8.2 Anatomy of Selected Synovial Joints
Learning Objectives
By the end of this section, you will be able to:
- Describe the bones that articulate together to form selected synovial joints
- Discuss the movements available at each joint
- Describe the structures that support and prevent excess movements at each joint
Each synovial joint of the body is specialized to perform certain movements. The movements that are allowed are determined by the structural classification for each joint. For example, a multiaxial ball-and-socket joint has much more mobility than a uniaxial hinge joint. However, the ligaments and muscles that support a joint may place restrictions on the total range of motion available. Thus, the ball-and-socket joint of the shoulder has little in the way of ligament support, which gives the shoulder a very large range of motion. In contrast, movements at the hip joint are restricted by strong ligaments, which reduce its range of motion but confer stability during standing and weight bearing.
This section will examine the anatomy of selected synovial joints of the body. Anatomical names for most joints are derived from the names of the bones that articulate at that joint, although some joints, such as the elbow, hip, and knee joints are exceptions to this general naming scheme.
Articulations of the Vertebral Column
In addition to being held together by the intervertebral discs, adjacent vertebrae also articulate with each other at synovial joints formed between the superior and inferior articular processes called zygapophysial joints (facet joints). These are plane joints that provide for only limited motions between the vertebrae. The orientation of the articular processes at these joints varies in different regions of the vertebral column and serves to determine the types of motions available in each vertebral region. The cervical and lumbar regions have the greatest ranges of motions.
The articulations formed between the skull, the atlas (C1 vertebra), and the axis (C2 vertebra) differ from the articulations in other vertebral areas and play important roles in movement of the head. The atlanto-occipital joint is formed by the articulations between the superior articular processes of the atlas and the occipital condyles on the base of the skull. This articulation has a pronounced U-shaped curvature, oriented along the anterior-posterior axis. This allows the skull to rock forward and backward, producing flexion and extension of the head. This moves the head up and down, as when shaking your head “yes.”
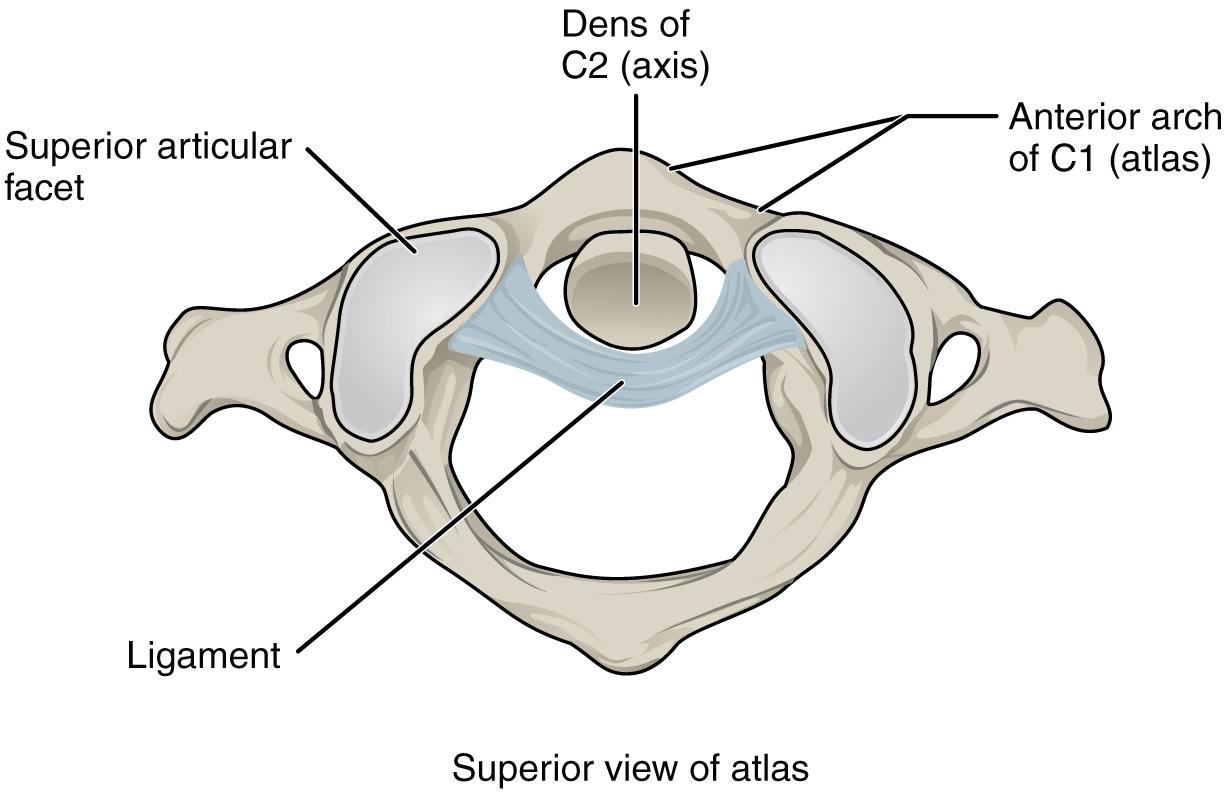
The atlantoaxial joint, between the atlas and axis, consists of three articulations. The paired superior articular processes of the axis articulate with the inferior articular processes of the atlas. These articulating surfaces are relatively flat and oriented horizontally. The third articulation is the pivot joint formed between the dens, which projects upward from the body of the axis, and the inner aspect of the anterior arch of the atlas (Figure 8.4). A strong ligament passes posterior to the dens to hold it in position against the anterior arch. These articulations allow the atlas to rotate on top of the axis, moving the head toward the right or left, as when shaking your head “no.”
