110 17.5 The Parathyroid Glands
Learning Objectives
By the end of this section, you will be able to:
- Describe the location and structure of the parathyroid glands
- Describe the hormonal control of blood calcium levels
- Discuss the physiological response of parathyroid dysfunction
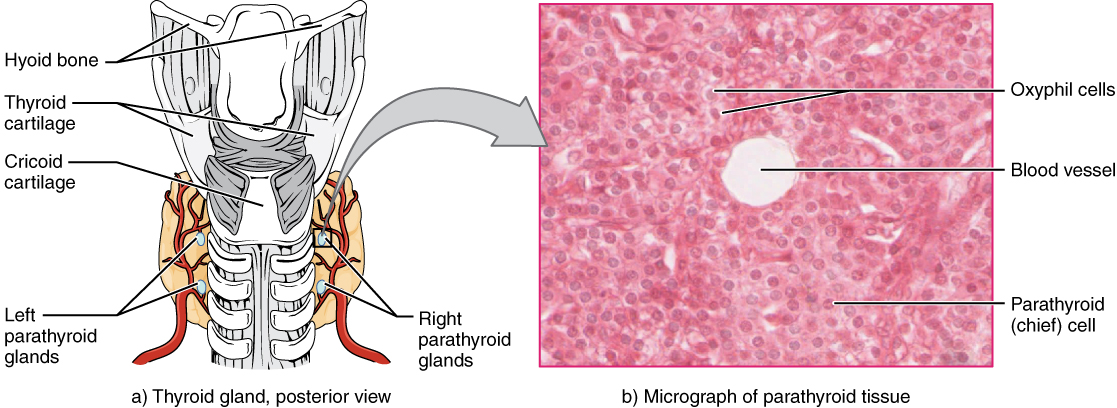
The parathyroid glands are tiny, round structures usually found embedded in the posterior surface of the thyroid gland (Figure 1). A thick connective tissue capsule separates the glands from the thyroid tissue. Most people have four parathyroid glands, but occasionally there are more in tissues of the neck or chest. The function of one type of parathyroid cells, the oxyphil cells, is not clear. The primary functional cells of the parathyroid glands are the chief cells. These epithelial cells produce and secrete the parathyroid hormone (PTH), the major hormone involved in the regulation of blood calcium levels.

View the University of Michigan WebScope at http://141.214.65.171/Histology/Endocrine%20System/217_HISTO_40X.svs/view.apml to explore the tissue sample in greater detail.
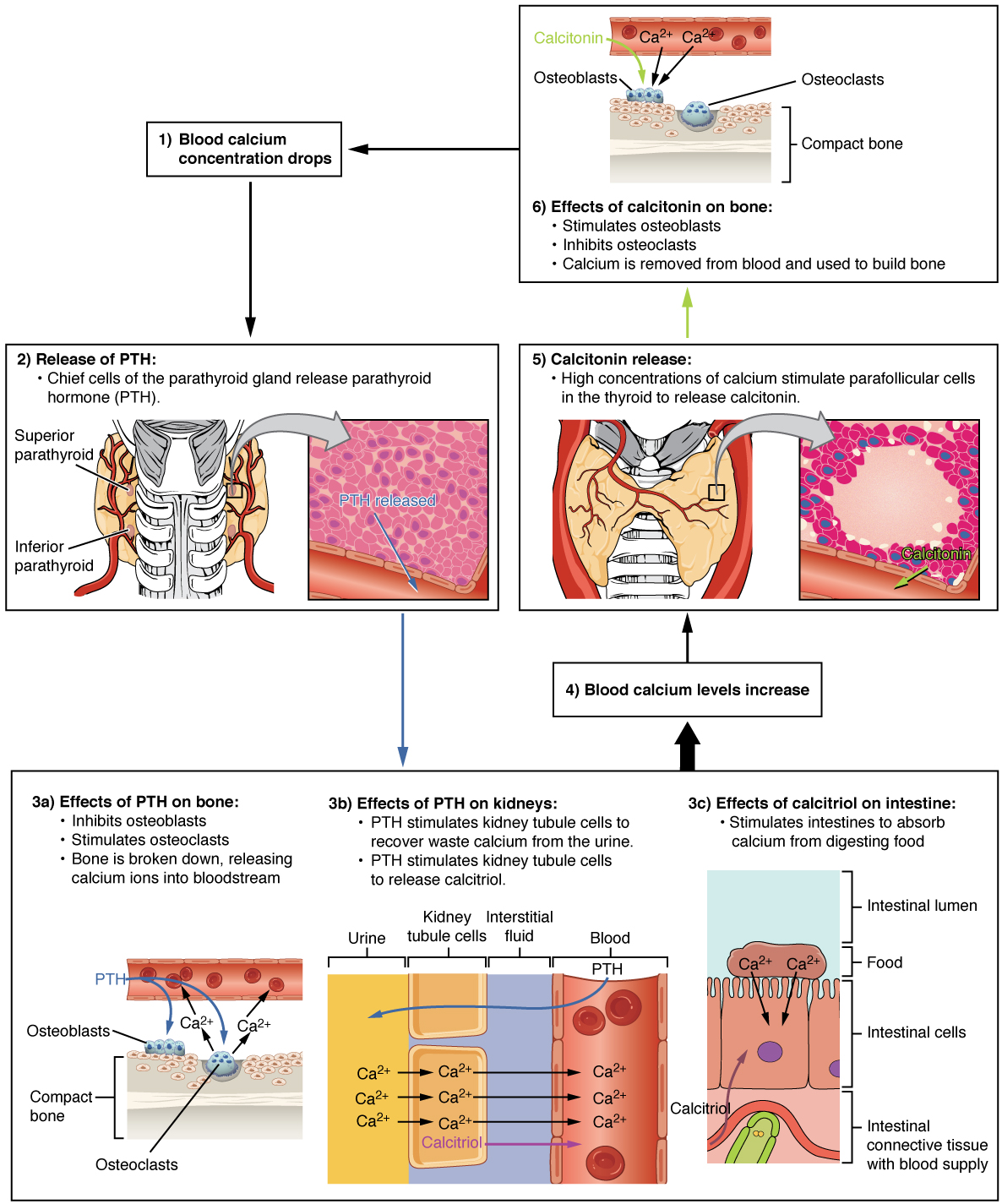
The parathyroid glands produce and secrete PTH, a peptide hormone, in response to low blood calcium levels (Figure 2). PTH secretion causes the release of calcium from the bones by stimulating osteoclasts, which secrete enzymes that degrade bone and release calcium into the interstitial fluid. PTH also inhibits osteoblasts, the cells involved in bone deposition, thereby sparing blood calcium. PTH causes increased reabsorption of calcium (and magnesium) in the kidney tubules from the urine filtrate. In addition, PTH initiates the production of the steroid hormone calcitriol (also known as 1,25-dihydroxyvitamin D), which is the active form of vitamin D3, in the kidneys. Calcitriol then stimulates increased absorption of dietary calcium by the intestines. A negative feedback loop regulates the levels of PTH, with rising blood calcium levels inhibiting further release of PTH.
Abnormally high activity of the parathyroid gland can cause hyperparathyroidism, a disorder caused by an overproduction of PTH that results in excessive calcium reabsorption from bone. Hyperparathyroidism can significantly decrease bone density, leading to spontaneous fractures or deformities. As blood calcium levels rise, cell membrane permeability to sodium is decreased, and the responsiveness of the nervous system is reduced. At the same time, calcium deposits may collect in the body’s tissues and organs, impairing their functioning.
In contrast, abnormally low blood calcium levels may be caused by parathyroid hormone deficiency, called hypoparathyroidism, which may develop following injury or surgery involving the thyroid gland. Low blood calcium increases membrane permeability to sodium, resulting in muscle twitching, cramping, spasms, or convulsions. Severe deficits can paralyze muscles, including those involved in breathing, and can be fatal.
