart rhythms.
- Restrictive cardiomyopathy, which is a complication of other conditions that cause the myocardium to scar or stiffen (Centers for Disease Control and Prevention, 2023).
Cardiomyopathy may also be caused by myocardial infarctions, myocardial infections, pregnancy, alcohol or cocaine abuse, autoimmune and endocrine diseases. Because the myocardium is responsible for contracting and pumping blood, patients with cardiomyopathy experience impaired heart function which may lead to heart failure (Centers for Disease Control and Prevention, 2023). To learn more about cardiomyopathy, visit the CDC’s cardiomyopathy web page [New Tab].
Heart Failure
Heart failure is defined as the inability of the heart to pump enough blood to meet the needs of the body. It is also called congestive heart failure (CHF). This condition causes swelling in the lower extremities and shortness of breath due to a buildup of fluid in the lungs. It may be caused by cardiomyopathy and it may lead to hypertension and heart valve disorders (Heart & Stroke, n.d.). To learn more, visit the Heart & Stroke’s congestive heart failure web page [New Tab].
Valvular Heart Disease
The four heart valves open and close at specific times during the cardiac cycle in order to ensure that blood flows in only one direction through the heart. This requires that these valves open and close completely. Infections such as rheumatic disease or bacterial endocarditis can affect the heart valves and result in scar tissue formation which interferes with valve function. Other causes of heart valve disease include: congenitally malformed valves, autoimmune diseases, and other cardiovascular diseases, such as aortic aneurysms and atherosclerosis (Centers for Disease Control and Prevention, 2019).
Concept check
Do you remember the names and locations of the 4 heart valves?
Heart valve disease may be asymptomatic or cause dyspnea, arrhythmias, fatigue, and other symptoms. It is often detected when a heart murmur is heard through a stethoscope (Centers for Disease Control and Prevention, 2019).
- Mitral Valve Prolaspse
- The mitral (bicuspid) valve is diseased or malformed and is not able to close completely, allowing the regurgitation of blood back into the left atrium during systole. Because some of the blood goes back into the atrium, insufficient blood is pumped out of the ventricle into the systemic circulation. This inability to close properly and the resulting regurgitation may also be found in other heart valves (Centers for Disease Control and Prevention, 2019).
- Aortic Stenosis
- The aortic valve is narrowed and hardened, preventing it from opening fully and allowing sufficient blood to travel to the systemic circulation. Any heart valve can be stenosed, but this disorder most often affects the aortic valve (Centers for Disease Control and Prevention, 2019).
Visit the CDC’s page on valvular heart disease [New Tab] to learn more.
Aneurysms
An aneurysm is a defect in the wall of an artery in which the wall becomes thin and weak and starts to balloon out as blood pulses against the vessel wall. This can happen to any artery and even to the myocardial walls. Aneurysms sometimes occur in the portion of the aorta that is in the thorax (see Figure 9.8). If these aneurysms start to leak between layers of the vessel wall, the condition is known as aortic dissection. If an aortic or cardiac aneurysm bursts, there is sudden, massive internal bleeding (Centers for Disease Control and Prevention, 2021).
People who smoke, have hypertension, hypercholesterolemia, and/or atherosclerosis have an increased risk of developing aneurysms. Having a family history of aneurysms or certain genetic diseases may also increase a person’s risk of developing an aneurysm.
Aneurysms are often asymptomatic and may be detected incidentally during diagnostic tests that are being done for other reasons. They are sometimes repaired surgically and sometimes treated with medications such as antihypertensives (Centers for Disease Control and Prevention, 2021; Tittley, n.d.). Visit the Canadian Society for Vascular Surgery’s page on thoracic aortic aneurysms [New Tab] to learn more.
Heart Defects
Fetal circulation is different from postnatal circulation. There are 2 extra openings in the fetal heart: the foramen ovale and the ductus arteriosus, which allow blood circulation that bypasses the immature fetal lungs. The fetal blood is reoxygenated by the mother’s lungs and transported between mother and fetus via the placenta. These two openings usually close around the time of birth (Betts, et al., 2013).
