22.2. The Kidneys and Osmoregulatory Organs
Learning Objectives
By the end of this section, you will be able to:
- Explain how the kidneys serve as the main osmoregulatory organs in mammalian systems
- Describe the structure of the kidneys and the functions of the parts of the kidney
- Describe how the nephron is the functional unit of the kidney and explain how it actively filters blood and generates urine
- Detail the three steps in the formation of urine: glomerular filtration, tubular reabsorption, and tubular secretion
Although the kidneys are the major osmoregulatory organ, the skin and lungs also play a role in the process. Water and electrolytes are lost through sweat glands in the skin, which helps moisturize and cool the skin surface, while the lungs expel a small amount of water in the form of mucous secretions and via evaporation of water vapor.
Kidneys: The Main Osmoregulatory Organ
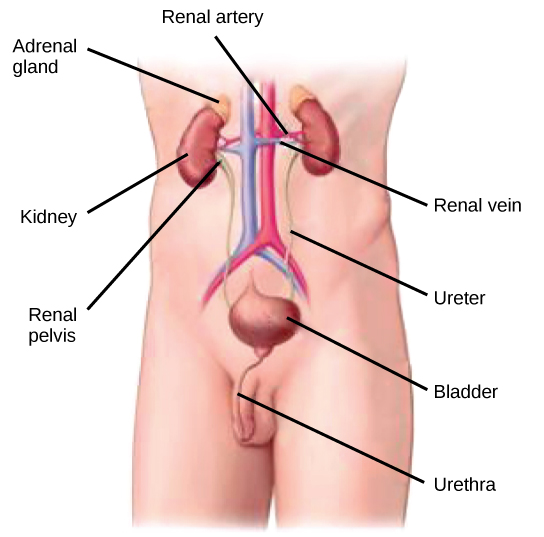
The kidneys, illustrated in Figure 22.4, are a pair of bean-shaped structures that are located just below and posterior to the liver in the peritoneal cavity. The adrenal glands sit on top of each kidney and are also called the suprarenal glands. Kidneys filter blood and purify it. All the blood in the human body is filtered many times a day by the kidneys; these organs use up almost 25 percent of the oxygen absorbed through the lungs to perform this function. Oxygen allows the kidney cells to efficiently manufacture chemical energy in the form of ATP through aerobic respiration. The filtrate coming out of the kidneys is called urine.
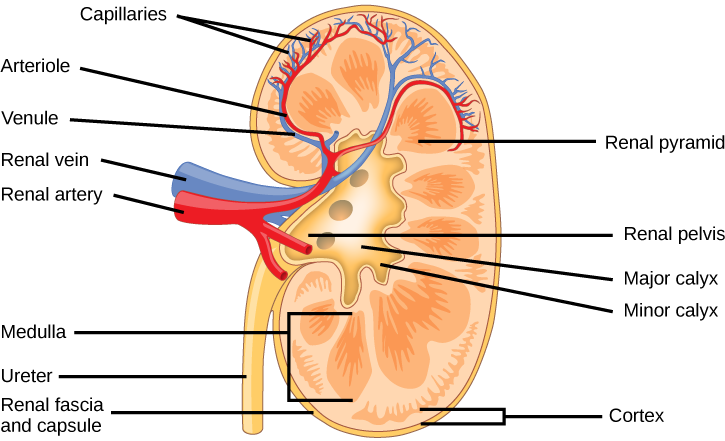
Kidney Structure
Externally, the kidneys are surrounded by three layers, illustrated in Figure 22.5. The outermost layer is a tough connective tissue layer called the renal fascia. The second layer is called the perirenal fat capsule, which helps anchor the kidneys in place. The third and innermost layer is the renal capsule. Internally, the kidney has three regions—an outer cortex, a medulla in the middle, and the renal pelvis in the region called the hilum of the kidney. The hilum is the concave part of the bean-shape where blood vessels and nerves enter and exit the kidney; it is also the point of exit for the ureters. The renal cortex is granular due to the presence of nephrons—the functional unit of the kidney. The medulla consists of multiple pyramidal tissue masses, called the renal pyramids. In between the pyramids are spaces called renal columns through which the blood vessels pass. The tips of the pyramids, called renal papillae, point toward the renal pelvis. There are, on average, eight renal pyramids in each kidney. The renal pyramids along with the adjoining cortical region are called the lobes of the kidney. The renal pelvis leads to the ureter on the outside of the kidney. On the inside of the kidney, the renal pelvis branches out into two or three extensions called the major calyces, which further branch into the minor calyces. The ureters are urine-bearing tubes that exit the kidney and empty into the urinary bladder.