Shoulder Joint
The shoulder joint is called the glenohumeral joint. This is a ball-and-socket joint formed by the articulation between the head of the humerus and the glenoid cavity of the scapula (Figure 8.5). This joint has the largest range of motion of any joint in the body. However, this freedom of movement is due to the lack of structural support and thus the increased mobility is offset by a loss of stability.
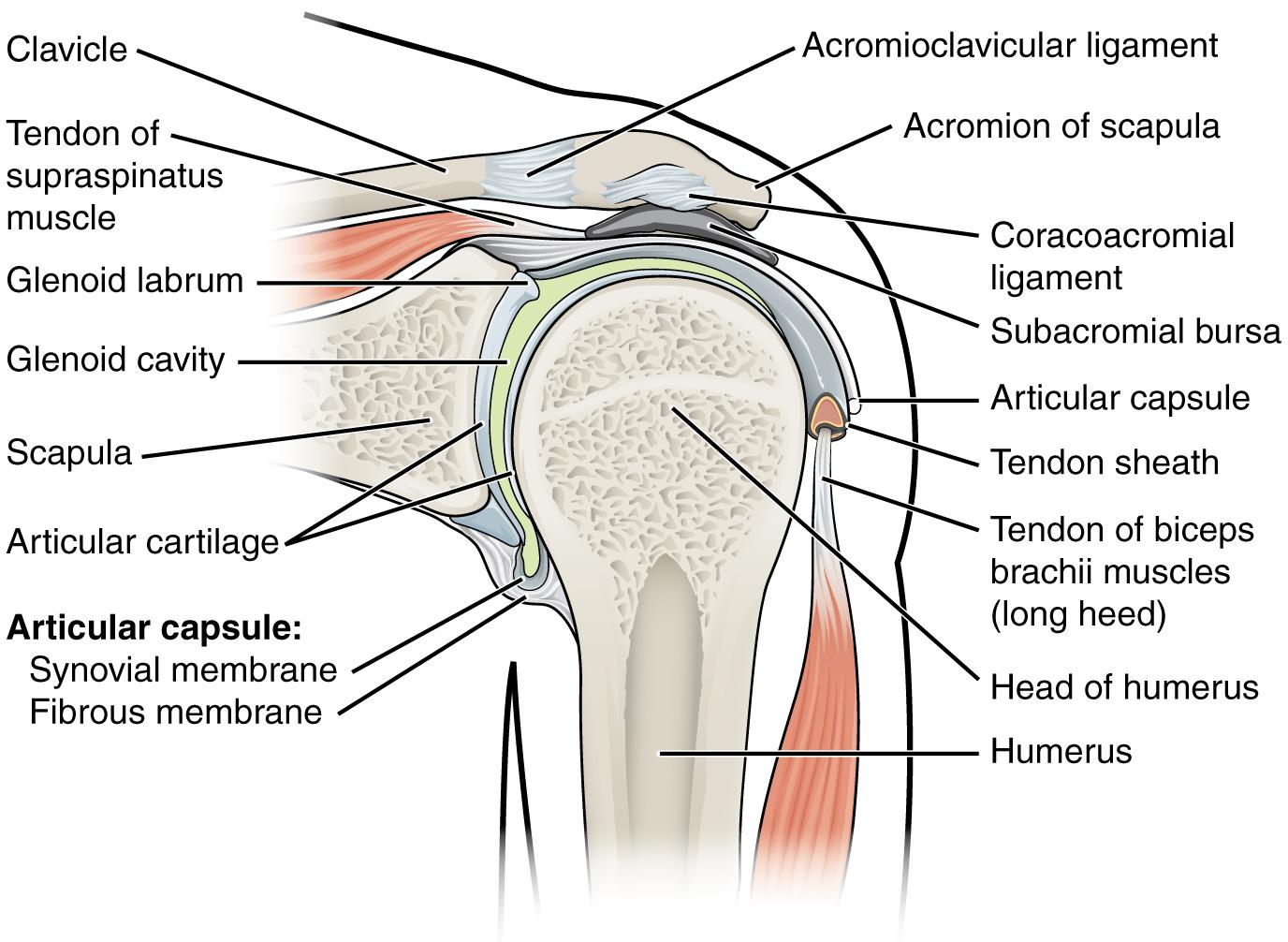
The large range of motions at the shoulder joint is provided by the articulation of the large, rounded humeral head with the small and shallow glenoid cavity, which is only about one third of the size of the humeral head. The socket formed by the glenoid cavity is deepened slightly by a small lip of fibrocartilage called the glenoid labrum, which extends around the outer margin of the cavity. The articular capsule that surrounds the glenohumeral joint is relatively thin and loose to allow for large motions of the upper limb. Some structural support for the joint is provided by thickenings of the articular capsule wall that form intrinsic ligaments. These include the coracohumeral ligament, running from the coracoid process of the scapula to the anterior humerus, and three ligaments, each called a glenohumeral ligament, located on the anterior side of the articular capsule. These ligaments help to strengthen the superior and anterior capsule walls.