Septal defects are commonly first detected through auscultation. Unusual heart sounds may be detected because blood is not flowing and valves are not closing correctly. Medical imaging is ordered to confirm or rule out a diagnosis. In many cases, treatment may not be needed.
- Patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. If untreated, the condition can result in congestive heart failure.
- Patent foramen ovale is one type of atrial septal defect (ASD) due to a failure of the hole in the interatrial septum to close at birth.
- As much as 20 – 25 percent of the general population may have a patent foramen ovale; most have the benign, asymptomatic version, but in extreme cases, a surgical repair is required to close the opening permanently.
- Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. This allows blood that is relatively low in oxygen from the right ventricle to flow into the left ventricle and mix with the blood that is relatively high in oxygen.
- Symptoms include a distinct heart murmur, low blood oxygen percent saturation, dyspnea, polycythemia, clubbing of the fingers and toes, and in children, difficulty in feeding or failure to grow and develop.
- It is the most common cause of cyanosis following birth. Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging.
- In the case of severe septal defects, including both tetralogy of fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a blue baby. Regardless of normal skin pigmentation, individuals with this condition have an insufficient supply of oxygenated blood, which leads to cyanosis, especially when active (Betts et al., 2013).

Diseases of the Coronary Circulation
Coronary Artery Disease (CAD)
Coronary artery disease occurs when the buildup of plaque in the coronary arteries obstructs the flow of blood and decreases compliance of the vessels. This condition is called atherosclerosis. As the disease progresses and coronary blood vessels become more and more narrow, cells of the myocardium become ischemic, which causes symptoms of angina pectoris in some patients. If untreated, coronary artery disease can lead to MI.
The image below shows the blockage of coronary arteries on an angiogram (Betts et al., 2013).
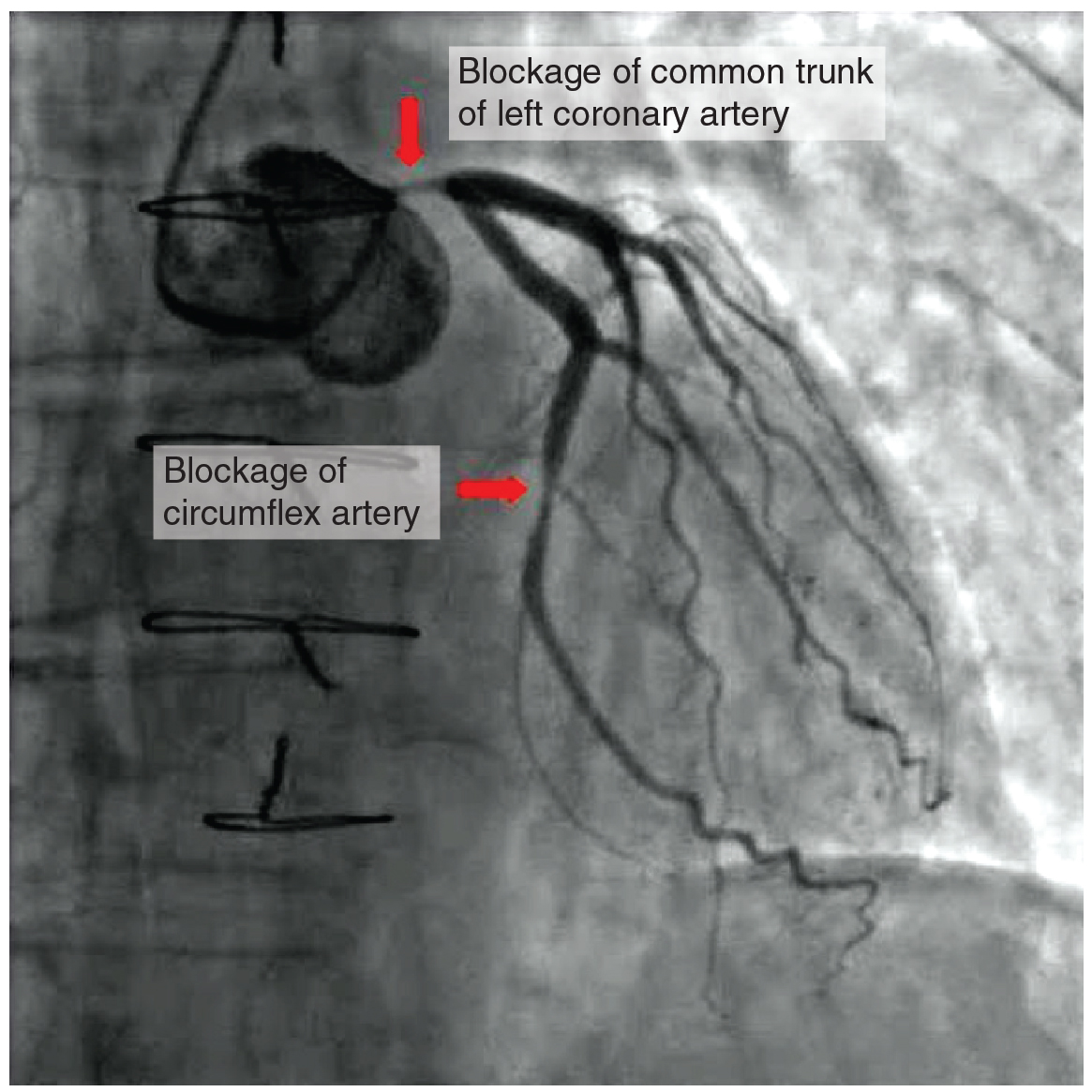
CAD is progressive and chronic. Risk factors include smoking, family history, hypertension, obesity, diabetes, high alcohol consumption, lack of exercise, stress, and hyperlipidemia. Treatments may include medication, changes to diet and exercise, angioplasty with a balloon catheter, insertion of a stent, or coronary artery bypass graft (CABG) (Betts et al., 2013).