Which of the following statements about the kidney is false?
- The renal pelvis drains into the ureter.
- The renal pyramids are in the medulla.
- The cortex covers the capsule.
- Nephrons are in the renal cortex.
Because the kidney filters blood, its network of blood vessels is an important component of its structure and function. The arteries, veins, and nerves that supply the kidney enter and exit at the renal hilum. Renal blood supply starts with the branching of the aorta into the renal arteries (which are each named based on the region of the kidney they pass through) and ends with the exiting of the renal veins to join the inferior vena cava. The renal arteries split into several segmental arteries upon entering the kidneys. Each segmental artery splits further into several interlobar arteries and enters the renal columns, which supply the renal lobes. The interlobar arteries split at the junction of the renal cortex and medulla to form the arcuate arteries. The arcuate “bow shaped” arteries form arcs along the base of the medullary pyramids. Cortical radiate arteries, as the name suggests, radiate out from the arcuate arteries. The cortical radiate arteries branch into numerous afferent arterioles, and then enter the capillaries supplying the nephrons. Veins trace the path of the arteries and have similar names, except there are no segmental veins.
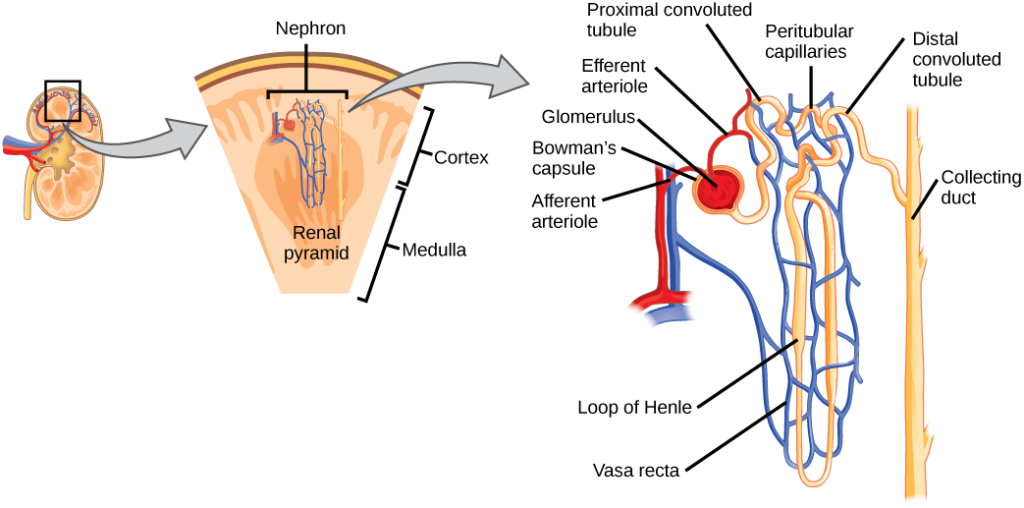
As mentioned previously, the functional unit of the kidney is the nephron, illustrated in Figure 22.6. Each kidney is made up of over one million nephrons that dot the renal cortex, giving it a granular appearance when sectioned sagittally. There are two types of nephrons— cortical nephrons (85 percent), which are deep in the renal cortex, and juxtamedullary nephrons (15 percent), which lie in the renal cortex close to the renal medulla. A nephron consists of three parts—a renal corpuscle, a renal tubule, and the associated capillary network, which originates from the cortical radiate arteries.
