11 Obstetrics
Learning Objectives
- Identify the common processes in obstetrics
- Describe the specialty of obstetrics
- Spell the medical terms used in obstetrics and use correct abbreviations
- Identify the medical specialties associated with obstetrics
- Explore common complications and procedures related to obstetrics
Obstetric Word Parts
Introduction to Obstetrics
Obstetrics is a specialty that is concerned with the mother and fetus during pregnancy, childbirth and the immediate postpartum period. Obstetricians study obstetrics and gynecology and are referred to as OB/GYN Obstetrics and Gynecology.
Watch this video:
Media 11.1. Reproductive System, Part 4 – Pregnancy & Development: Crash Course A&P #43 [Online video]. Copyright 2015 by CrashCourse.
Obstetrics Medical Terms
Fertilization
Fertilization occurs when a sperm and an oocyte (egg) combine. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell is called a zygote.
Most of the time, a woman releases a single egg during an ovulation cycle.
- In approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized.
- Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times.
- Less common, one zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins.
Stages of Childbirth
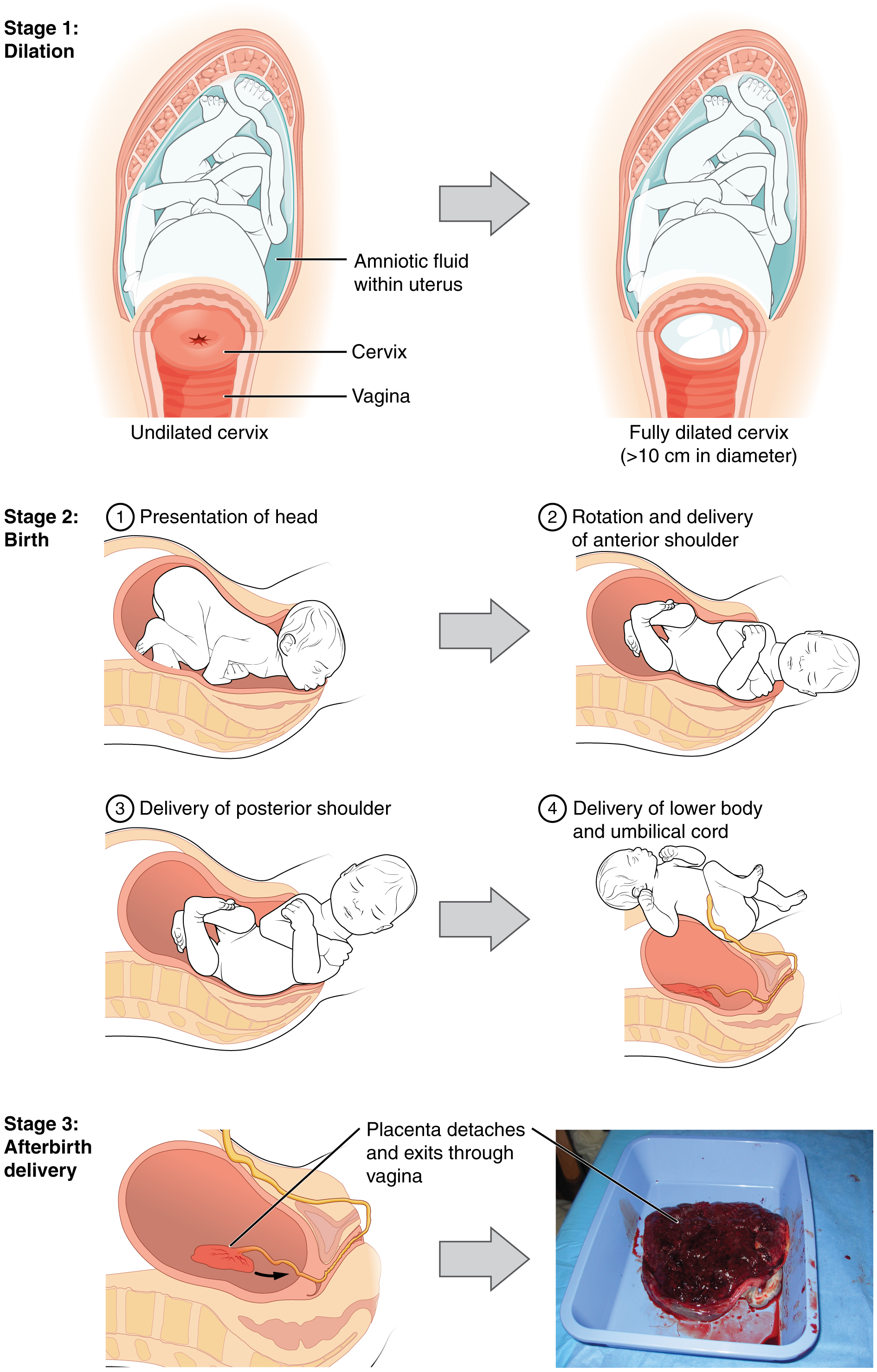
The process of childbirth can be divided into three stages (see Figure 11.1):
- cervical dilation
- expulsion of the newborn
- after birth
For vaginal birth to occur, the cervix must dilate fully to 10 cm in diameter, wide enough to deliver the newborn’s head. The dilation stage is the longest stage of labour and typically takes 6-12 hours. However, it varies widely and may take minutes, hours, or days, depending in part on whether the mother has given birth before. In each subsequent labour, this stage tends to be shorter.