- Angioplasty is a procedure in which the occlusion is mechanically widened with a balloon. A specialized catheter with an expandable tip is inserted into a blood vessel in the arm or leg, and then directed to the site of the occlusion. At this point, the balloon is inflated to compress the plaque material and to open the vessel to increase blood flow. Once the balloon is deflated and retracted, a stent consisting of a specialized mesh is typically inserted at the site of occlusion to reinforce the weakened and damaged walls and prevent re-occlusion.
- Coronary bypass surgery (Coronary artery bypass graft CABG) is a surgical procedure which grafts a replacement vessel obtained from another part of the body to bypass the occluded area (Betts et al., 2013).
Myocardial Infarction
Myocardial infarction (MI) is the medical term for a heart attack.
An MI normally results from a lack of blood flow to a region of the heart, resulting in death of the cardiac muscle cells. An MI often occurs when a coronary artery is blocked by the buildup of atherosclerotic plaque. It can also occur when a piece of an atherosclerotic plaque breaks off and travels through the coronary arterial system until it lodges in one of the smaller vessels. MIs may be triggered by excessive exercise, in which the partially occluded artery is no longer able to pump sufficient quantities of blood, or severe stress, which may induce spasm of the smooth muscle in the walls of the vessel (Betts et al., 2013).
Did You Know 1?
In the case of acute MI (AMI), there is often sudden pain beneath the sternum (retrosternal pain) called angina pectoris, often radiating down the left arm in males but not in female patients. Other common symptoms include dyspnea, palpitations, nausea and vomiting, diaphoresis, anxiety, and syncope. Many of the symptoms are shared with other medical conditions, including anxiety attacks and simple indigestion, so differential diagnosis is critical (Betts et al., 2013).
An MI can be confirmed by examining the patient’s ECG.
Other diagnostic tests include:
- echocardiography
- CT
- MRI
- Common blood tests indicating an MI include elevated levels of creatine kinase MB and cardiac troponin, both of which are released by damaged cardiac muscle cells (Betts et al., 2013)
MIs may induce dangerous heart rhythms and even cardiac arrest. Important risk factors for MI include coronary artery disease, age, smoking, high blood levels of LDL, low levels of HDL, hypertension, diabetes mellitus, obesity, lack of physical exercise, chronic kidney disease, excessive alcohol consumption, and use of illegal drugs (Betts et al., 2013).
Diseases of the (Electrical) Conduction System
Arrhythmia
Did You Know 2?