However, the primary support for the shoulder joint is provided by muscles crossing the joint, particularly the four rotator cuff muscles. These muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) arise from the scapula and attach to the greater or lesser tubercles of the humerus. As these muscles cross the shoulder joint, their tendons encircle the head of the humerus and become fused to the walls of the articular capsule. The thickening of the capsule formed by the fusion of these four muscle tendons is called the rotator cuff. The subacromial bursa helps to prevent friction between the rotator cuff muscle tendons and the scapula as these tendons cross the glenohumeral joint. In addition to their individual actions of moving the upper limb, the rotator cuff muscles also serve to hold the head of the humerus in position within the glenoid cavity. By constantly adjusting their strength of contraction to resist forces acting on the shoulder, these muscles serve as “dynamic ligaments” and thus provide the primary structural support for the glenohumeral joint.
Injuries to the shoulder joint are common. Repetitive use of the upper limb, particularly in abduction such as during throwing, swimming, or racquet sports, may lead to acute or chronic inflammation of the bursa or muscle tendons, a tear of the glenoid labrum, or degeneration or tears of the rotator cuff. Because the humeral head is strongly supported by muscles and ligaments around its anterior, superior, and posterior aspects, most dislocations of the humerus occur in an inferior direction. This can occur when force is applied to the humerus when the upper limb is fully abducted, as when diving to catch a baseball and landing on your hand or elbow.
Interactive Link
What this video for a tutorial on the anatomy of the shoulder joint. What movements are available at the shoulder joint?
Elbow Joint
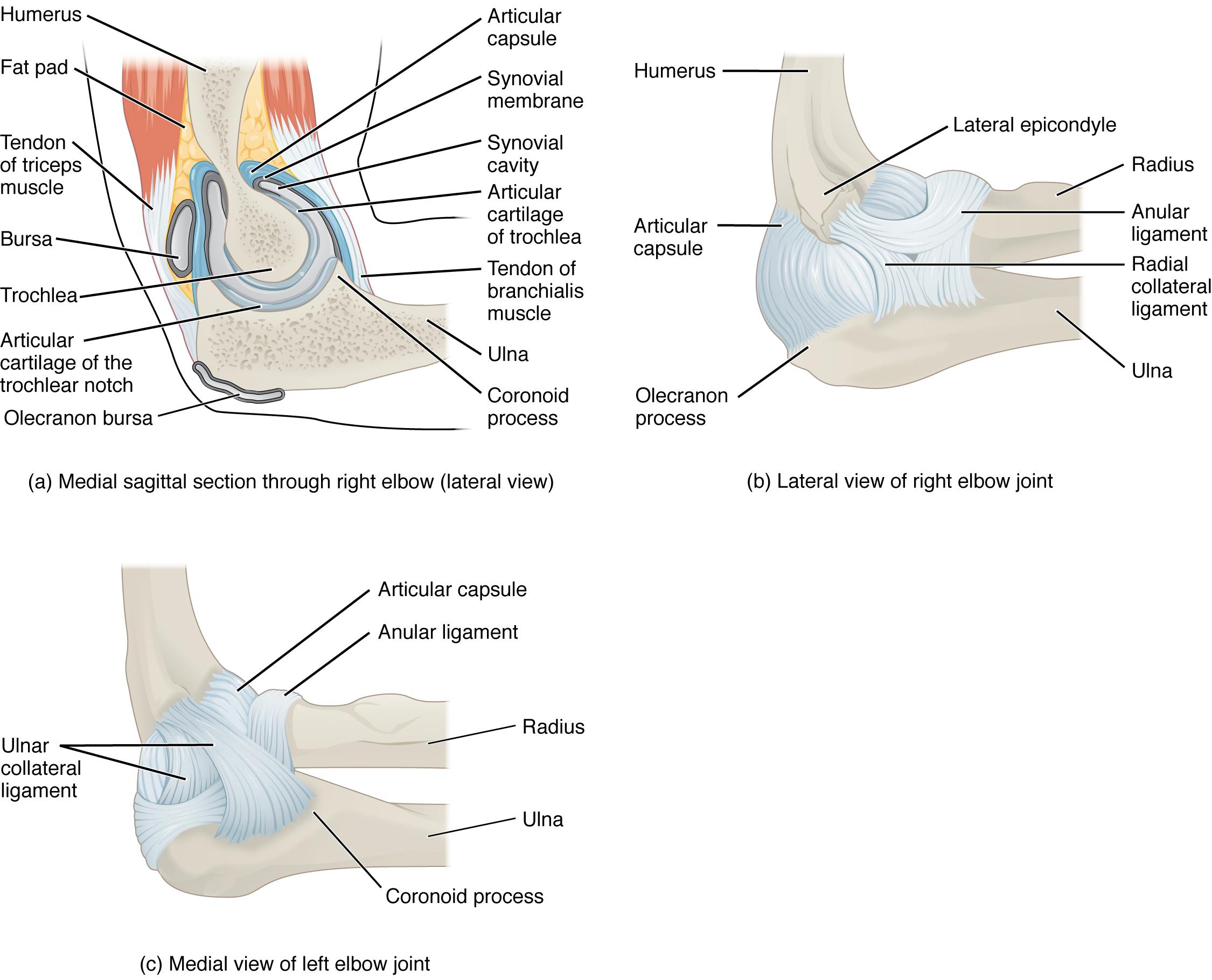
The elbow joint is a uniaxial hinge joint formed by the humeroulnar joint, the articulation between the trochlea of the humerus and the trochlear notch of the ulna. Also associated with the elbow are the humeroradial joint and the proximal radioulnar joint. All three of these joints are enclosed within a single articular capsule (Figure 8.6).