Concept Check
- How is a due date determined?
- Explain the difference between a monozygotic pregnancy and a dizygotic pregnancy.
Homeostasis in the Newborn: Apgar Score
In the minutes following birth, a newborn must undergo dramatic systemic changes to be able to survive outside the womb. An obstetrician, midwife, or nurse can estimate how well a newborn is doing by obtaining an Apgar score. The Apgar score was introduced in 1952 by the anesthesiologist Dr. Virginia Apgar as a method to assess the effects on the newborn of anesthesia given to the labouring mother. Healthcare providers now use it to assess the general well-being of the newborn, whether or not analgesics or anesthetics were used.
The five criteria, skin colour, heart rate, reflex, muscle tone, and respiration, are assessed and each criterion is assigned a score of 0, 1, or 2. Scores are taken at 1 minute after birth and again at 5 minutes after birth. Each time scores are taken, the five scores are added together. High scores (out of a possible 10) indicate the baby has made the transition from the womb well, whereas lower scores indicate that the baby may be in distress.
The technique for determining an Apgar score is quick and easy, painless for the newborn, and does not require any instruments except for a stethoscope. A convenient way to remember the five scoring criteria is to apply the mnemonic APGAR:
- Appearance (skin colour)
- Pulse (heart rate)
- Grimace (reflex)
- Activity (muscle tone)
- Respiration
Of the five Apgar criteria, heart rate and respiration are the most critical. Poor scores for either of these measurements may indicate the need for immediate medical attention to resuscitate or stabilize the newborn. In general, any score lower than 7 at the 5-minute mark indicates that medical assistance may be needed. A total score below 5 indicates an emergency situation. Normally, a newborn will get an intermediate score of 1 for some of the Apgar criteria and will progress to a 2 by the 5-minute assessment. Scores of 8 or above are normal.
Obstetrics Medical Terms not Easily Broken into Word Parts
Obstetrics Abbreviations
Medical Terms in Context
Procedures Related to Obstetrics
In Vitro Fertilization (IVF)
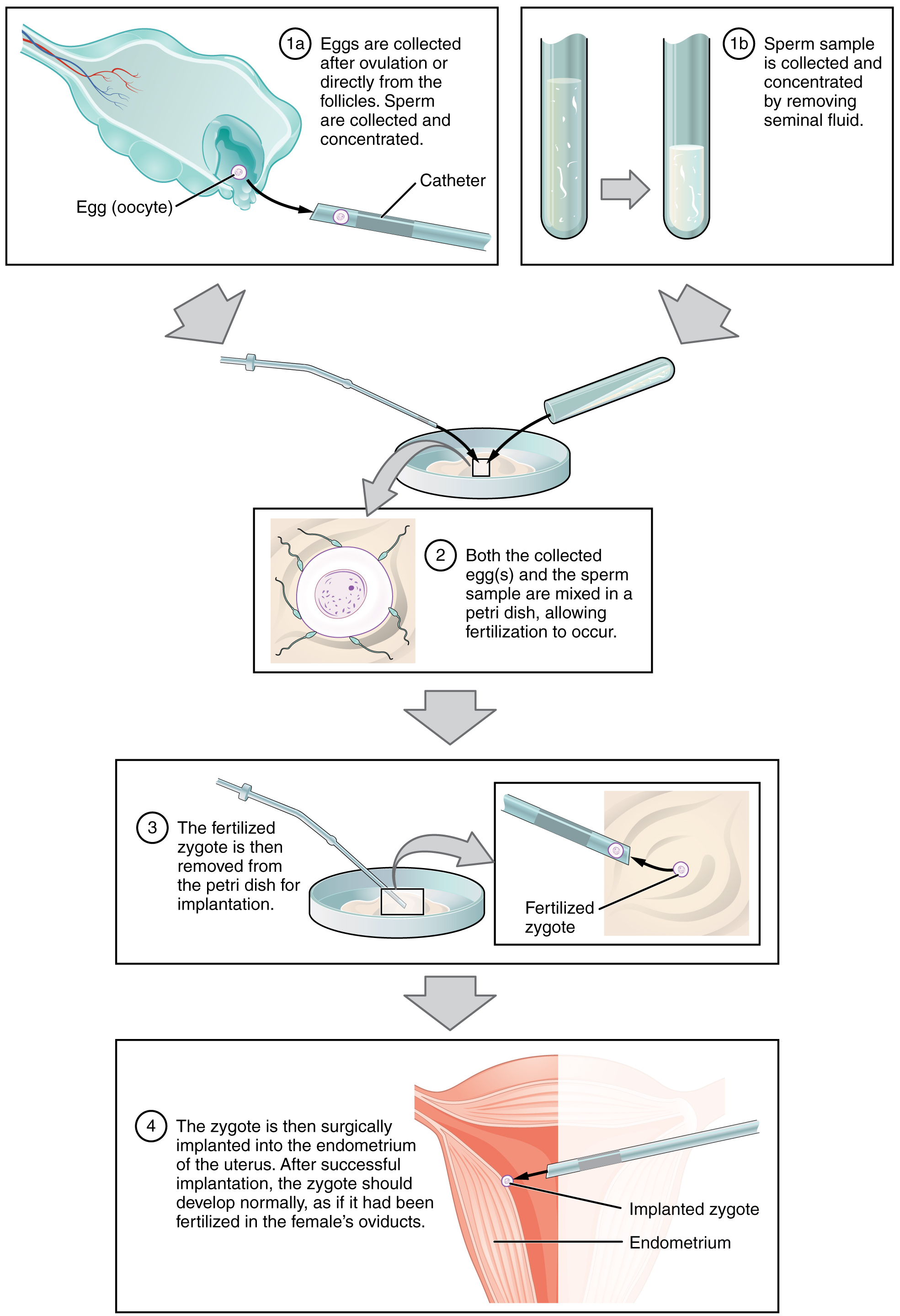
IVF, which stands for in vitro fertilization, is an assisted reproductive technology. In vitro, which in Latin translates to in glass, refers to a procedure that takes place outside of the body. There are many different indications for IVF. For example, a woman may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. A man may have a low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg. Figure 11.2 illustrates the steps involved in IVF.
Prenatal Screening and Diagnostic Testing
Obstetrics Vocabulary
Abortion
Termination of a pregnancy before the fetus is viable.