Arrhythmia does not mean an absence of a heartbeat! That would be asystole, or flat line!
Arrhythmia is defined as the absence of a regular rhythm, meaning that the heart rate is either too fast, too slow or just irregular.
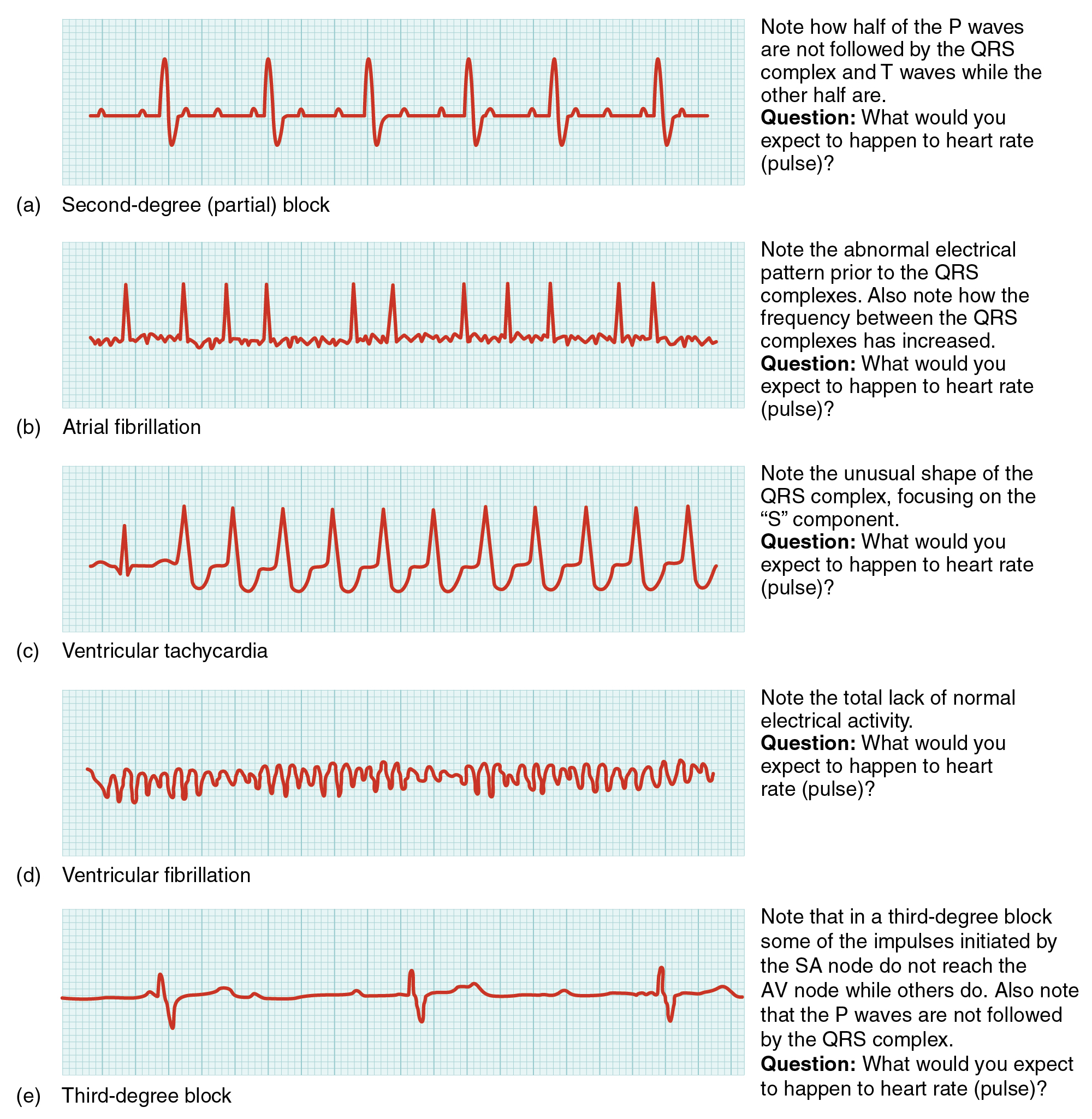
The heart’s natural pacemaker, the sinoatrial (SA) node, initiates an electrical impulse 60-90 times per minute in a resting adult. This impulse travels through the heart’s conduction system in order to ensure a smooth, coordinated pumping action. This electrical activity can be detected and recorded through the skin using an electrocardiograph. Arrhyhmias may occur when the SA node fails to initiate an impulse, or when the conduction system fails to transmit that impulse through the heart.
