3.5 – Integumentary System Changes (Aging, Disease and Disorders, Skin)
Changes Due to Aging
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength (see Figure 3.9). In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the elasticity and resilience of the skin, exhibits a reduced ability to regenerate, which leads to slower wound healing. The hypodermis, with its fat stores, loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin.

Did You Know?
A reduced sweating ability can cause some elderly to be intolerant to extreme heat.
Disease and Disorders
The integumentary system is susceptible to a variety of diseases, disorders, and injuries. These range from annoying but relatively benign bacterial or fungal infections that are categorized as disorders, to skin cancer and severe burns, which can be fatal. In this section, you will learn several of the most common skin conditions.
One of the most talked about diseases is skin cancer. Most cancers are identified by the organ or tissue in which the cancer originates. One common form of cancer is skin cancer.
In general, cancers result from an accumulation of DNA mutations. These mutations can result in cell populations that do not die when they should and uncontrolled cell proliferation that leads to tumors. Although many tumors are benign, some metastasize. Cancers are characterized by their ability to metastasize.
Sun Damage
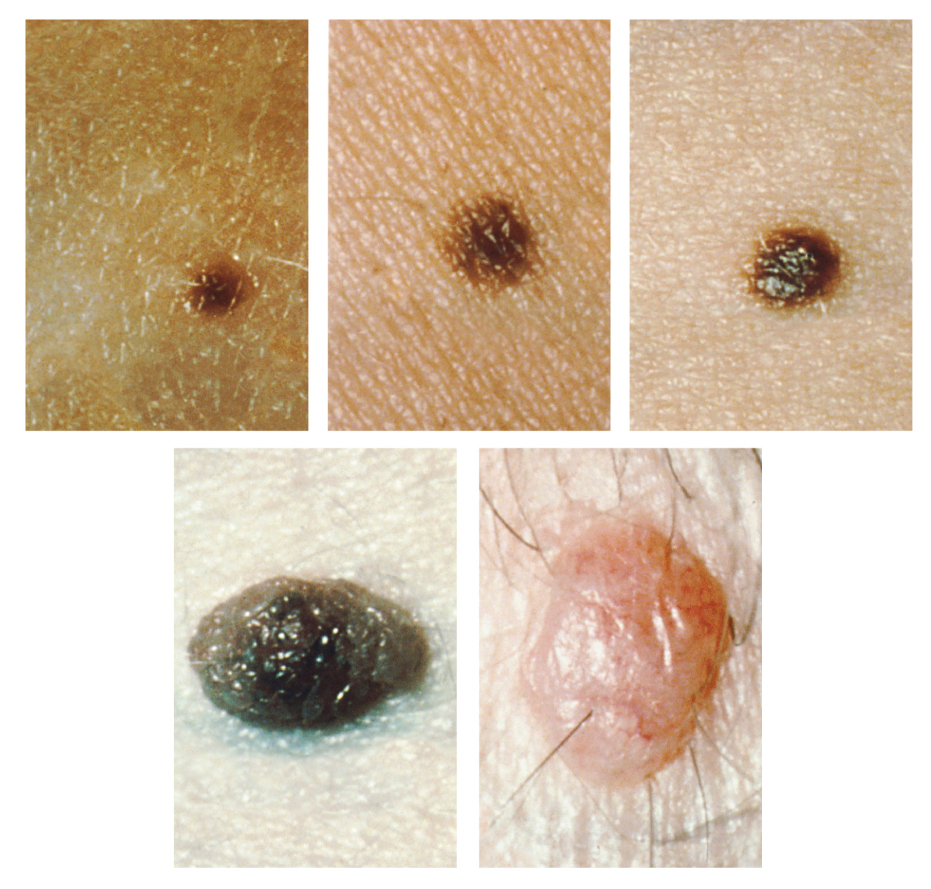
It requires about 10 days after initial sun exposure for melanin synthesis to peak, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Dark-skinned individuals can also get sunburns, but are more protected than pale-skinned individuals. Too much sun exposure can eventually lead to wrinkling due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer. When there is an irregular accumulation of melanocytes in the skin, freckles appear. Moles are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (see Figure 3.10).