Which of the following statements about the nephron is false?
- The collecting duct empties into the distal convoluted tubule.
- The Bowman’s capsule surrounds the glomerulus.
- The loop of Henle is between the proximal and distal convoluted tubules.
- The loop of Henle empties into the distal convoluted tubule.
Renal Corpuscle
The renal corpuscle, located in the renal cortex, is made up of a network of capillaries known as the glomerulus and the capsule, a cup-shaped chamber that surrounds it, called the glomerular or Bowman’s capsule.
Renal Tubule
The renal tubule is a long and convoluted structure that emerges from the glomerulus and can be divided into three parts based on function. The first part is called the proximal convoluted tubule (PCT) due to its proximity to the glomerulus; it stays in the renal cortex. The second part is called the loop of Henle, or nephritic loop, because it forms a loop (with descending and ascending limbs) that goes through the renal medulla. The third part of the renal tubule is called the distal convoluted tubule (DCT) and this part is also restricted to the renal cortex. The DCT, which is the last part of the nephron, connects and empties its contents into collecting ducts that line the medullary pyramids. The collecting ducts amass contents from multiple nephrons and fuse together as they enter the papillae of the renal medulla.
Capillary Network within the Nephron
The capillary network that originates from the renal arteries supplies the nephron with blood that needs to be filtered. The branch that enters the glomerulus is called the afferent arteriole. The branch that exits the glomerulus is called the efferent arteriole. Within the glomerulus, the network of capillaries is called the glomerular capillary bed. Once the efferent arteriole exits the glomerulus, it forms the peritubular capillary network, which surrounds and interacts with parts of the renal tubule. In cortical nephrons, the peritubular capillary network surrounds the PCT and DCT. In juxtamedullary nephrons, the peritubular capillary network forms a network around the loop of Henle and is called the vasa recta.
Concept in Action

Go to
this website to see another coronal section of the kidney and to explore an animation of the workings of nephrons.
Kidney Function and Physiology
Kidneys filter blood in a three-step process. First, the nephrons filter blood that runs through the capillary network in the glomerulus. Almost all solutes, except for proteins, are filtered out into the glomerulus by a process called glomerular filtration. Second, the filtrate is collected in the renal tubules. Most of the solutes get reabsorbed in the PCT by a process called tubular reabsorption. In the loop of Henle, the filtrate continues to exchange solutes and water with the renal medulla and the peritubular capillary network. Water is also reabsorbed during this step. Then, additional solutes and wastes are secreted into the kidney tubules during tubular secretion, which is, in essence, the opposite process to tubular reabsorption. The collecting ducts collect filtrate coming from the nephrons and fuse in the medullary papillae. From here, the papillae deliver the filtrate, now called urine, into the minor calyces that eventually connect to the ureters through the renal pelvis. This entire process is illustrated in Figure 22.7.
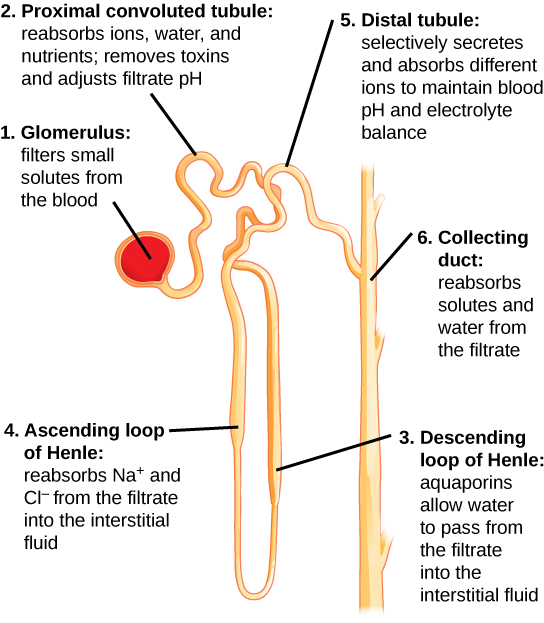
Glomerular Filtration
Glomerular filtration filters out most of the solutes due to high blood pressure and specialized membranes in the afferent arteriole. The blood pressure in the glomerulus is maintained independent of factors that affect systemic blood pressure. The “leaky” connections between the endothelial cells of the glomerular capillary network allow solutes to pass through easily. All solutes in the glomerular capillaries, except for macromolecules like proteins, pass through by passive diffusion. There is no energy requirement at this stage of the filtration process. Glomerular filtration rate (GFR) is the volume of glomerular filtrate formed per minute by the kidneys. GFR is regulated by multiple mechanisms and is an important indicator of kidney function.