In the event that the electrical activity of the heart is severely disrupted, cessation of electrical activity or fibrillation may occur. In fibrillation, the heart beats in a wild, uncontrolled manner, which prevents it from being able to pump effectively.
- Atrial fibrillation is a serious condition, but as long as the ventricles continue to pump blood, the patient’s life may not be in immediate danger.
- Ventrical fibrillation is a medical emergency that requires life support, because the ventricles are not effectively pumping blood. Left untreated, ventricular fibrillation may lead to brain death.
The most common treatment is defibrillation, which uses special paddles to apply a charge to the heart from an external electrical source in an attempt to establish a normal sinus rhythm. A defibrillator effectively stops the heart so that the SA node can trigger a normal conduction cycle. External automated defibrillators (EADs) are being placed in areas frequented by large numbers of people, such as schools, restaurants, and airports. These devices contain simple and direct verbal instructions that can be followed by non-medical personnel in an attempt to save a life (Betts et al., 2013).
Abnormal Heart Rates
Bradycardia is the condition in a which resting adult heart rate drops below 60 bpm. A client exhibiting symptoms such as weakness, fatigue, dizziness, syncope, chest discomfort, palpitations or respiratory distress may indicate that the heart is not providing sufficient oxygenated blood to the tissues. If the patient is not exhibiting symptoms, then bradycardia is not considered clinically significant. The term relative bradycardia may be used with a patient who has a HR in the normal range but is still suffering from these symptoms. Most patients remain asymptomatic as long as the HR remains above 50 bpm.
Tachycardia is the condition in which the resting rate is above 100 bpm. Tachycardia is not normal in a resting patient and may be detected in pregnant women or individuals experiencing extreme stress. Some individuals may remain asymptomatic, but when present, symptoms may include dizziness, shortness of breath, rapid pulse, heart palpitations, chest pain, or syncope. Treatment depends upon the underlying cause, but may include medications, implantable cardioverter defibrillators, ablation, or surgery (Betts et al., 2013).
Heart Block
A heart block refers to an interruption in the normal conduction pathway. Heart blocks are generally named after the part of the conduction system that is causing the problem. For example, bundle branch blocks occur within either the left or right atrioventricular bundle branches.
AV blocks are often described by degrees. A first-degree or partial block indicates a delay in conduction between the SA and AV nodes. A second-degree or incomplete block occurs when some impulses from the SA node reach the AV node and continue, while others do not. In the third-degree or complete block, there is no correlation between atrial activity and ventricular activity. This means that none of the impulses generated by the SA node get transmitted to the rest of the heart and the AV node must take over as the primary pacemaker, initiating contractions at 40–60 beats per minute, which is adequate to maintain consciousness.
In order to speed up the heart rate and restore full sinus rhythm, a cardiologist can implant an artificial pacemaker, which delivers electrical impulses to the heart muscle to ensure that the heart continues to contract and pump blood effectively. These artificial pacemakers are programmable by the cardiologists and can either provide stimulation temporarily upon demand or on a continuous basis. Some devices also contain built-in defibrillators (Betts et al., 2013).