Basal Cell Carcinoma (BCC)
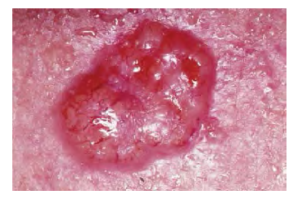
Basal cell carcinoma is a form of cancer that affects the mitotically active stem cells in the stratum basale of the epidermis. It is the most common of all cancers that occur in the United States and is frequently found on the head, neck, arms, and back, which are are as that are most susceptible to long-term sun exposure. Although UV rays are the main culprit, exposure to other agents, such as radiation and arsenic, can also lead to this type of cancer. Wounds on the skin due to open sores, tattoos, burns, etc. may be predisposing factors. Basal cell carcinomas start in the stratum basale and usually spread along this boundary. At some point, they begin to grow toward the surface and become an uneven patch, bump, growth, or scar on the skin surface (see Figure 3.11). Like most cancers, basal cell carcinomas respond best to treatment when caught early. Treatment options include surgery, freezing (cryosurgery), and topical ointments.
Squamous Cell Carcinoma (SCC)

Squamous cell carcinoma is a cancer that affects the keratinocytes of the stratum spinosum and presents as lesions commonly found on the scalp, ears, and hands (see Figure 3.12). It is the second most common skin cancer. The American Cancer Society reports that two of 10 skin cancers are squamous cell carcinomas, and it is more aggressive than basal cell carcinoma. If not removed, these carcinomas can metastasize. Surgery and radiation are used to cure squamous cell carcinoma.
Melanoma
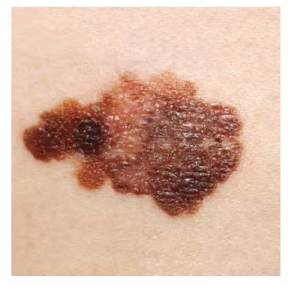
A melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the pigment-producing cells in the epidermis. Typically, a melanoma develops from a mole. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface (see Figure 3.13). Treatment typically involves surgical excision and immunotherapy.
ABCDE for Early Diagnosis
Doctors often give their patients the following ABCDE mnemonic to help with the diagnosis of early-stage melanoma. If you observe a mole on your body displaying these signs, consult a doctor.
- Asymmetry – the two sides are not symmetrical
- Borders – the edges are irregular in shape
- Color – the color is varied shades of brown or black
- Diameter – it is larger than 6 mm (0.24 in)
- Evolving – its shape has changed
Some specialists cite the following additional signs for the most serious form, nodular melanoma:
- Elevated – it is raised on the skin surface
- Firm – it feels hard to the touch
- Growing – it is getting larger
Albinism
Albinism is a genetic disorder that affects (completely or partially) the coloring of skin, hair, and eyes. This is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Recall that melanin helps protect the skin from the harmful effects of UV radiation. Individuals with albinism tend to need more protection from UV radiation, as they are more prone to sunburns and skin cancer. They also tend to be more sensitive to light and have vision problems due to the lack of pigmentation on the retinal wall (Betts et al., 2013).
Treatment of this disorder usually involves addressing the symptoms, such as limiting UV light exposure to the skin and eyes. In vitiligo, the melanocytes in certain areas lose their ability to produce melanin, possibly due to an autoimmune reaction. This leads to a loss of color in patches (see Figure 3.14). Neither albinism nor vitiligo directly affects the lifespan of an individual (Betts et al., 2013).

Changes in Skin Colouration
Other changes in the appearance of skin colouration can be indicative of diseases associated with other body systems.
- Liver disease or liver cancer can cause the accumulation of bile and the yellow pigment bilirubin, leading to the skin appearing yellow or jaundiced.
- Tumors of the pituitary gland can result in the secretion of large amounts of melanocyte-stimulating hormone (MSH), which results in a darkening of the skin.
- Addison’s disease can stimulate the release of excess amounts of adrenocorticotropic hormone (ACTH), which can give the skin a deep bronze color.
- A sudden drop in oxygenation can affect skin color, causing the skin to initially turn ashen (white).
- A prolonged reduction in oxygen levels, dark red deoxyhemoglobin becomes dominant in the blood, making the skin appear blue, a condition referred to as cyanosis. This happens when the oxygen supply is restricted, as when someone is experiencing difficulty in breathing because of asthma or a heart attack. However, in these cases the effect on skin color has nothing to do with the skin’s pigmentation (Betts et al., 2013).