Alpha-fetoprotein test (AFP)
A maternal blood test to detect potential fetal abnormalities such as neural tube defects or multiple pregnancies; The AFP is taken between 14 and 19 weeks gestation.
Amenorrhea
Absences of the flow of menses, no period; one of the first signs of pregnancy or menopause.
Amniocentesis
Surgical puncture to remove a small amount of amniotic fluid through a needle via the abdomen. The fluid is tested for any potential fetal abnormalities.
Artificial insemination
A process where the semen is introduced into the vagina by mechanical means, thus called artificial.
Breech
The position of the fetus is feet first. Ideally, the position of the fetus should be headfirst for a safer delivery.
Caesarian section (C/S, c-section)
Delivery of the fetus through an abdominal incision.
Cephalopelvic disproportion
A condition where the infant’s head is larger than the pelvic outlet and therefore will require a c-section.
Cerclage
A suture inserted into the cervix to prevent dilation and prevention miscarriage. The suture is removed when the fetus is full-term and allows the vaginal delivery to proceed.
Cephalic version
Pertaining to turning the head; this procedure is done on the fetus when they are in the head-down position.
Chorionic villus sampling
A small piece of placenta is taken and tested to determine potential for birth defects.
Dilation and curettage (D&C)
A procedure where the cervix is dilated (widened) and a curette (a sharp instrument) is used to remove the lining of the uterus. This procedure is conducted when there is abnormal bleeding from the uterus and also to remove any products of conception, for example following an incomplete miscarriage or abortion.
Eclampsia
A very serious condition in pregnancy with hypertension; patients are at high risk of coma, convulsions, and even death.
Ectopic pregnancy
The embryo implants any other place but the inner endo-uterine lining.
Episiotomy
A procedure where an incision is made to widen the vaginal opening to prevent ripping or tearing of the perineum during delivery.
Gestation
The process of being pregnant.
Gestational Diabetes
The condition or developing diabetes during pregnancy. The newborn tend to be large at delivery and the mother is monitored closely for weight gain and glucose testing. The goal is to balance the sugars so the fetus is not too large for a vaginal delivery.
Gestational Hypertension
A condition where there is an increase in blood pressure during pregnancy. Blood pressure is monitoring closely during pregnancy for the safety of the mother and infant.
Hyperemesis
Excessive vomiting during pregnancy.
Hyperemesis Gravidarum
Hyperemesis can occur with any pregnant women, even a woman who miscarries. Often these women may require hospitalization for fluid and electrolyte intake.