The articular capsule of the elbow is thin on its anterior and posterior aspects, but is thickened along its outside margins by strong intrinsic ligaments. These ligaments prevent side-to-side movements and hyperextension. On the medial side is the triangular ulnar collateral ligament. This arises from the medial epicondyle of the humerus and attaches to the medial side of the proximal ulna. The strongest part of this ligament is the anterior portion, which resists hyperextension of the elbow. The ulnar collateral ligament may be injured by frequent, forceful extensions of the forearm, as is seen in baseball pitchers.
The lateral side of the elbow is supported by the radial collateral ligament. This arises from the lateral epicondyle of the humerus and then blends into the lateral side of the annular ligament. The annular ligament encircles the head of the radius. This ligament supports the head of the radius as it articulates with the radial notch of the ulna at the proximal radioulnar joint. This is a pivot joint that allows for rotation of the radius during supination and pronation of the forearm.
Interactive Link
Watch this animation to learn more about the anatomy of the elbow joint. Which structures provide the main stability for the elbow?
Hip Joint
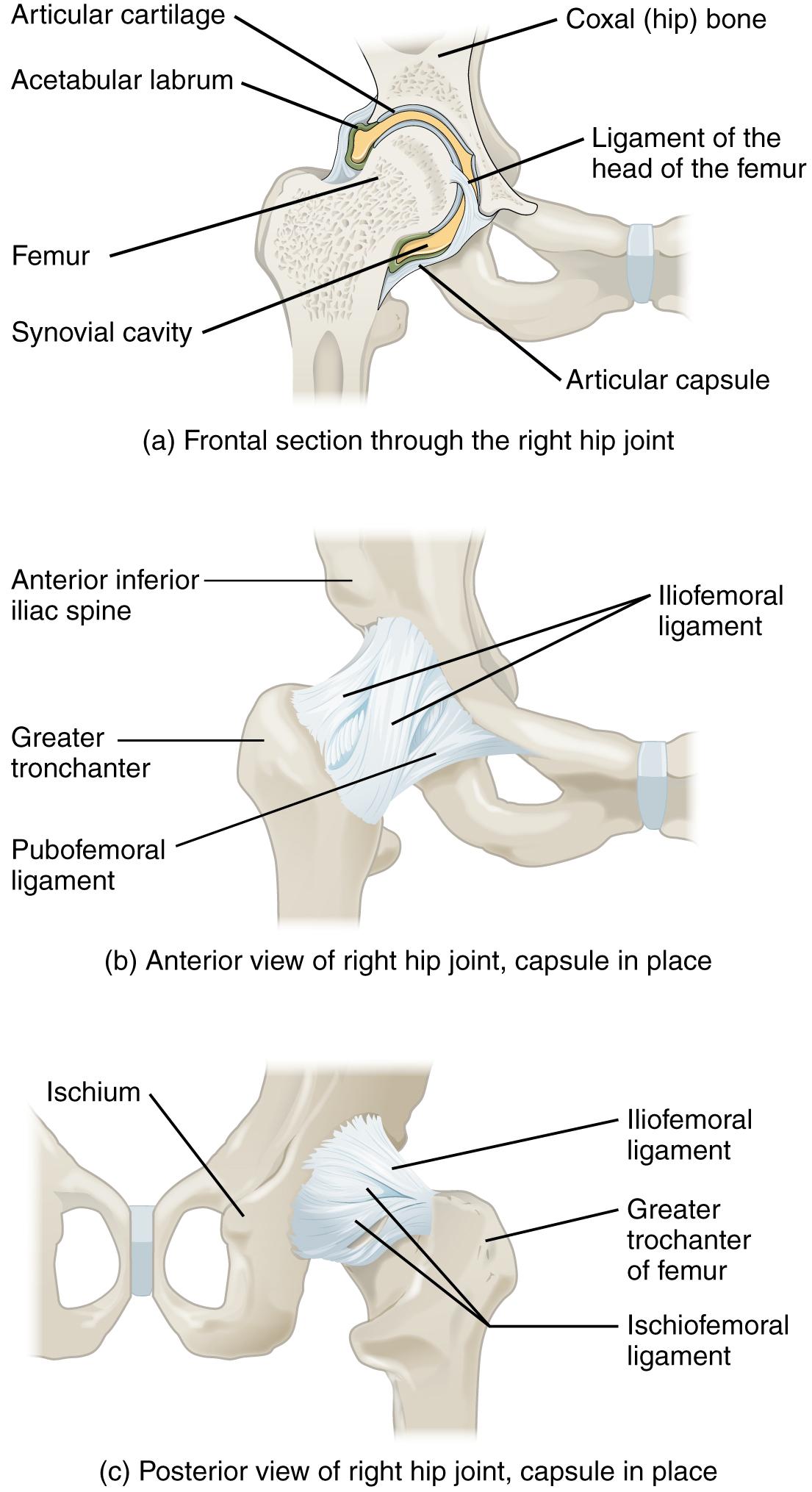
The hip joint is a multiaxial ball-and-socket joint between the head of the femur and the acetabulum of the hip bone (Figure 8.7). The hip carries the weight of the body and thus requires strength and stability during standing and walking. For these reasons, its range of motion is more limited than at the shoulder joint.