Concept in Action

To learn more about the vascular system of kidneys, click through
this review and the steps of blood flow.
Tubular Reabsorption and Secretion
Tubular reabsorption occurs in the PCT part of the renal tubule. Almost all nutrients are reabsorbed, and this occurs either by passive or active transport. Reabsorption of water and some key electrolytes are regulated and can be influenced by hormones. Sodium (Na+) is the most abundant ion and most of it is reabsorbed by active transport and then transported to the peritubular capillaries. Because Na+ is actively transported out of the tubule, water follows it to even out the osmotic pressure. Water is also independently reabsorbed into the peritubular capillaries due to the presence of aquaporins, or water channels, in the PCT. This occurs due to the low blood pressure and high osmotic pressure in the peritubular capillaries. However, every solute has a transport maximum and the excess is not reabsorbed.
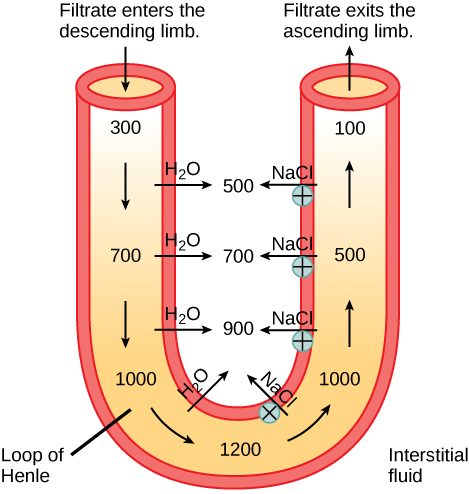
In the loop of Henle, the permeability of the membrane changes. The descending limb is permeable to water, not solutes; the opposite is true for the ascending limb. Additionally, the loop of Henle invades the renal medulla, which is naturally high in salt concentration and tends to absorb water from the renal tubule and concentrate the filtrate. The osmotic gradient increases as it moves deeper into the medulla. Because two sides of the loop of Henle perform opposing functions, as illustrated in Figure 22.8, it acts as a countercurrent multiplier. The vasa recta around it acts as the countercurrent exchanger.
Loop diuretics are drugs sometimes used to treat hypertension. These drugs inhibit the reabsorption of Na+ and Cl– ions by the ascending limb of the loop of Henle. A side effect is that they increase urination. Why do you think this is the case?
By the time the filtrate reaches the DCT, most of the urine and solutes have been reabsorbed. If the body requires additional water, all of it can be reabsorbed at this point. Further reabsorption is controlled by hormones, which will be discussed in a later section. Excretion of wastes occurs due to lack of reabsorption combined with tubular secretion. Undesirable products like metabolic wastes, urea, uric acid, and certain drugs, are excreted by tubular secretion. Most of the tubular secretion happens in the DCT, but some occurs in the early part of the collecting duct. Kidneys also maintain an acid-base balance by secreting excess H+ ions.
Although parts of the renal tubules are named proximal and distal, in a cross-section of the kidney, the tubules are placed close together and in contact with each other and the glomerulus. This allows for exchange of chemical messengers between the different cell types. For example, the DCT ascending limb of the loop of Henle has masses of cells called macula densa, which are in contact with cells of the afferent arterioles called juxtaglomerular cells. Together, the macula densa and juxtaglomerular cells form the juxtaglomerular complex (JGC). The JGC is an endocrine structure that secretes the enzyme renin and the hormone erythropoietin. When hormones trigger the macula densa cells in the DCT due to variations in blood volume, blood pressure, or electrolyte balance, these cells can immediately communicate the problem to the capillaries in the afferent and efferent arterioles, which can constrict or relax to change the glomerular filtration rate of the kidneys.