Cardiovascular System – Consultation Report
Cardiovascular System – Consultation Report (Text version)
Fill in the consultation report with the words listed below:
- shortness
- ECG
- implant
- embolism
- BP
- venous
- CBC and Diff
- hypercholesterolemia
- cardiovascular
- hypertension,
- WBC
- bradycardia
- intravenous
PATIENT NAME: Lorna GILBERT
AGE: 52
SEX: Female
DOB: February 27
DATE OF CONSULTATION: June 12
REQUESTING PHYSICIAN: Trevor Sharpe, MD, Family Medicine
CONSULTING PHYSICIAN: Kevin Palmer, MD, Cardiology
HISTORY: This 52-year-old female was referred to our cardiology clinic by her family physician Dr. Trevor Sharpe. She had visited her physician last month with complaints of persistent fatigue, dizziness, light-headedness, fainting, and an inability to exercise without experiencing ________[Blank 1] of breath. She claims that she is otherwise healthy; however, there is a history of ___________[Blank 2] diseases in her family. Her father had developed DVT during a long flight and subsequently suffered from pulmonary ___________[Blank 3]. Her mother had idiopathic intracranial _________[Blank 4] and died from MI at a relatively young age. The patient has 3 siblings, 2 of them suffering from hypertension and ______________[Blank 5].
LABORATORY DATA: The laboratory results show normal ____________[Blank 6]. Hemoglobin, Hct, __________[Blank 7] count, and platelet count are within normal range. The patient’s PT and partial thromboplastin time are normal.
ALLERGIES: She is not allergic to any medications.
PHYSICAL EXAMINATION: Today the patient is alert and oriented but feels completely exhausted. She is also complaining of a mild chest pain. Her ________[Blank 8]- is 180/110. Heart rate is in the high 50s with irregular rate and rhythm. NECK: is supple, without jugular ___________[Blank 9] distention or bruits. LUNGS: are clear, without wheezing, rhonchi, or rales.
IMPRESSION: I suspect the patient suffers from _________[Blank 10] and needs a pacemaker to regulate her heart rhythms. However, given the significant history of cardiovascular disorders in her family, I will order more tests before making a definite diagnosis.
PLAN: I will admit the patient to a telemetry bed and monitor her for 48 hours. If her chest pain worsens, she will be moved to CCU and will be treated with ____________[Blank 11] nitroglycerin. An __________[Blank 12] has also been ordered to confirm bradycardia. If the ECG results confirm my speculations, the patient will be scheduled for a pacemaker __________[Blank 13] as soon as possible.
_____________________________________
Kevin Palmer, MD, Cardiology
Check your answers: [1]
Activity source: Cardiovascular System – Consultation Report by Seedah Akram & Heather Scudder, from Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY- 4.0. /Text version added.
Medical Specialties and Procedures Related to the Heart
Cardiologists and Cardiovascular Surgeons
Cardiologists are medical doctors that specialize in diagnosing and treating heart disease non-invasively. Cardiovascular/thoracic surgeons provide surgical treatments for the heart and other thoracic organs (Canadian Medical Association, 2019). To learn more about these specialists, please visit the CMA’s Canadian Specialy Profiles web page [New Tab].
Cardiology Technologists
Cardiology Technologists complete a college training program and perform diagnostic tests such as electrocardiography, stress testing, Holter monitor testing, ambulatory blood pressure testing, as well as pacemaker monitoring and programming (Canadian Society of Cardiology Technologists, n.d.). Please visit the Canadian Society of Cardiology Technologists web page [New Tab] for more information.
Cardiovascular Perfusionists
Cardiovascular perfusionists complete a college training program and are responsible for operation of the heart-lung bypass machine during open heart surgery. They also monitor the patient’s vitals, adminstering IV fluids, and other drugs (Michener Institute of Education, n.d.). Please visit the Michener Institute’s Cardiovasular Perfusion program page [New Tab] for more information.