The acetabulum is the socket portion of the hip joint. This space is deep and has a large articulation area for the femoral head, thus giving stability and weight bearing ability to the joint. The acetabulum is further deepened by the acetabular labrum, a fibrocartilage lip attached to the outer margin of the acetabulum. The surrounding articular capsule is strong, with several thickened areas forming intrinsic ligaments. These ligaments arise from the hip bone, at the margins of the acetabulum, and attach to the femur at the base of the neck. The ligaments are the iliofemoral ligament, pubofemoral ligament, and ischiofemoral ligament, all of which spiral around the head and neck of the femur. These ligaments stabilize the hip joint and allow you to maintain an upright standing position with only minimal muscle contraction. Inside of the articular capsule, the ligament of the head of the femur (ligamentum teres) spans between the acetabulum and femoral head. This intracapsular ligament is normally slack and does not provide any significant joint support, but it does provide a pathway for an important artery that supplies the head of the femur.
Interactive Link
Watch this video for a tutorial on the anatomy of the hip joint. What is a possible consequence following a fracture of the femoral neck within the capsule of the hip joint?
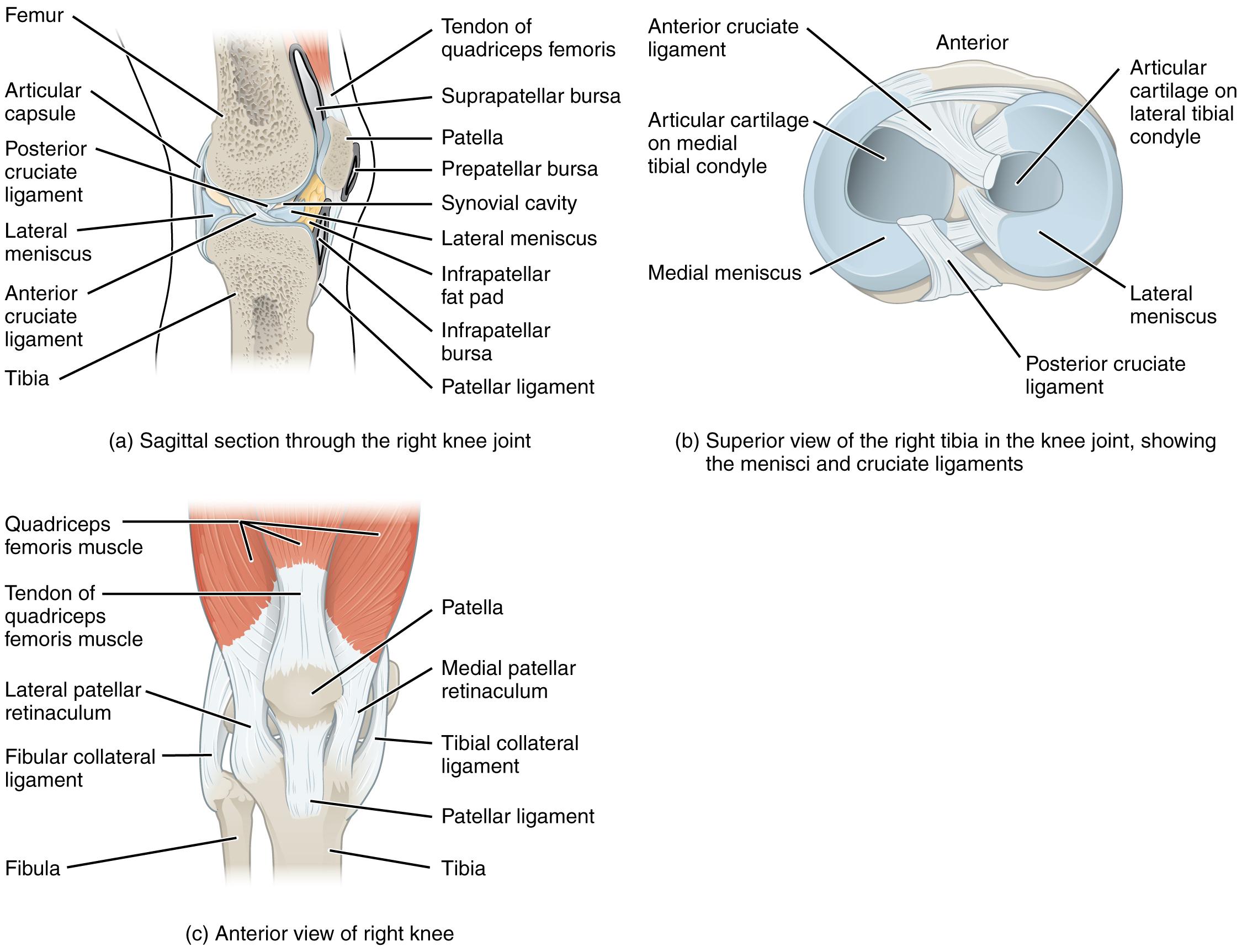
Knee Joint
The knee joint is the largest joint of the body (Figure 8.8). It actually consists of three articulations. The femoropatellar joint is found between the patella and the distal femur. The medial tibiofemoral joint and lateral tibiofemoral joint are located between the medial and lateral condyles of the femur and the medial and lateral condyles of the tibia. All of these articulations are enclosed within a single articular capsule. The knee functions as a hinge joint, allowing flexion and extension of the leg. The knee is well constructed for weight bearing in its extended position, but is vulnerable to injuries associated with hyperextension, twisting, or blows to the medial or lateral side of the joint, particularly while weight bearing.
