Gladys’ Health Part B: Alzheimer’s
Gladys was becoming increasingly forgetful and would often behave in ways that were not normal for her.
She would forget that she had something on the stove or forget to turn her oxygen on. She was often unkempt and continually asking when Paul would be home from school.
Glady was found numerous times wondering the streets unaware of how to get home. She once thought Paul was Hugh and started kissing him. She would physically abuse Hugh when he was trying to help her.
Hugh took her to see her family physician who diagnosed Gladys with Alzheimer’s disease.
Alzheimer’s Disease
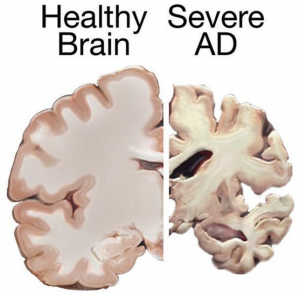
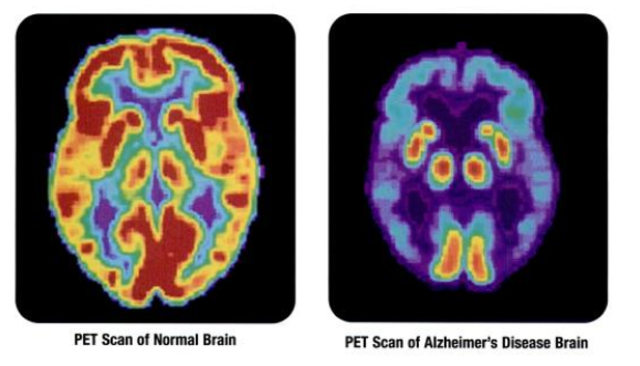
People with AD gradually suffer memory loss and a decline in thinking abilities, as well as major personality changes. These losses in cognitive function are accompanied by changes in the brain, including the build-up of amyloid plaques and tau-containing neurofibrillary tangles, which result in the death of brain cells and the breakdown of the connections between them.
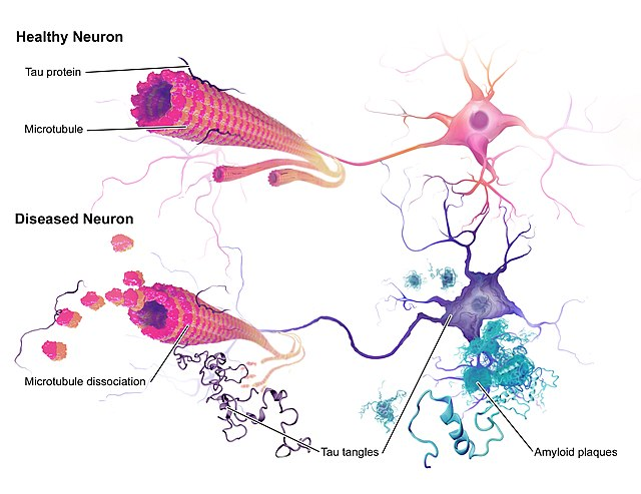
Amyloid plaques and neurofibrillary tangles are the primary hallmarks of Alzheimer’s disease. Plaques are dense deposits of protein and cellular material outside and around the brain’s nerve cells. Tangles are twisted fibers that build up inside the nerve cells. Scientists have known about plaques and tangles since 1906, when a German physician, Dr. Alois Alzheimer, first identified them in the brain of woman who had died after suffering paranoid delusions and psychosis.
Laboratory Tests
Doctors may order a panel of tests used to help rule out conditions that contribute to, or cause similar symptoms. Some of these tests might include:
Vitamin B12
- Important for brain & nerve function
- Red blood cell production
- Cell repair
CBC (Complete Blood Count)
Gives summary of blood components to help determine the cause of many symptoms
TSH (Thyroid Stimulating Hormone)
Rule out neurologic symptoms from possible thyroid disorders
Toxicology screen
Alcohol and drug tests to rule out symptoms of intoxication
Electrolytes
Balance is important for normal brain & nerve function
Medications
| Drug Name | Drug Type & Use | How It Works | Common Side Effects | Manufacturer’s Recommended Dosage |
| Aricept® (donepezil) |
|
Prevents acetyl choline breakdown | Nausea, vomiting, diarrhea, muscle cramps, fatigue, weight loss |
|
| Namenda® (memantine) | N-methyl D-aspartate (NMDA) antagonist
Treats moderate – severe symptoms |
Blocks the toxic effects of excess glutamate and regulates glutamate activation | Dizziness, headache, diarrhea, constipation, confusion |
|
Personality and Behaviour Changes in Alzheimer’s
- Getting upset, worried, and angry more easily
- Acting depressed or not interested in things
- Hiding things or believing other people are hiding things
- Imagining things that aren’t there
- Wandering away from home
- Pacing
- Unusual sexual behaviour
- Hitting others
- Misunderstanding what is seen or heard
- Stops caring about how they look
Which of these changes are present in Gladys?