Skin Disorders
Two common skin disorders are eczema and acne. Eczema is an inflammatory condition that occurs in individuals of all ages. Acne involves the clogging of pores, which can lead to infection and inflammation, and is often seen in adolescents. Other disorders, include seborrheic dermatitis (on the scalp), psoriasis, fungal infections, cold sores, impetigo, scabies, hives, and warts (Betts et al., 2013).
Eczema

Eczema is an allergic reaction that manifests as dry, itchy patches of skin that resemble rashes (see Figure 3.15). It may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. Symptoms are usually managed with moisturizers, corticosteroid creams, and immunosuppressants (Betts et al., 2013).
Acne
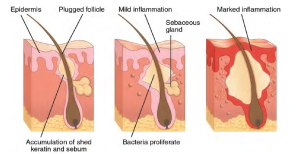
Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands (face and back). It is most common along with the onset of puberty due to associated hormonal changes, but can also occur in infants and continue into adulthood. Hormones, such as androgens, stimulate the release of sebum. An overproduction and accumulation of sebum along with keratin can block hair follicles. This plug is initially white. The sebum, when oxidized by exposure to air, turns black. Acne results from infection by acne-causing bacteria (Propionibacterium and Staphylococcus), which can lead to redness and potential scarring due to the natural wound healing process (see Figure 3.16) (Betts et al., 2013).
Ringworm
Tinea or dermatophytosis is often referred to as ringworm. Ringworm presents as a circular rash that is itchy and red and can be found on various parts of the body. It is referred to by the location where it is found:
- Tinea pedis: feet or commonly referred to as athlete’s feet
- Tinea capitis: scalp
- Tinea barbae – beard
- Tinea manuum – hands
- Tinea unguium – Toenails and fingernails also called onychomycosis
- Tinea corporis – Body parts such as arms and legs (Center for Disease Control and Prevention, 2018a).
To learn more about ringworm, visit the Center for Disease Control and Prevention’s web page on fungal infections [New Tab].
Psoriasis
Psoriasis is a chronic autoimmune disorder that results in patches of thick red skin with the appearance of silvery scales. These patches can be found on elbows, knees, scalp, lower back, face, feet, fingernails, toenails and even the mouth. Psoriasis can be confused with other skin diseases, so a dermatologist is the best physician to diagnose psoriasis. Treatments may include creams, ointments, ultraviolet light therapy and medication (Center for Disease Control and Prevention, 2018). To learn more, visit the Canadian Association of Psoriasis Patients’ page on psoriasis and inflammation [New Tab].
Injuries
Because the skin is the part of our bodies that meets the world most directly, it is especially vulnerable to injury. Injuries include burns, wounds, as well as scars and calluses. They can be caused by sharp objects, heat, excessive pressure or friction to the skin (Betts et al., 2013).
Skin injuries set off a healing process that occurs in several overlapping stages.
- The first step to repairing damaged skin is the formation of a blood clot that helps stop the flow of blood and scabs over time. Many different types of cells are involved in wound repair, especially if the surface area that needs repair is extensive.
- Before the basal stem cells of the stratum basale can recreate the epidermis, fibroblasts mobilize and divide rapidly to repair the damaged tissue by collagen deposition, forming granulation tissue.
- Blood capillaries follow the fibroblasts and help increase blood circulation and oxygen supply to the area.
- Immune cells, such as macrophages, roam the area and engulf any foreign matter to reduce the chance of infection (Betts et al., 2013).
Burns
A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can lead to a massive loss of fluid. Dehydration, electrolyte imbalance, and renal and circulatory failure follow, which can be fatal. Burn patients are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to the lives of burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of skin (Betts et al., 2013).