Nephrologist
A nephrologist studies and deals with diseases of the kidneys—both those that cause kidney failure (such as diabetes) and the conditions that are produced by kidney disease (such as hypertension). Blood pressure, blood volume, and changes in electrolyte balance come under the purview of a nephrologist.
Nephrologists usually work with other physicians who refer patients to them or consult with them about specific diagnoses and treatment plans. Patients are usually referred to a nephrologist for symptoms such as blood or protein in the urine, very high blood pressure, kidney stones, or renal failure.
Nephrology is a subspecialty of internal medicine. To become a nephrologist, medical school is followed by additional training to become certified in internal medicine. An additional two or more years is spent specifically studying kidney disorders and their accompanying effects on the body.
Summary
The kidneys are the main osmoregulatory organs in mammalian systems; they function to filter blood and maintain the osmolarity of body fluids at 300 mOsm. They are surrounded by three layers and are made up internally of three distinct regions—the cortex, medulla, and pelvis.
The blood vessels that transport blood into and out of the kidneys arise from and merge with the aorta and inferior vena cava, respectively. The renal arteries branch out from the aorta and enter the kidney where they further divide into segmental, interlobar, arcuate, and cortical radiate arteries.
The nephron is the functional unit of the kidney, which actively filters blood and generates urine. The nephron is made up of the renal corpuscle and renal tubule. Cortical nephrons are found in the renal cortex, while juxtamedullary nephrons are found in the renal cortex close to the renal medulla. The nephron filters and exchanges water and solutes with two sets of blood vessels and the tissue fluid in the kidneys.
There are three steps in the formation of urine: glomerular filtration, which occurs in the glomerulus; tubular reabsorption, which occurs in the renal tubules; and tubular secretion, which also occurs in the renal tubules.
Exercises
- Which of the following statements about the kidney is false?
- The renal pelvis drains into the ureter.
- The renal pyramids are in the medulla.
- The cortex covers the capsule.
- Nephrons are in the renal cortex.
- Which of the following statements about the nephron is false?
- The collecting duct empties into the distal convoluted tubule.
- The Bowman’s capsule surrounds the glomerulus.
- The loop of Henle is between the proximal and distal convoluted tubules.
- The loop of Henle empties into the distal convoluted tubule.
- The macula densa is/are:
- present in the renal medulla.
- dense tissue present in the outer layer of the kidney.
- cells present in the DCT and collecting tubules.
- present in blood capillaries.
- The osmolarity of body fluids is maintained at ________.
- 100 mOsm
- 300 mOsm
- 1000 mOsm
- it is not constantly maintained
- The gland located at the top of the kidney is the ________ gland.
- adrenal
- pituitary
- thyroid
- thymus
- Loop diuretics are drugs sometimes used to treat hypertension. These drugs inhibit the reabsorption of Na+ and Cl– ions by the ascending limb of the loop of Henle. A side effect is that they increase urination. Why do you think this is the case?
- Why are the loop of Henle and vasa recta important for the formation of concentrated urine?
- Describe the structure of the kidney.
Answers
- C
- A
- C
- B
- A
- Loop diuretics decrease the excretion of salt into the renal medulla, thereby reducing its osmolality. As a result, less water is excreted into the medulla by the descending limb, and more water is excreted as urine.
- The loop of Henle is part of the renal tubule that loops into the renal medulla. In the loop of Henle, the filtrate exchanges solutes and water with the renal medulla and the vasa recta (the peritubular capillary network). The vasa recta acts as the countercurrent exchanger. The kidneys maintain the osmolality of the rest of the body at a constant 300 mOsm by concentrating the filtrate as it passes through the loop of Henle.