Image Descriptions
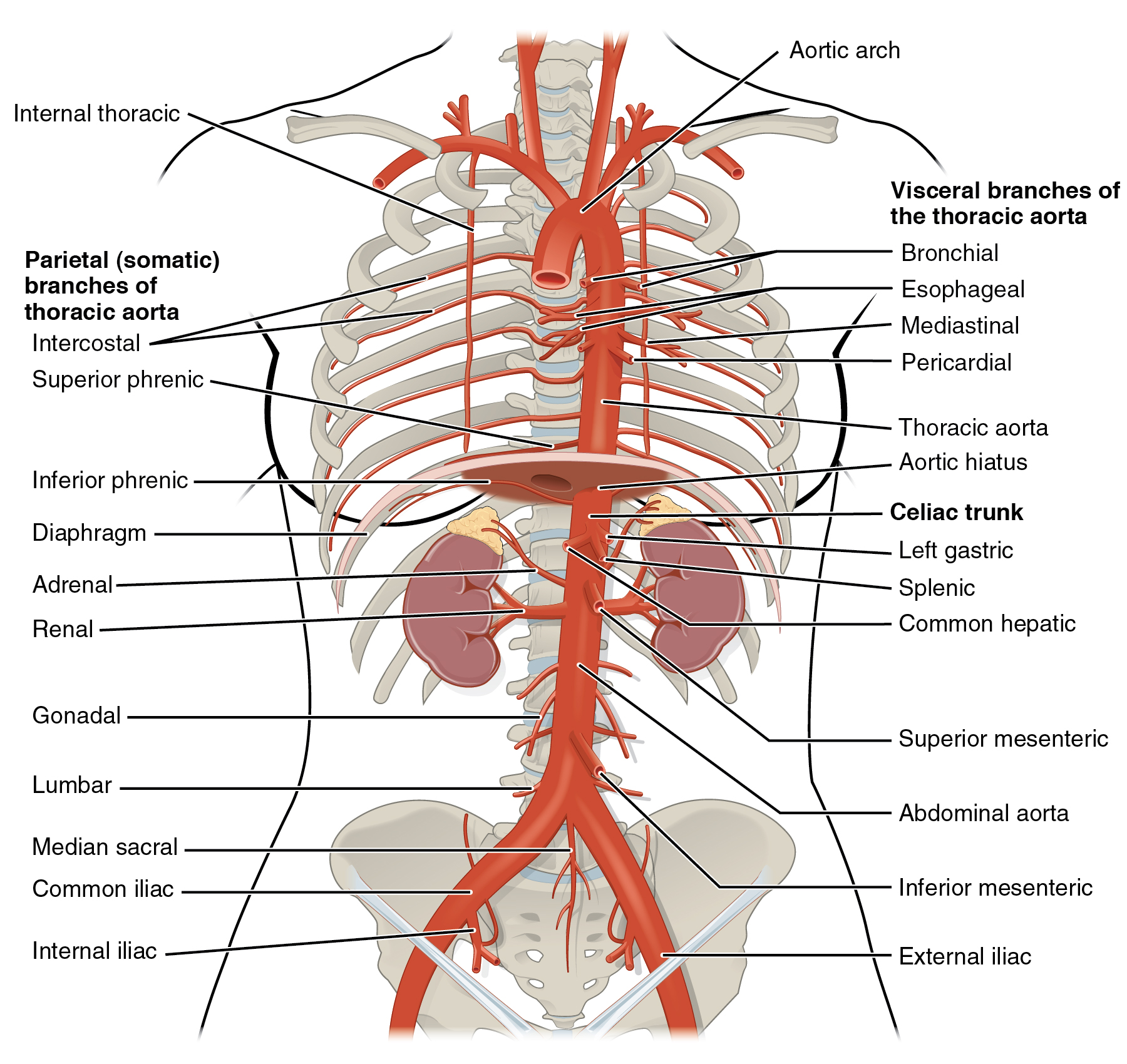
Figure 9.8 image description: This diagram shows the arteries in the thoracic and abdominal cavity. Visceral branches of the thoracic aorta labels (from top): bronchial, esophageal, mediastinal, pericardial, thoracic aorta, aortic hiatus, celiac trunk, left gastric, splenic, common hepatic, superior mesenteric, abdominal aorta, inferior mesenteric, external iliac. Parietal (somatic) branches of thoracic aorta labels (from top): intercostal, superior phrenic, inferior phrenic, diaphragm, adrenal, renal, gonadal, lumbar, medial sacral, common iliac, internal iliac. [Return to Figure 9.8].
Figure 9.9 image description: This diagram shows the structure of the heart with different congenital defects. The top left panel shows patent foramen ovale (label reads foramen ovale fails to close), the top right panel shows coarctation of the aorta (label reads narrow segment of aorta), the bottom left panel shows patent ductus ateriosus (label reads Ductus arteriosus remains open) and the bottom right shows tetralogy of fallot (labels read aorta emerges from both ventricles, interventricular septal defect, enlarged right ventricle, stenosed pulmonary semilunar valve). [Return to Figure 9.9].