Burn Classification
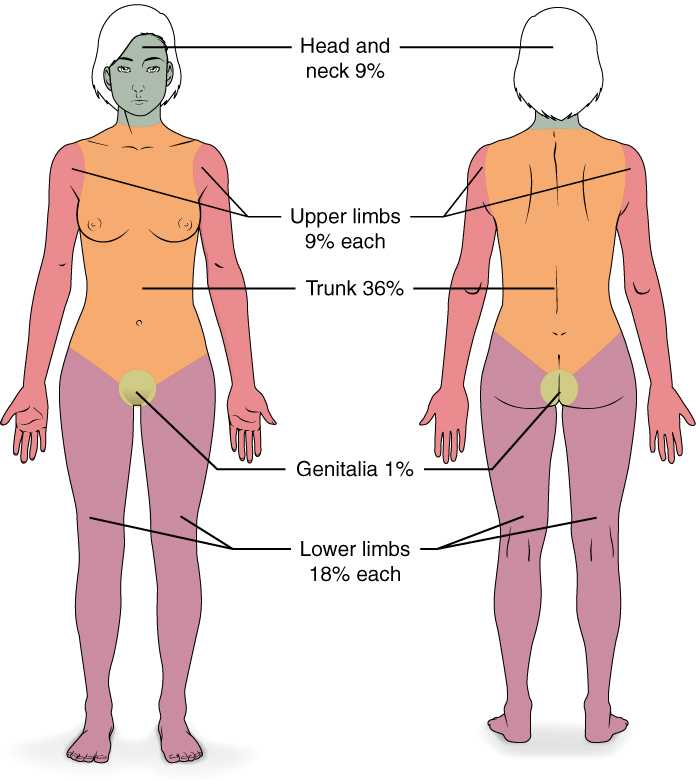
Burns are sometimes measured in terms of the size of the total surface area affected. This is referred to as the rule of nines, which associates specific anatomical areas with a percentage that is a factor of nine (see Figure 3.17) (Betts et al., 2013).
Burns are also classified by the degree of their severity.
- A first-degree burn is a superficial burn that affects only the epidermis. Although the skin may be painful and swollen, these burns typically heal on their own within a few days. Mild sunburn fits into the category of a first-degree burn.
- A second-degree burn goes deeper and affects both the epidermis and a portion of the dermis. These burns result in swelling and painful blistering of the skin. It is important to keep the burn site clean and sterile to prevent infection. If this is done, the burn will heal within several weeks.
- A third-degree burn fully extends into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns that may appear white, red, or black; they require medical attention and will heal slowly without it.
- A fourth-degree burn is even more severe, affecting the underlying muscle and bone.
Oddly, third and fourth-degree burns are usually not as painful because the nerve endings themselves are damaged. Full-thickness burns cannot be repaired by the body, because the local tissues used for repair are damaged and require debridement, or amputation in severe cases, followed by grafting of the skin from an unaffected part of the body, or from skin grown in tissue culture for grafting purposes. Skin grafts are required when the damage from trauma or infection cannot be closed with sutures or staples (Betts et al., 2013).
Scars and Keloids
Most cuts or wounds, with the exception of ones that only scratch the epidermis, lead to scar formation. Scarring occurs in cases in which there is repair of skin damage, but the skin fails to regenerate the original skin structure. Fibroblasts generate scar tissue in the form of collagen, and the bulk of repair is due to the basket-weave pattern generated by collagen fibers and does not result in regeneration of the typical cellular structure of skin. Instead, the tissue is fibrous in nature and does not allow for the regeneration of accessory structures, such as hair follicles, sweat glands, or sebaceous glands (Betts et al., 2013).
Sometimes, there is an overproduction of scar tissue, because the process of collagen formation does not stop when the wound is healed; this results in a keloid. In contrast, scars that result from acne and chickenpox have a sunken appearance and are called atrophic scars (Betts et al., 2013)
Scarring of skin after wound healing is a natural process and does not need to be treated further. The application of mineral oil and lotions may reduce the formation of scar tissue. However, modern cosmetic procedures, such as dermabrasion, laser treatments, and filler injections have been invented as remedies for severe scarring. All of these procedures try to reorganize the structure of the epidermis and underlying collagen tissue to make it look more natural (Betts et al., 2013).
Bedsores and Stretch Marks
Skin and its underlying tissue can be affected by excessive pressure. One example of this is called a bedsore. Bedsores, also called decubitus ulcers, are caused by constant, long-term, unrelieved pressure on certain body parts that are bony, reducing blood flow to the area and leading to necrosis. Bedsores are most common in elderly patients who have debilitating conditions that cause them to be immobile. Most hospitals and long-term care facilities have the practice of turning the patients every few hours to prevent the incidence of bedsores. If left untreated bedsores can be fatal if they become infected (Betts et al., 2013)
The skin can also be affected by pressure associated with rapid growth. A stretch mark results when the dermis is stretched beyond its limits of elasticity, as the skin stretches to accommodate the excess pressure. Stretch marks usually accompany rapid weight gain during puberty and pregnancy. They initially have a reddish hue, but lighten over time. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen (Betts et al., 2013).