Induction
The process of bringing on or starting labour. This may be done with a membrane sweep or through the use of IV oxytocin.
In vitro Fertilization (IVF)
A process where the ova is fertilized outside the body and then implanted into the uterus.
Meconium Staining
When the fetus defecates while in utero; the first defecation is called meconium, it is black and sticky. If the infant inhales the meconium upon delivery or through the birth canal, the meconium can be aspirated into the lungs and stick to the lung tissue. The newborn will have problems breathing and go into distress. The newborn’s umbilical cord will be stained a brownish colour.
Natal
Pertaining to born.
Neonatal
Pertaining to the newborn. For example neonatal record, neonatal unit
Non-stress test
Test conducted on the pregnant woman to assess the fetal heart rate (FHR).
Nulligravida
A woman who has never been pregnant.
Obstetrician
The person who specializes in the study of obstetrics and gynecology and are referred to as OB/GYN Obstetrics and Gynecology.
Oligohydramnios
A condition where there is minimal amniotic fluid within the placental sac. Too little fluid can restrict the fetus from movement and growth.
Oocyte
Female gamete.
Oxytocia
A rapid birth.
Placenta Abruptio or Abruptio Placenta
Occurs when the placenta prematurely becomes detached from the uterine wall. This is a medical emergency and requires an immediate c-section to safe both the woman and infants lives. the infant will not be getting oxygen from the mother and the mother may hemorrhage.
Placenta Previa
Occurs when the placenta partially or completely covers the cervical os (opening).
Polyhydramnios
A condition where there is excessive amniotic fluid in the placenta. The delivery will be a c-section to prevent bleeding during delivery of the fetus.
Preeclampsia
The abnormal condition in pregnancy where the patient experiences hypertension, edema and proteinuria.
Primigravida
First pregnancy.
Sperm
Male gamete (spermatozoon).
Vaginal Birth Following a C-Section
Having a vaginal delivery after a previous c-section delivery.
Zygote
Process of fertilization is complete and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human.
Zygote Intrafallopian Transfer (ZIFT)
Mixing of the ova and sperm in a laboratory. Fertilization is confirmed to grow into zygotes and then are inserted into the Fallopian tubes (Healthwise Staff, 2018).
Test Yourself
References
[CrashCourse]. (2019, November 23). Reproductive System, Part 4 – Pregnancy & Development: Crash Course A&P #43 [Video]. YouTube. https://youtu.be/BtsSbZ85yiQ
Genetics Education Canada Knowledge Organization. (2019). Guide to understanding prenatal screening tests. https://geneticseducation.ca/public-resources/prenatal-and-preconception-genetics/guide-to-understanding-prenatal-screening-tests/#diagnostic
Government of Canada. (2019, May 28). Fertility. https://www.canada.ca/en/public-health/services/fertility/fertility.html
Healthwise Staff. (2018, September 5). Gamete and zygote intrafallopian transfer (GIFT and ZIFT) for infertility. HealthLink BC. https://www.healthlinkbc.ca/health-topics/hw202763
Image Descriptions
Figure 11.1 image description: This multi-part figure shows the different stages of childbirth. The top panel shows dilation of the cervix (undilated vs fully dilated), the middle panel shows birth (presentation of the head, rotation and delivery of anterior shoulder, delivery of posterior shoulder, delivery of lower body and umbilical cord), and the bottom panel shows afterbirth delivery. [Return to Figure 11.1].
Figure 11.2 image description: This multi-part figure shows the different steps in in vitro fertilization. The top panel shows how the oocytes and the sperm are collected and prepared (text reads: 1a) eggs are collected after ovulation or directly from the follicles. Sperm are collected and concentrated. 1b) Sperm sample is collected and concentrated by removing seminal fluid). The next panel shows the sperm and oocytes being mixed in a petri dish (text labels read: 2) both the collected eggs and the sperm sample are mixed in a petri dish, allowing fertilization to occur). The panel below that shows the fertilized zygote being prepared for implantation (text labels read: 3a) the fertilized zygote is then removed from the petri dish for implantation. 3b) fertilized zygote). The last panel shows the fertilized zygote being implanted into the uterus (text label reads: 4) The zygote is then surgically implanted into the endometrium of the uterus. After successful implantation, the zygote should develop normally, as if it had been fertilized in the female’s oviducts). [Return to Figure 11.2].
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
male gamete (spermatozoon)
female gamete
Process of fertilization is complete and results in a single-celled diploid zygote with all the genetic instructions it needs to develop into a human.
assisted reproductive technology
A small piece of placenta is taken and tested to determine potential for birth differences
surgical puncture (using a needle) to remove amniotic fluid for sampling.

