Mary’s Health Part A: Osteoarthritis (OA)
Mary spent her years tending to her garden and home. Over the last few years, Mary has been having difficulties with maintaining their home both inside and out. Mary has been slowing down with her indoor and outdoor activities due to joint pain and stiffness.
In 2012, Mary went to see her family physician because the over the counter medications she had been taking were no longer relieving her joint pain and stiffness.

Major Joints affected & Mary’s Symptoms
| Hand | Hip |
|
|
| Shoulder | Foot |
|
|
| Knee | Spine |
|
|
Mary being diagnosed with Stage 4 OA
In 2012 Mary was diagnosed with Stage 4 osteoarthritis (OA) and osteoporosis(OP)
Diagnosis
During the physical exam, the doctor checks affected joints for tenderness, swelling, redness, and flexibility
Imaging tests
X-rays: Cartilage doesn’t show up on X-ray images, but cartilage loss is revealed by a narrowing of the space between the bones in your joint. An X-ray can also show bone spurs around a joint.
Magnetic resonance imaging (MRI): An MRI uses radio waves and a strong magnetic field to produce detailed images of bone and soft tissues, including cartilage. An MRI isn’t commonly needed to diagnose osteoarthritis but can help provide more information in complex cases.
Bone densitometry. Uses a very small dose of ionizing radiation to produce pictures of the inside of the body (usually the lower (or lumbar) spine and hips) to measure bone loss.
Lab tests
Blood tests: Although there’s no blood test for osteoarthritis, certain tests can help rule out other causes of joint pain, such as rheumatoid arthritis.
Joint fluid analysis: Your doctor might use a needle to draw fluid from an affected joint. The fluid is then tested for inflammation and to determine whether your pain is caused by gout or an infection rather than osteoarthritis.
Osteoarthritis
Overview
- Called degenerative joint disease
- Most common form of arthritis
- Affecting millions of people worldwide

Characteristics
- Occurs when the protective cartilage that cushions the ends of the bones wears down overtime
- Can damage any joint
- Most commonly affects joints in hands, knees, hips and spine
- Can cause pain, stiffness and swelling
- Can cause reduced function & disability
Imaging test: X-rays

Osteoarthritic Hip and Spine

Osteoarthritis specific tests
Synovial Fluid Viscosity
- Indicates if joint fluid is normal or abnormal
- Very viscous
- Less viscous in infection or arthritis
- Hyaluronidase released by neutrophils destroys the hyaluronic acid that is required for joint lubrication
Bedside String Test
- Indicates presence of disease
- Failure to form a string is indicative of disease
- Normal synovial fluid forms a 3-6 cm string from the tip of a syringe

Testing Mary’s joints for crystals
Synovial Fluid Crystals
- Important in the identification of arthritis
Calcium Pyrophosphate (CPP)
- Seen in degenerative arthritis
- Must be performed soon after collection to avoid degradation of crystal formations
Stage 4 OA
Stage 4 – Severe
- Bone realignment surgery for knee & hip
- Pain medication or hyaluronic injections
- Cartilage is almost completely gone, bone spurs have multiplied, very painful
- Inflammatory response
Stepped-Care Approach for the Treatment of OA
OA cannot be reversed. However, treatments can reduce pain and improve movement.
NSAID (Nonsteroidal anti-inflammatory drugs)
This approach is recommended by the physician to manage Mary’s care
Mary is prescribed Celebrex & Acetaminophen
| Medication | Typical Dosage |
| Acetaminophen | 650 to 1000 mg QID |
| Celecoxib (Celebrix) | 50 to 400 mg OD |
| Diclofenac/misoprostol (Arthrotec) | 50 mg/200 mcg BID-TID |
| Ibuprofen (OTC) | 400 to 600 mg TID |
| Meloxicam (Mobic) | 7.5 to 15 mg OD |
| Nabumetone | 500 mg BID |
| Naproxen (OTC) (Aleve) | 220 to 440 mg BID |
| Oxaprozin (Daypro) | 1200 mg OD |
| Sulindac (Clinoril) | 150 to 200 mg BID |
These medications are Over the counter (OTC) medications commonly used to manage pain and inflammation related to Osteoarthritis.
Acetaminophen acts by reducing pain to facilitate mobility for a short duration, however, as Mary has advanced Stage 4 Osteoarthritis this medication was not helpful for her.
Celecoxib acts to relieve pain and inflammation. It is a Nonsteroidal anti-inflammatory drug similar to Aspirin and it targets pain receptors and blocks them temporarily and prevents immune inflammatory responses for a short period. This would relieve Mary of her OA symptoms of pain, stiffness, and swelling of her joints.
Over the counter (OTC) medications aren’t working for Mary….
Characteristics
- Opioids-low dosages and careful monitoring
- Intra-articular injections of corticosteroids or hyaluronic acid
OTC Risks
- May cause flare-up within the first 24 hours
- May cause chronic constipation
- Older patients at risk of falls
OTC
- Short-term relief lasting 4-8 weeks
- Improvement from baseline at 48 hours
Therapeutic Drug Monitoring (TDM)
TDM required if:
- Pharmacokinetics are variable
- Drug has a narrow therapeutic range
- Elimination of drug is highly affected by clinical state (i.e. kidney disease, liver disease)
- Patient requires chronic prescriptions
- Other factors
Routes of ingestion and digestion/metabolism of a drug:
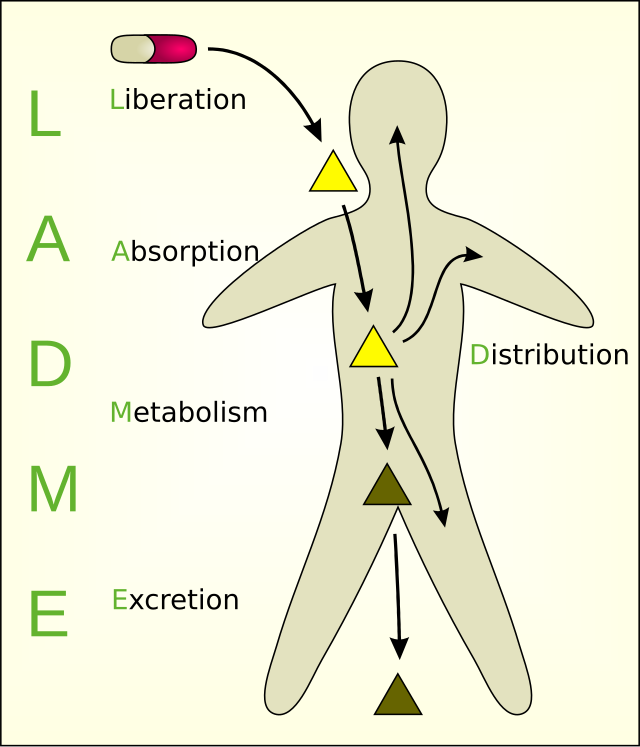
When drugs enter the body they go through 4 processes:
- Absorption– enters the bloodstream (i.e. orally, intravenously, etc.)
- Distribution– distributed through body (which receptor they bind to and how they interact with cell membranes)
- Metabolism– broken down/ chemically altered to aide in removal from body
- Elimination– excreted/ removed (generally via kidneys through urine)
Therapeutic Drug Monitoring (TDM)
- If drug is administered at time intervals equal to the drug’s half-life, the drug will reach a steady state after 5 doses
- Ideal time for blood collection to determine peak concentration
- Trough blood collection is the lowest concentration, taken just before next dose
Goal
To reach equilibrium where the rate of drug administration = rate of drug elimination to prevent toxicity. This is dependent on the half life of the medication