Calluses
When you wear shoes that do not fit well and are a constant source of abrasion on your toes, you tend to form a callus at the point of contact. This occurs because the basal stem cells in the stratum basale are triggered to divide more often to increase the thickness of the skin at the point of abrasion to protect the rest of the body from further damage. This is an example of a minor or local injury, and the skin manages to react and treat the problem independent of the rest of the body. Calluses can also form on your fingers if they are subject to constant mechanical stress, such as long periods of writing, playing string instruments, or video games. A corn is a specialized form of callus. Corns form from abrasions on the skin that result from an elliptical-type motion (Betts et al., 2013).
Integumentary System Medical Terms In Use
Medical Terms in Context: Consultation Report
Consultation Report (Text Version)
INTEGUMENTARY SYSTEM – CONSULTATION REPORT
Fill in the consultation report with using the following words:
- Excisional
- Lesion
- Asymmetrical
- Mole
- Benign
- Biopsy
- Irregular
PATIENT NAME: Rosemary COOMBS
AGE: 54
Sex: Female
DOB: December 2
DATE OF CONSULTATION: May 29
REQUESTING PHYSICIAN: Trevor Sharpe, MD, Family Medicine
CONSULTING PHYSICIAN: Donna Brown, MD, Dermatology
HISTORY: This 54-year-old white female, went to her family doctor a year ago when she noticed a dark brown spot on her neck. The spot was a six cm, dark brown, flat ______[Blank 1] with smooth borders that appeared _____[Blank 2] . Ms. Coombs recently went to Dr. Sharpe for a physical and the _____[Blank 3] was examined, it was suggested that Ms. Coombs see me.
PAST HISTORY: No known history of any skin disorders.
PHYSICAL EXAMINATION: Normal except for the lesion on her chest which has grown to 1.3 cm in diameter and ______[Blank 4] in shape. It is mainly dark brown, with regions of darker black. The borders are ______[Blank 5] in outline. There is some blackened areas that are slightly elevated.
PLAN: I have booked a follow up appointment for next week to do an _____[Blank 6] biopsy. I will then send the specimen for a _____[Blank 7]. Another follow up appointment will be made once I receive the results of the biopsy.
____________________________
Donna Brown, MD, Dermatology
Note: Report samples (H5P and Pressbooks) are to encourage learners to identify correct medical terminology and do not represent the Association for Health Documentation Integrity (AHDI) formatting standards.
Check your answers: [1]
Activity source: Integumentary system – consultation report by Heather Scudder, licensed under CC BY 4.0./Text version added.
Medical Terminology in Text
Medical Terminology (Text version)
Fill in the spaces below with the following terms:
- Xero
- o
- hidr
- rhytid
- ous
- genic
- logist
- o
- ectomy
- derma
- cutane
- itis
- ous
- o
- al
- necr
- o
- o
- plasty
- sis
- phagia
- tone
- trans
- sub
- cutane
- dermat
- derma
- kerat
- aden
- auto
- derm
- per
- onych
- dermat
____[Blank 1a] / ____ [Blank 2a]/ ____[Blank 3a] / ____[Blank 4a] refers to the surgical repair of one’s own skin.
Something that generates the production of epidermal tissues might be called ____[Blank 2a] / ____[Blank 2b] /____[Blank 2b].
____[Blank 3a] / ____[Blank 3b] / ____[Blank 3c] refers to something in state of death.
____[Blank 4a] /____[Blank 4b] /____[Blank 4c] is a technical name for finger-biting.
____[Blank 5a] / ____[Blank 5b] / ____[Blank 5c] means pertaining to through the skin.
____[Blank 6a] / ____[Blank 6b] / ____[Blank 6c] injection is given under the skin.
During the winter months many people complain of ____[Blank 7a] / ____[Blank 7b] and use extra lotion.