Managing Personality & Behavioural Changes
- Keep things simple; Ask or say one thing at a time
- Have a daily routine
- Reassurance that they are safe and you are there to help
- Focus on their feelings rather than their words
- Don’t argue or try to reason with them
- Try not to show frustration or anger
- Use humor when appropriate
- Allow a safe environment for pacing
- Try using music, singing, or dancing for distraction
- Ask them to help (“let’s set the table” or “I need help folding the clothes”)
Changes in Gladys’ Communication Skills
Persons with Alzheimer’s may have problems with:
- Finding the right word or losing their train of thought when speaking
- Understanding what words mean
- Paying attention during long conversations
- Remembering the steps in common activities
- Blocking out background noises
- Frustration if communication is not working
- Being very sensitive to the tone and loudness of voices
Making Communication Easier
Understand that Alzheimer’s causes changes in communication skills.
Try some tips that may make communication easier:
- Make eye contact and use their name
- Beware of your tone, loudness of voice, and body language
- Encourage two-way conversation for as long as possible
- Use other methods besides speaking, such as gentle touch
- Try distraction if communication creates problems
- Be patient
- Offer simple step-by-step instructions
- Try not to interrupt
- Don’t talk to the person using “baby talk” or a “baby voice”
Preventing Alzheimer’s with Physical activity
- Regular physical exercise is a beneficial strategy to lower the risk of Alzheimer’s and vascular dementia
- Exercise may directly benefit brain cells by increasing blood and oxygen flow in the brain
- Because of its known cardiovascular benefits, a medically approved exercise program is valuable part of any overall wellness plan
What is good for the heart is good for the head
Heart-healthy eating includes limiting the intake of sugar and saturated fats and making sure to eat plenty of fruits, vegetables, and whole grains. Two diets have been studied and may be beneficial to lowering the risk of Alzheimer’s.
Dash Diet
- Emphasizes vegetables, fruits, fat-free or low-fat dairy products, whole grains, fish, poultry, beans, seeds, nuts and vegetable oils.
- Limits sodium, sweets, sugary beverages, red meats
Mediterranean Diet
- Little red meat
- Emphasizes whole grains, fruits and vegetables, fish & shellfish, healthy fats like nuts and olive oil
Smoking & Alzheimer’s
- Inhaling tobacco smoke has been linked to oxidative stress.
- Oxidative stress is an imbalance between toxic molecules inside our cells and the antioxidants we need to remove them. This imbalance causes damage to cells in our body
- Smoking also damages the structure of your blood vessels, making it harder for blood to flow freely around the body and into the brain.
- The brain uses around 20% of the body’s oxygen supply from blood, which means anything stopping the brain from getting an oxygen-rich blood supply is stopping brain cells from getting the nutrients they need to survive, thrive and resist damage.
Alcohol & Alzheimer’s
- Heavy alcohol consumption over a long period of time can lead to brain damage.
- People who drink heavily over a long period of time are more likely to have a reduced volume of the brain’s white matter, which helps to transmit signals between different brain regions. This can lead to issues with the way the brain functions.
- Long-term heavy alcohol consumption can also result in a lack of vitamin thiamine B1 and Korsakoff’s Syndrome, a memory disorder affecting short term memory.
Gladys continued to deteriorate
By 2018, Gladys could no longer communicate and was completely dependent on others for her care. A care conference was called with her primary care team, Hugh and Paul. It was decided that it was best for Gladys to be placed in a long-term care facility.
Approximately nine months after admission Gladys was diagnosed with aspiration pneumonia. The facility’s physician presented Hugh with the options of antibiotics to treat the pneumonia and a feeding tube to provide Gladys with nutritional input while lowering the risk of aspiration. Based on what Hugh knew of Gladys’s values, he decided to withdraw all treatment and signed a DNR.
DNR and DNH Orders
- Ontario nursing home DNR & DNH orders reduce inappropriate hospitalizations, but not entirely
- 3 in 5 nursing home residents had a DNR recorded on admission (Do Not Resuscitate)
- 1 in 7 had a DNH (Do Not Hospitalize)
- Residents with a DNR or DNH were less likely to experience hospitalization or in-hospital death
Hospitalization:
- DNR: 13% less likely
- DNH: 30% less likely
In-hospital death:
- DNR: 40% less likely
- DNH: 60% less likely

