Mental Health and Mental Illnesses
A client’s mental health refers to their emotional and psychological well-being that affects their day-to-day functioning. The World Health Organization (2014) defines mental health as a “state of well-being in which every individual realizes … [their] own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to … [their] community.” Mental health is often underscreened, which reveals a significant gap considering that stress is pervasive in society.
Clinical Tip
Mental health is a component of every person—a state of well-being that fluctuates throughout life.
Mental illness includes conditions such as depression, anxiety, addiction, schizophrenia, post-traumatic stress disorder, among others. By definition, mental illness is a disruption in everyday function, which means a person’s employment, relationships, and civil participation can all be impaired by mental illness.
It is important to assess a client’s mental health, and if present, mental illnesses. You want to begin this component of the assessment with a statement such as, “Mental health is an important part of our lives and so I ask all clients about their mental health and any concerns or illnesses they may have.”
See Table 2.5 for a selection of questions and statements that you may ask clients to elicit data about their mental health. Note also that there are many other factors that influence mental health, such as violence and trauma, which are addressed under the next section, Functional Health.
| Question or Statement | Considerations |
|
Tell me about your mental health.
|
This question broadly focuses on health and invites a dialogue. The statement should not be asked in isolation or as a one-off question, as societally and culturally there are different meanings of what constitutes mental health and a client may not identify themselves as having mental health issues. If a client responds “Good,” consider probing a bit further with “Tell me about how so,” or “What do you mean by good?” which allows them to respond in more depth.
|
|
Tell me about the stress in your life.
|
Stress, by and large, is a relatable term that many clients have experienced and that is something they are likely more comfortable talking about than more difficult health issues because it is so ubiquitous. It’s important to be attentive to the client’s language and consider terms they may use, such as “extreme stress,” “severe stress,” “unmanaged stressed,” or “debilitating stress,” as these may indicate an underlying mental health issue or stress that requires intervention.
|
|
How does stress affect you?
|
Understanding how stress affects the client provides insight into the mental, physical, and social impact on them. You may need to probe about how stress affects the client physically, mentally, and socially.
|
|
How do you cope with this stress? (may include positive or negative coping strategies.)
|
This question invites discussion about coping strategies. It is important to be attentive to any self-harm coping strategies such as substance abuse, isolation/disengagement, food restriction, purging, cutting, compulsions, and phobias as these could indicate a mental health issue. Additionally, you want to use a strength-based approach to your assessment and facilitate the client’s capacity to identify and use positive coping strategies.
|
|
Have you experienced a loss in your life or a death that is meaningful to you?
|
Inviting discussions about loss and grief could be helpful for clients who have not had an outlet to speak openly about their emotions and the impact. Allowing for loss and grief to be talked about and understanding to what degree grief is affecting health is an important aspect of a mental health assessment.
|
|
Have you had a recent breakup or divorce?
|
Estrangement, emancipation, disruption, or severance of a relationship are not necessarily an indication of a mental illness. However, a pattern in relational disruption may indicate underlying issues such as, but not limited to, ineffective relationship skills, poor coping, or low self-esteem. Assess further if the client reports a breakup or divorce.
|
|
Have you recently lost your job or been off work?
|
Many clients define themselves through their work, and job loss can be disruptive to everyday life. Understanding the meaning of loss of employment is an important dimension of mental health.
|
|
Have you recently had any legal issues?
|
Asking about legal issues should be purposeful, not invasive. For example, a pattern of driving under the influence or possession of illicit drugs could indicate an underlying addiction. Use your clinical judgment when asking questions about legal issues, and be sure to convey an unconditionally accepting way of being with the client.
|
|
Have you purchased any weapons?
|
The purchase of weapons by itself is not an indication of mental illness. In Canada, some people enjoy hunting and other recreational activities that involve weapons. However, the purchase of weapons in response to threats to personal safety or to feelings of self-harm could indicate an underlying mental illness.
|
Table 2.5: Mental health and illness assessment
If the client identifies that they have a mental illness, you want to assess the onset of it, and the associated impacts, treatments, hospitalizations, complications, and disabilities. Here are some questions and statements that you may use to elicit more information about the client’s well-being in light of having a mental illness:
- How does that illness affect you?
- How does that illness affect your day-to-day life?
- How do you cope with the illness?
- What resources do you draw upon to cope with your illness?
- When were you diagnosed?
- Who was the treating practitioner?
- Have you been hospitalized? Where?
- Tell me about your treatment (e.g., medications, counselling).
- Have you experienced any complications?
- Has the illness resulted in a disability?
- Do you have any concerns that have not been addressed related to your illness?
Take Action
Health promotion is a vital component of all mental health assessments. You should collaborate with the client on how to develop healthy behaviours to promote their mental health. Also, chronic and sustained stress is an influencing factor of certain diseases such as heart disease and cancer. Furthermore, some coping behaviours related to stress, such as using alcohol and cigarettes, can exacerbate the onset of these diseases. Thus, assessment and collaborative interventions are important.