At the femoropatellar joint, the patella slides vertically within a groove on the distal femur. The patella is a sesamoid bone incorporated into the tendon of the quadriceps femoris muscle, the large muscle of the anterior thigh. The patella serves to protect the quadriceps tendon from friction against the distal femur. Continuing from the patella to the anterior tibia just below the knee is the patellar ligament. Acting via the patella and patellar ligament, the quadriceps femoris is a powerful muscle that acts to extend the leg at the knee. It also serves as a “dynamic ligament” to provide very important support and stabilization for the knee joint.
The medial and lateral tibiofemoral joints are the articulations between the rounded condyles of the femur and the relatively flat condyles of the tibia. During flexion and extension motions, the condyles of the femur both roll and glide over the surfaces of the tibia. The rolling action produces flexion or extension, while the gliding action serves to maintain the femoral condyles centered over the tibial condyles, thus ensuring maximal bony, weight-bearing support for the femur in all knee positions.
Located between the articulating surfaces of the femur and tibia are two articular discs, the medial meniscus and lateral meniscus (see Figure 8.8b). Each is a C-shaped fibrocartilage structure that is thin along its inside margin and thick along the outer margin. They are attached to their tibial condyles, but do not attach to the femur. The menisci provide padding between the bones and help to fill the gap between the round femoral condyles and flattened tibial condyles.
The knee joint has multiple ligaments that provide support, particularly in the extended position (see Figure 8.8c). Outside of the articular capsule, located at the sides of the knee, are two extrinsic ligaments. The fibular collateral ligament (lateral collateral ligament) is on the lateral side and spans from the lateral epicondyle of the femur to the head of the fibula. The tibial collateral ligament (medial collateral ligament) of the medial knee runs from the medial epicondyle of the femur to the medial tibia. As it crosses the knee, the tibial collateral ligament is firmly attached on its deep side to the articular capsule and to the medial meniscus. In the fully extended knee position, both collateral ligaments are taut (tight), thus serving to stabilize and support the extended knee and preventing side-to-side or rotational motions between the femur and tibia.
The articular capsule of the posterior knee is thickened by intrinsic ligaments that help to resist knee hyperextension. Inside the knee are two ligaments, the anterior cruciate ligament and posterior cruciate ligament. These ligaments are anchored inferiorly to the tibia at the intercondylar eminence, the roughened area between the tibial condyles. The cruciate ligaments are named for whether they are attached anteriorly or posteriorly to this tibial region. Each ligament runs diagonally upward to attach to the inner aspect of a femoral condyle. The cruciate ligaments are named for the X-shape formed as they pass each other (cruciate means “cross”). The posterior cruciate ligament is the stronger ligament. It serves to support the knee when it is flexed and weight bearing, as when walking downhill. In this position, the posterior cruciate ligament prevents the femur from sliding anteriorly off the top of the tibia. The anterior cruciate ligament becomes tight when the knee is extended, and thus resists hyperextension.
