Hugh’s Health Part B: Benign Prostatic Hyperplasia
Hugh was now experiencing urinary issues that he had attributed to the normal aging process. He frequently needed to urinate, especially at night, though he had difficulty starting to urinate, and once he did it was a weak stream. He was unable to completely empty his bladder.
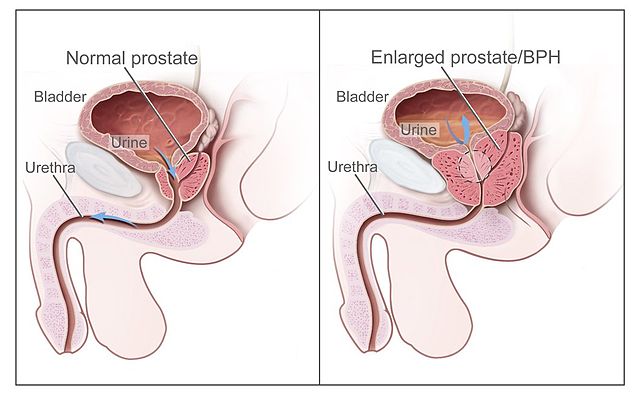
Once again, Hugh decided to see his family physician. Physical examination and mildly elevated serum prostate-specific antigen (PSA) confirmed that Hugh had benign prostatic hyperplasia (BPH), is a common condition as men age.
Risk Factors
- Aging
- Family history
- Diabetes or heart disease
- Lifestyle
Complications
- Sudden inability to urinate
- Urinary tract infection (UTI)
- Bladder calculi
- Bladder damage
- Kidney damage
Hugh’s Benign Prostatic Hyperplasia (BPH)

Diagnostics for BPH
- Digital rectal exam. The doctor inserts a finger into the rectum to check your prostate for enlargement.
- Urine test. Analyzing a sample of your urine can help rule out an infection or other conditions that can cause similar symptoms.
- Blood test. The results can indicate kidney problems.
- Prostate-specific antigen (PSA) blood test. PSA is a substance produced in your prostate. PSA levels increase when you have an enlarged prostate. However, elevated PSA levels can also be due to recent procedures, infection, surgery or prostate cancer.
- Urinary flow test. You urinate into a receptacle attached to a machine that measures the strength and amount of your urine flow. Test results help determine over time if your condition is getting better or worse.
- Post void residual volume test. This test measures whether you can empty your bladder completely. The test can be done using ultrasound or by inserting a catheter into your bladder after you urinate to measure how much urine is left in your bladder.
- 24-hour voiding diary. Recording the frequency and amount of urine might be especially helpful if more than one-third of your daily urinary output occurs at night.
Prostate Specific Antigen
3 forms found in blood:
- Complexed to α1-antichymotrypsin
- Free PSA (unbound, not complexed)
- Enveloped by α2-macroglobulin
Only the first two are immunologically detectable
Assays available for Free PSA and Total PSA
Total PSA used to monitor and detect prostate cancer
Elevated levels also seen in benign prostatic hypertrophy
Do not perform testing after:
- Procedures involving manipulation of prostate (i.e. DRE, cystoscopy, transrectal ultrasound)
- Resection of the prostate/prostate biopsy
- Ideally should wait 6 weeks following any of these procedures to avoid falsely elevated results
Note: Only serum samples may be used
Surgical Intervention for Hugh

Given Hugh’s symptoms, he was scheduled for a transurethral resection of the prostate (TURP)
Transurethral Resection of the Prostate is usually considered if:
- Your symptoms are moderate to severe
- Medication hasn’t relieved your symptoms
- You have a urinary tract obstruction, bladder stones, blood in your urine or kidney problems
- You prefer definitive treatment
- Transurethral Resection of the Prostate (TURP)