You also need to be attentive to critical findings that require intervention. For example, if a client talks about feeling despair, hopeless, or depressed, it is important to screen for suicidal thinking. You should begin with a general probing question, such as “Have you ever felt like hurting yourself?” If the client responds with a “yes,” then you should progress with more exploratory and specific questions that assess the immediacy and the intensity of the feelings. For example, you may say, “Tell me more about that feeling. Have you been thinking about hurting yourself today? Have you put together a plan to hurt yourself?”
Points of Consideration
- The client most at risk is one who has a specific plan about self-harm, specifying how and when, particularly if it is within 48 hours. The age of the client is not a factor in this determination. Under these circumstances, you should not leave the client alone. You should collaborate with them about an immediate emergency plan of care.
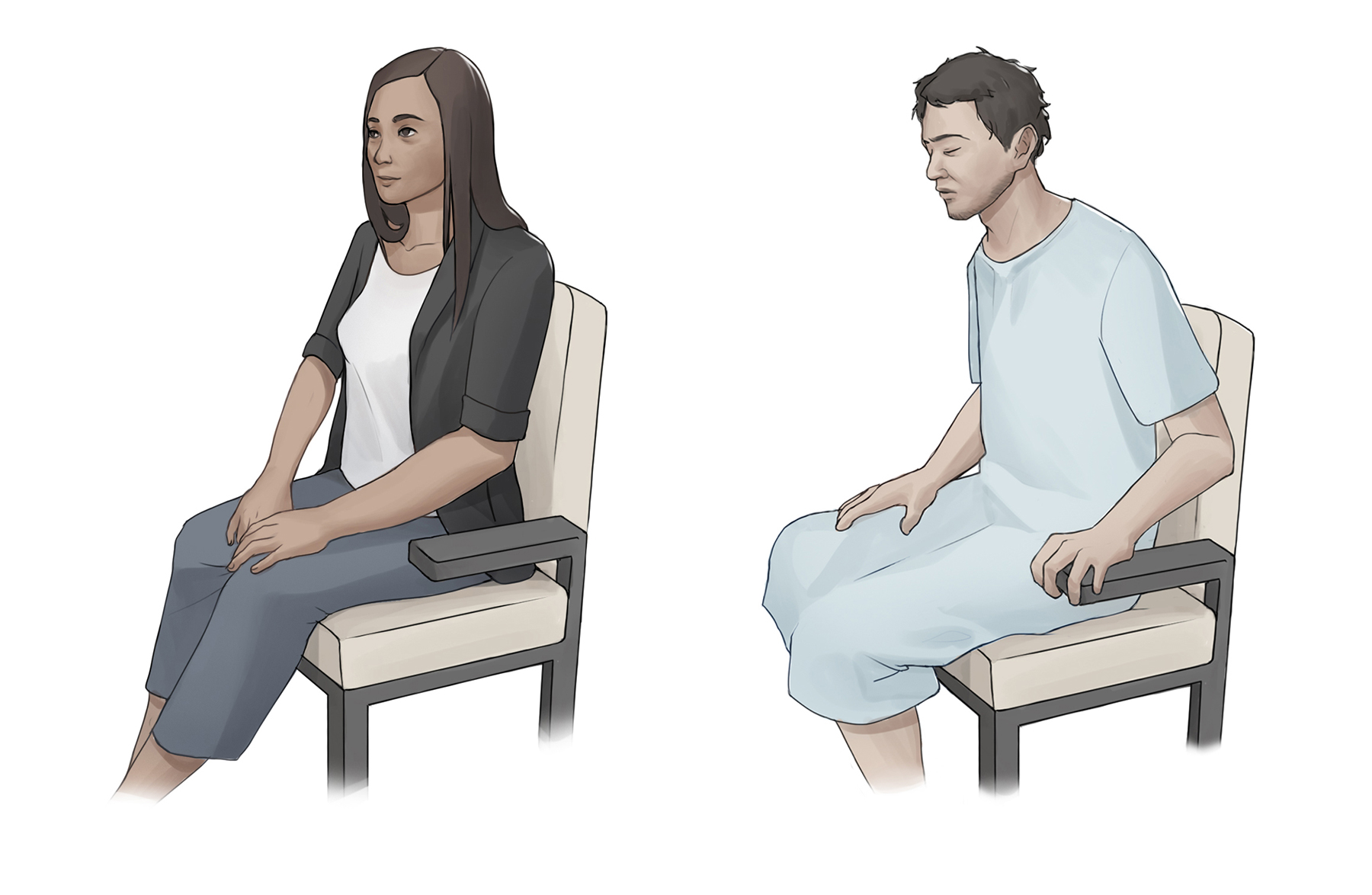
- It is important that you not make assumptions about a client’s mental health based on their appearance, facial expression, and capacity to function in their daily life. For example, you shouldn’t assume that a person dressed nicely with a smile or neutral expression is mentally healthy or that a dishevelled person in a gown (see Figure 2.6) has mental health issues.
An approach or philosophy that focuses on empowerment, views the client as resourceful, and emphasizes their strengths, but does not ignore their challenges.
Behaviour of accepting the client, respecting their right to self-determination, and supporting them regardless of our perception of what they say or do.
To worsen or increase in severity
Interventions that are developed with the client, not for the client.