Disorders of the…
Joints
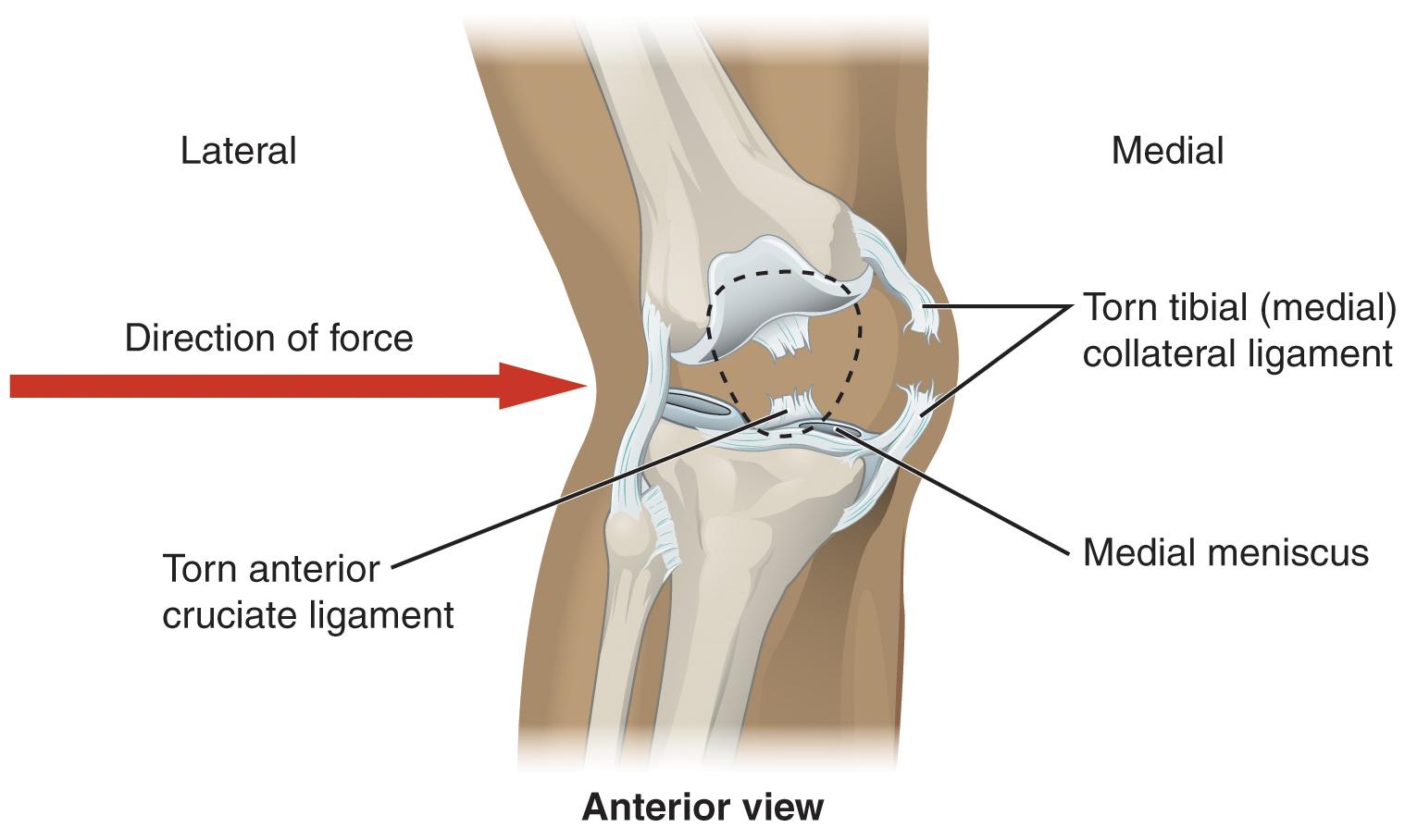
Injuries to the knee are common. Since this joint is primarily supported by muscles and ligaments, injuries to any of these structures will result in pain or knee instability. Injury to the posterior cruciate ligament (PCL) occurs when the knee is flexed and the tibia is driven posteriorly, such as falling and landing on the tibial tuberosity or hitting the tibia on the dashboard when not wearing a seatbelt during an automobile accident. More commonly, injuries occur when forces are applied to the extended knee, particularly when the foot is planted and unable to move. Anterior cruciate ligament (ACL) injuries can result with a forceful blow to the anterior knee, producing hyperextension, or when a runner makes a quick change of direction that produces both twisting and hyperextension of the knee.
A worse combination of injuries can occur with a hit to the lateral side of the extended knee (Figure 8.9). A moderate blow to the lateral knee will cause the medial side of the joint to open, resulting in stretching or damage to the medial collateral ligament (MCL). Because the medial meniscus is attached to the medial collateral ligament, a stronger blow can tear the ligament and also damage the medial meniscus. This is one reason that the medial meniscus is 20 times more likely to be injured than the lateral meniscus. A powerful blow to the lateral knee produces a “terrible triad” injury, in which there is a sequential injury to the medial collateral ligament, medial meniscus, and anterior cruciate ligament.
Arthroscopic surgery has greatly improved the surgical treatment of knee injuries and reduced subsequent recovery times. This procedure involves a small incision and the insertion into the joint of an arthroscope, a pencil-thin instrument that allows for visualization of the joint interior. Small surgical instruments are also inserted via additional incisions. These tools allow a surgeon to remove or repair a torn meniscus or to reconstruct a ruptured cruciate ligament. The current method for anterior cruciate ligament replacement involves using a portion of the patellar ligament. Holes are drilled into the cruciate ligament attachment points on the tibia and femur, and the patellar ligament graft, with small areas of attached bone still intact at each end, is inserted into these holes. The bone-to-bone sites at each end of the graft heal rapidly and strongly, thus enabling a rapid recovery.
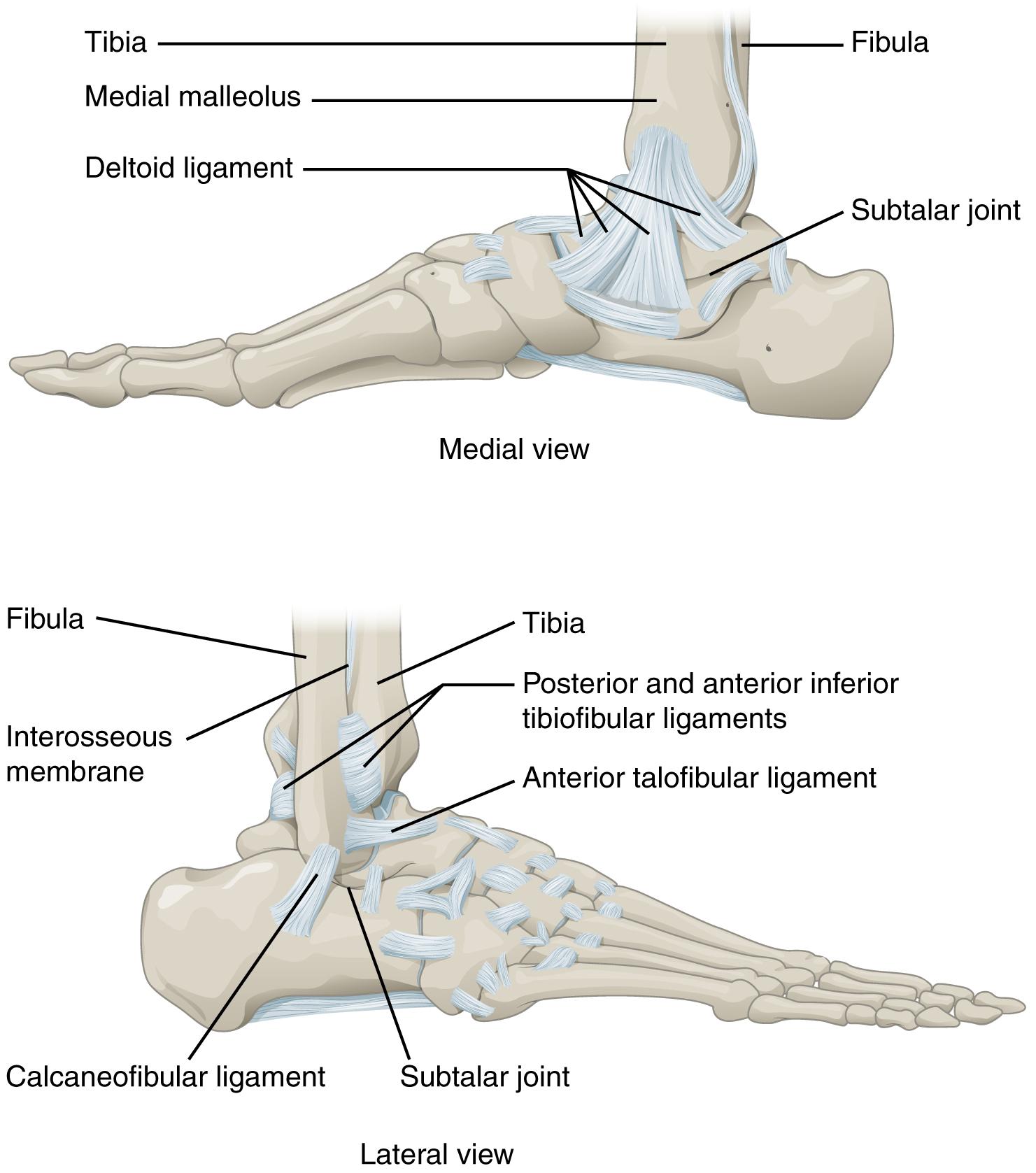
Ankle and Foot Joints
The ankle is formed by the talocrural joint (Figure 8.10). It consists of the articulations between the talus bone of the foot and the distal ends of the tibia and fibula of the leg (crural = “leg”). The superior aspect of the talus bone is square-shaped and has three areas of articulation. The top of the talus articulates with the inferior tibia. This is the portion of the ankle joint that carries the body weight between the leg and foot. The sides of the talus are firmly held in position by the articulations with the medial malleolus of the tibia and the lateral malleolus of the fibula, which prevent any side-to-side motion of the talus. The ankle is thus a uniaxial hinge joint that allows only for dorsiflexion and plantar flexion of the foot.
