Hugh’s Health Part A: Hypertension
Hugh and Gladys entertained often, socialized with the elite of Toronto. Rich foods and large amounts of alcohol were an everyday occurrence for this couple.
In 1990, Hugh was seen by his family physician for headaches, vision problems, fatigue, and occasional nose bleeds. Hugh had repeated blood pressure readings of 150/90 mm Hg and was given instructions to change his lifestyle.
Hugh was put on a diuretic and angiotensin converting enzyme (ACE) inhibitor. He was able to manage his hypertension with these medications. He did not change his lifestyle as recommended by his physician.

Components of Arterial Blood Pressure
The systolic pressure is the higher value and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole.
The diastolic pressure is the lower value and represents the arterial pressure of blood during ventricular relaxation, or diastole.

Managing Hypertension
| Blood Pressure Category | Systolic (mm Hg) | Diastolic (mm Hg) |
| Ideal | 115 | 75 |
| Normal | 120 | 80 |
| Pre-Hypertension | 120-139 | 80-89 |
| Hypertension | 140 (or higher) | 90 (or higher) |
How should he interpret his repeated blood pressure readings of 150/90 mm Hg?
Hugh has to make lifestyle changes
- Exercise
- Healthy diet
- Manage salt intake
- Healthy weight
- Stress management
- Limit alcohol
- No smoking
Hugh’s Hypertension Medications
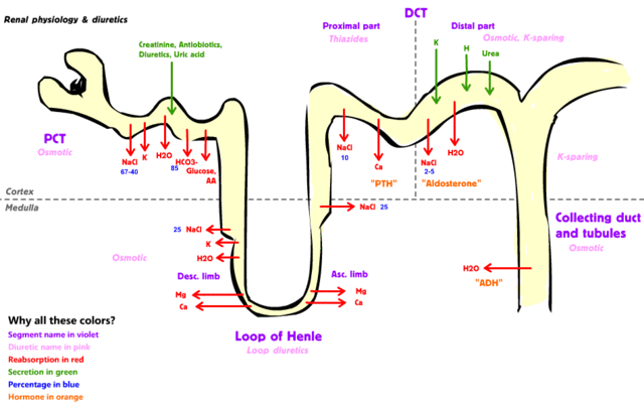
Diuretics
- Get rid of excess sodium and water, often used with additional prescription therapies
- Thiazide diuretics, potassium-sparing diuretics, combination diuretics
ACE inhibitors
Help to produce less angiotensin, blood vessels relax and open up
Hugh’s Blood Pressure Medications
Furosemide (Lasix)-loop diuretic
- Inhibits the NKCC2 cotransporter.
- Inhibits the reabsorption of sodium.
- The interstitium will lose its tonicity.
- Affecting how much water is reabsorbed by the Loop of Henle and collecting ducts.
- More water leaves via the filtrate rather than go back into the blood.
Ramipril (Altace)-ACE inhibitor
- Reduce the activity of angiotensin-converting enzyme.
- ACE is responsible for hormones that help control BP.
- Narrowing effect on blood vessels that ↑BP.
- ACE inhibitors limit this enzyme, making the blood vessels relax and widen.
- Lowering BP and improving blood flow to the heart muscle.
Understanding the Renin- Angiotensin Activation System
The RAAS system is controlled by the Sympathetic Nervous System and causes the body to increase Blood Pressure during periods of stress via RAAS
- This is activated to maintain adequate perfusion/ BP when the body identifies decreased blood volume is present
- This is a natural hormonal response that the body completes without medications
Example: Hypovolemic shock
Main Organs Involved in the RAAS System
| Brain | Posterior Pituitary gland secretes ADH hormone triggering the reabsorption of water to increase blood volume |
| Kidneys | Juxtaglomerular cells secrete renin that is released into the blood to metabolize Angiotensin and the Adrenal glands of the kidneys secrete aldosterone to reabsorb sodium and water |
| Lungs | The lungs produce the special enzyme ACE (Angiotensin Converting Enzyme) to turn Angiotensin 1 in to the active form of Angiotensin 2. |
| Liver | The liver produces the protein Angiotensinogen to facilitate the hormonal response and increases systemic BP |
| Heart and Vascular System | Angiotensin 2 binds to alpha-Adrenergic 2 receptor in the endothelium of blood vessels and stimulates vasoconstriction and increase BP |

Critical Thinking Questions
Select the client in which activation of the RAAS system would be contraindicated?
-
- A client experiencing an asthma attack
- A client with pneumonia
- A client with a closed head injury
- A client that is 3 days postoperative following a cardiac bypass surgery
Clients with traumatic brain injuries typically already have swelling of the brain components, if the BP increases then this may affect perfusion and result in hypoxia/ irreversible brain death therefore fluid should be removed from the body and BP controlled to prevent RAAS activation
What is the mechanism of action for a ACE inhibitor medication?
This medication would act on the ACE enzyme produced by the lungs and prevent the conversion of Angiotensin 1 to Angiotensin 2 preventing the systematic rise in BP.
What are some potential health complications for Hugh related to his substance abuse, HTN, and current prognosis?
-
- Heart Failure- increasing myocardial stretch may result in hypertrophy and reduced ejection fraction
- Kidney Failure- not excreting waste products
- Stroke-cerebral ischema
- Deep vein thrombosis
- Metabolic syndrome
- Anticholinergic effects- dry mouth/ constipation/ urinary retention/ photophobia/ blurred vision/ drowsiness