When blood calcium levels are high, calcitonin is produced and secreted by the parafollicular cells of the thyroid gland. As discussed earlier, calcitonin inhibits the activity of osteoclasts, reduces the absorption of dietary calcium in the intestine, and signals the kidneys to reabsorb less calcium, resulting in larger amounts of calcium excreted in the urine.
Chapter Review
Calcium is required for a variety of important physiologic processes, including neuromuscular functioning; thus, blood calcium levels are closely regulated. The parathyroid glands are small structures located on the posterior thyroid gland that produce parathyroid hormone (PTH), which regulates blood calcium levels. Low blood calcium levels cause the production and secretion of PTH. In contrast, elevated blood calcium levels inhibit secretion of PTH and trigger secretion of the thyroid hormone calcitonin. Underproduction of PTH can result in hypoparathyroidism. In contrast, overproduction of PTH can result in hyperparathyroidism.
Review Questions
1. When blood calcium levels are low, PTH stimulates ________.
- urinary excretion of calcium by the kidneys
- a reduction in calcium absorption from the intestines
- the activity of osteoblasts
- the activity of osteoclasts
2. Which of the following can result from hyperparathyroidism?
- increased bone deposition
- fractures
- convulsions
- all of the above
Critical Thinking Questions
1. Describe the role of negative feedback in the function of the parathyroid gland.
2. Explain why someone with a parathyroid gland tumor might develop kidney stones.
Glossary
- hyperparathyroidism
- disorder caused by overproduction of PTH that results in abnormally elevated blood calcium
- hypoparathyroidism
- disorder caused by underproduction of PTH that results in abnormally low blood calcium
- parathyroid glands
- small, round glands embedded in the posterior thyroid gland that produce parathyroid hormone (PTH)
- parathyroid hormone (PTH)
- peptide hormone produced and secreted by the parathyroid glands in response to low blood calcium levels
Solutions
Answers for Review Questions
- D
- B
Answers for Critical Thinking Questions
- The production and secretion of PTH is regulated by a negative feedback loop. Low blood calcium levels initiate the production and secretion of PTH. PTH increases bone resorption, calcium absorption from the intestines, and calcium reabsorption by the kidneys. As a result, blood calcium levels begin to rise. This, in turn, inhibits the further production and secretion of PTH.
- A parathyroid gland tumor can prompt hypersecretion of PTH. This can raise blood calcium levels so excessively that calcium deposits begin to accumulate throughout the body, including in the kidney tubules, where they are referred to as kidney stones.


Feedback/Errata