Additional joints between the tarsal bones of the posterior foot allow for the movements of foot inversion and eversion. Most important for these movements is the subtalar joint, located between the talus and calcaneus bones. The joints between the talus and navicular bones and the calcaneus and cuboid bones are also important contributors to these movements. All of the joints between tarsal bones are plane joints. Together, the small motions that take place at these joints all contribute to the production of inversion and eversion foot motions.
Like the hinge joints of the elbow and knee, the talocrural joint of the ankle is supported by several strong ligaments located on the sides of the joint. These ligaments extend from the medial malleolus of the tibia or lateral malleolus of the fibula and anchor to the talus and calcaneus bones. Since they are located on the sides of the ankle joint, they allow for dorsiflexion and plantar flexion of the foot. They also prevent abnormal side-to-side and twisting movements of the talus and calcaneus bones during eversion and inversion of the foot. On the medial side is the broad deltoid ligament. The deltoid ligament supports the ankle joint and also resists excessive eversion of the foot. The lateral side of the ankle has several smaller ligaments. These include the anterior talofibular ligament and the posterior talofibular ligament, both of which span between the talus bone and the lateral malleolus of the fibula, and the calcaneofibular ligament, located between the calcaneus bone and fibula. These ligaments support the ankle and also resist excess inversion of the foot.
Interactive Link
Watch this video for a tutorial on the anatomy of the ankle joint. What are the three ligaments found on the lateral side of the ankle joint?
Disorders of the…
Joints
The ankle is the most frequently injured joint in the body, with the most common injury being an inversion ankle sprain. A sprain is the stretching or tearing of the supporting ligament. Excess inversion causes the talus bone to tilt laterally, thus damaging the ligaments on the lateral side of the ankle. THe anterior talofibular ligament (ATFL) is most commonly injured, followed by the calcaneofibular ligament (CFL). In severe inversion injuries, the forceful lateral movement of the talus not only ruptures the lateral ankle ligaments, but also fractures the distal fibula.
Above the ankle, the distal ends of the tibia and fibula are united by a strong syndesmosis formed by the interosseous membrane and ligaments at the distal tibiofibular joint. These connections prevent separation between the distal ends of the tibia and fibula and maintain the talus locked into position between the medial malleolus and lateral malleolus. Injuries that produce a lateral twisting of the leg on top of the planted foot can result in stretching or tearing of the tibiofibular ligaments, producing a syndesmotic ankle sprain or “high ankle sprain.”
Most ankle sprains can be treated using the PRICE technique: Protect, Rest, Ice, Compression, and Elevation. Increasing joint stability using a brace may be required for a period of time. More severe injuries involving ligament tears or bone fractures may require surgery.