A patch filled with medication, applied to the skin so that medication goes through the skin is referred to as a ____[Blank 8a] / ____[Blank 8b] / ____[Blank 8c] patch.
An instrument use to cut the skin for biopsy is referred to as a ____[Blank 9a] / ____[Blank 9b].
A specialist who studies and treats disorders and diseases of the skin is referred to as a ____[Blank 10a] / ____[Blank 10b] / ____[Blank 10b]/
The medical term that means a sweat gland is inflamed is ____[Blank 11a] / ____[Blank 11b] / ____[Blank 11c].
The medical term to excise wrinkles or commonly referred to as a facelift is ____[Blank 12a] / ____[Blank 12b].
Check your answers: [2]
Activity source: Integumentary Medical Terms by Jesslyn Wilkinson, licensed under CC BY 4.0./Text version added.
Medical Specialties and Procedures Related to the Integumentary System
A dermatologist is a medical doctor with specialized training in treating diseases, disorders and injuries related to the integumentary system and its accessory structures. There are many dermatologic subspecialties such as cosmetic dermatology, dermatopathology, and pediatric dermatology. To learn more visit the Dermatology and Subspecialties section [New Tab] of the Canadian Dermatology Association website.
Dermatologists can be specially trained to perform a procedure called Mohs surgery. Mohs surgery excises skin cancers in thin layers until all cancer is removed from the tissue (Mayo Clinic Staff, 2017).
Image Descriptions
Figure 3.9 image description: This figure consists of two photos. One photo shows a young woman on the phone. Her skin is smooth and unwrinkled. The other photo shows an elderly woman in the same posture while on the phone. The skin of her hands and forearms is wrinkled. [Return to Figure 3.9].
Figure 3.10 image description: Five photos of moles. The three upper photos show moles that are small, flat, and dark brown. The bottom left photo shows a dark black mole that is raised above the skin. The bottom right photo shows a large, raised, reddish mole with protruding hairs. [Return to Figure 3.10].
Figure 3.11 image description: The image shows a section of skin tissue with a raised reddened growth in a circular shape with irregular margins. The raised area is shiny. In this appearance the growth appears to be a basal cell carcinoma. [Return to Figure 3.11]
Figure 3.17 image description: This diagram depicts the percentage of the total body area burned when a victim suffers complete burns to regions of the body. Complete burning of the face, head and neck account for 19% of the total body area. Burning of the chest, abdomen and entire back above the waist accounts for 36% of the total body area. Anterior and posterior surfaces of the arms and hands account for 18% of the total body area (9% for each arm). The anterior and posterior surface of both legs, along with the buttocks, accounts for 36% of the total body area (18% for each leg). Finally, the anterior and posterior surfaces of the genitalia account for 1% of the total body area. [Return to Figure 3.17].
Attribution
Except where otherwise noted, this chapter is adapted from “Integumentary System” in Building a Medical Terminology Foundation by Kimberlee Carter and Marie Rutherford licensed under CC BY 4.0. / A derivative of Betts et al., which can be accessed for free from Anatomy and Physiology (OpenStax).Adaptations: dividing Integumentary System chapter content into sub-chapters.
- 1. Mole, 2. Benign, 3. Lesion, 4. Asymmetrical, 5. Irregular, 6. Excisional, 7. Biopsy ↵
- 1. Dermat /o /auto /plasty. 2. Kerat /o /genic. 3. Necr /o /sis. 4. Onych /o /phagia. 5. Per /cutane /ous. 6. Sub /cutane /ous. 7. Xero /derma. 8. Trans /derm /al. 9. Derma /tone. 10. Dermat /o /logist. 11. Hidr /aden /itis. 12. Rhytid /ectomy. ↵
abnormal cells in the body dividing uncontrollably.
noncancerous, harmless
Production of cells that can mobilize and establish tumors in other organs of the body
Yellow coloured
abnormal condition of blue (bluish colour, lips, and nail beds) caused by deoxygenation.
loss of fluids/water is greater than what is taken in.
pertaining to within the vein
invasion by disease causing organisms
disease causing agents
excision of damaged tissue or foreign object.
collagen-rich skin formed after the process of wound healing that differs from normal skin
formation of a raised or hypertrophic scar
tissue death
pertaining to dermatology
Study of diseases of the skin.
remove by cutting out