- Externally, the kidneys are surrounded by three layers. The outermost layer is a tough connective tissue layer called the renal fascia. The second layer is called the perirenal fat capsule, which helps anchor the kidneys in place. The third and innermost layer is the renal capsule. Internally, the kidney has three regions—an outer cortex, a medulla in the middle, and the renal pelvis in the region called the hilum of the kidney, which is the concave part of the “bean” shape.
Glossary
- afferent arteriole
- arteriole that branches from the cortical radiate artery and enters the glomerulus
- arcuate artery
- artery that branches from the interlobar artery and arches over the base of the renal pyramids
- ascending limb
- part of the loop of Henle that ascends from the renal medulla to the renal cortex
- Bowman’s capsule
- structure that encloses the glomerulus
- calyx
- structure that connects the renal pelvis to the renal medulla
- cortex (animal)
- outer layer of an organ like the kidney or adrenal gland
- cortical radiate artery
- artery that radiates from the arcuate arteries into the renal cortex
- cortical nephron
- nephron that lies in the renal cortex
- countercurrent exchanger
- peritubular capillary network that allows exchange of solutes and water from the renal tubules
- countercurrent multiplier
- osmotic gradient in the renal medulla that is responsible for concentration of urine
- descending limb
- part of the loop of Henle that descends from the renal cortex into the renal medulla
- distal convoluted tubule (DCT)
- part of the renal tubule that is the most distant from the glomerulus
- efferent arteriole
- arteriole that exits from the glomerulus
- glomerular filtration
- filtration of blood in the glomerular capillary network into the glomerulus
- glomerular filtration rate (GFR)
- amount of filtrate formed by the glomerulus per minute
- glomerulus (renal)
- part of the renal corpuscle that contains the capillary network
- hilum
- region in the renal pelvis where blood vessels, nerves, and ureters bunch before entering or exiting the kidney
- inferior vena cava
- one of the main veins in the human body
- interlobar artery
- artery that branches from the segmental artery and travels in between the renal lobes
- juxtaglomerular cell
- cell in the afferent and efferent arterioles that responds to stimuli from the macula densa
- juxtamedullary nephron
- nephron that lies in the cortex but close to the renal medulla
- kidney
- organ that performs excretory and osmoregulatory functions
- lobes of the kidney
- renal pyramid along with the adjoining cortical region
- loop of Henle
- part of the renal tubule that loops into the renal medulla
- macula densa
- group of cells that senses changes in sodium ion concentration; present in parts of the renal tubule and collecting ducts
- medulla
- middle layer of an organ like the kidney or adrenal gland
- nephron
- functional unit of the kidney
- perirenal fat capsule
- fat layer that suspends the kidneys
- peritubular capillary network
- capillary network that surrounds the renal tubule after the efferent artery exits the glomerulus
- proximal convoluted tubule (PCT)
- part of the renal tubule that lies close to the glomerulus
- renal artery
- branch of the artery that enters the kidney
- renal capsule
- layer that encapsulates the kidneys
- renal column
- area of the kidney through which the interlobar arteries travel in the process of supplying blood to the renal lobes
- renal corpuscle
- glomerulus and the Bowman’s capsule together
- renal fascia
- connective tissue that supports the kidneys
- renal pelvis
- region in the kidney where the calyces join the ureters
- renal pyramid
- conical structure in the renal medulla
- renal tubule
- tubule of the nephron that arises from the glomerulus
- renal vein
- branch of a vein that exits the kidney and joins the inferior vena cava
- segmental artery
- artery that branches from the renal artery
- transport maximum
- maximum amount of solute that can be transported out of the renal tubules during reabsorption
- tubular reabsorption
- reclamation of water and solutes that got filtered out in the glomerulus
- tubular secretion
- process of secretion of wastes that do not get reabsorbed
- ureter
- urine-bearing tube coming out of the kidney; carries urine to the bladder
- urinary bladder
- structure that the ureters empty the urine into; stores urine
- urine
- filtrate produced by kidneys that gets excreted out of the body
- vasa recta
- peritubular network that surrounds the loop of Henle of the juxtamedullary nephrons