Figure 9.11 image description: In this image the QT cycle for different heart conditions are shown. From top to bottom, the arrhythmias shown are second-degree partial block (text reads: Note how half of the P waves are not followed by the QRS complex and T waves while the other half are. Question: what would you expect to happen to heart rate?), atrial fibrillation (text reads: Note the abnormal electric pattern prior to the QRS complexes. Also note how the frequency between the QRS complexes has increased. Question: What t would you expect to happen to heart rate?), ventricular tachycardia (text reads: Note the unusual shape of the QRS complex, focusing on the S component. Question: What would you expect to happen to heart rate?), ventricular fibrillation (text reads: Note the total lack of normal electrical activity. Question: What would you expect to happen to heart rate?), and third degree block (text reads: Note that in a third-degree block some of the impulses initiated by the SA node do not reach the AV node while others do. Also note that the P waves are not followed by the QRS complex. Question: What would you expect to happen to heart rate?). [Return to Figure 9.11].
Attribution
Except where otherwise noted, this chapter is adapted from “Cardiovascular System – Heart” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford, licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax). Adaptations: dividing Cardiovascular System – Heart chapter content into sub-chapters.
- 1. shortness 2. cardiovascular 3. embolism 4. hypertension 5. hypercholesterolemia 6. CBC and Diff 7. WBC 8. BP 9. venous 10. bradycardia 11. intravenous 12. ECG 13. implant ↵
excessive development; increase in the size of cells but not the number of cells
High blood pressure
difficult breathing
absence of a regular heart rhythm
an abnormal heart sound
higher than normal levels of cholesterol in the blood
a hardening of the arteries that involves the accumulation of plaque
class of medications used to treat high blood pressure
Pertaining to after birth
opening between right and left atria, which is normal in the fetal heart
connection between pulmonary trunk and aorta in the fetal heart
listening to the heart using a stethoscope
the wall separating the right and left atria.
The wall of myocardium that separates the right and left ventricles
a disorder in which too many red blood cells are produced
broadening of the nails and exaggerated curvature of the nails
abnormal condition of blue (bluish colour, lips, and nail beds) caused by deoxygenation.
process of using sound to record the heart
a fatty material including cholesterol, connective tissue, white blood cells, and some smooth muscle cells
the ability of the blood vessels to dilate and constrict as needed
ischemia is a condition in which cells receive insufficient amounts of blood and oxygen
chest pain
an x-ray of the coronary blood vessels using a special catheter and an injection of dye
Excessive fat in the blood
blocked/blockage
A myocardial infarction without symptoms. The patient may not know that they are having an MI.
A feeling in the chest that may be caused by an irregular heart rhythm
sweating
fainting
ECG/EKG both these abbreviations mean electrocardiogram or a recording of the electrical impulses in the heart
Computerized tomography: a special 3-dimensional x-ray, also called CAT=Computerized Axial Tomography
Magnetic Resonance Imaging: Highly detailed images produced using a strong magnet and radio waves
an enzyme that catalyzes the conversion of creatine to phosphocreatine, consuming ATP
the regulatory protein for muscle contraction
low-density lipoprotein, often referred to as 'bad' cholersterol
high-density lipoprotein, often referred to as 'good' cholesterol
An endocrine system disorder in which the pancreas does not produce insulin or the cells of the body do not respond to insulin. This results in high levels of glucose in the blood.
a complete absence of electrical activity in the heart, which is represented by a flat line on ecg
instrument used to record electrical activity within the heart
pertaining to without symptoms
ICD, an electronic implant that provides an automatic shock to convert a dangerous heart rhythm to a normal heart rhythm
Using extreme heat or extreme cold to destroy cells in part of the heart which were causing abnormal rhythms.
atrioventricular: the area of the heart where the atria and ventricles meet
This is the rhythm set by the heart's pacemaker, the sinoatrial node and is usually approximately 60-90 beats per minute in a resting adult.
process of recording electrical activity of the heart
An electronic implant that initiates a heart beat

