Hugh’s Health Part C: Colon Cancer
Hugh no longer had urinary issues, was sleeping better, had more energy, and was relieved that it was “nothing much”. Two months after his TURP, Hugh went in for his routine colonoscopy.
Biopsies were taken during the colonoscopy for testing in the lab. The pathologist reported Stage I colon cancer.
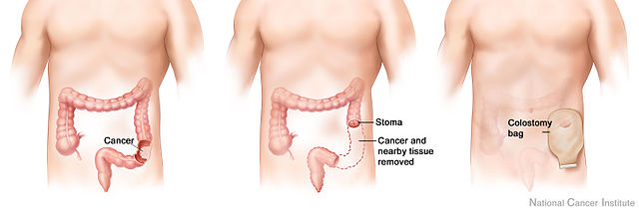
Hugh required a bowel resection which left him with a colostomy.

Histology of the Large Intestine

Stages of Colon Cancer
Stage 0 (Carcinoma in Situ)
- Abnormal cells found in the mucosa of the colon wall.
- These cells may become cancer and spread into nearby normal tissue.
Stage I Colon Cancer
- Cancer has formed in the mucosa of the colon wall.
- Has spread to the submucosa or to the muscle layer of the colon wall.
Stage II Colon Cancer
Is divided into stages IIA, IIB, and IIC:
Stage IIA
- Cancer has spread through the muscle layer of the colon to the serosa of the colon wall.
Stage IIB
- Cancer has spread through the serosa of the colon wall to the tissue that lines the organs in the abdomen.
Stage IIC
- Cancer has spread through the serosa of the colon wall to nearby organs
Stage III Colon Cancer
Is divided into stages IIIA, IIIB, and IIIC:
Stage IIIA
- Spread through the mucosa to the submucosa or the muscle layer and spread into 1 to 3 nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
- Or through the mucosa to the submucosa and spread to 4 to 6 nearby lymph nodes.
Stage IIIB
- Spread through the muscle layer to the serosa or has spread through the serosa to the tissue that lines the organs in the abdomen.
- Spread to 1 to 3 nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
- Spread to the muscle layer or to the serosa and to 4 to 6 nearby lymph nodes.
- Through the mucosa to the submucosa or to the muscle layer and spread to 7 or more nearby lymph nodes.
Stage IIIC
- Spread through the serosa to the tissue that lines the abdominal organs and spread to 4 to 6 nearby lymph nodes.
- Through the muscle layer to the serosa or spread through the serosa to the tissue that lines the abdominal organs and spread to 7 or more nearby lymph nodes.
- Spread through the serosa to nearby organs and spread to 1 or more nearby lymph nodes or cancer cells have formed in tissue near the lymph nodes.
Stage IV colon cancer
Is divided into stages IVA, IVB, and IVC:
Stage IVA
- Spread to one area or organ that is not near the colon or a distant lymph node.
Stage IVB
- Spread to more than one area or organ that is not near the colon or a distant lymph node.
Stage IVC
- Spread to the tissue that lines the wall of the abdomen and may have spread to other areas or organs.
Risk Factors for Colorectal Cancer
- Family history of colon or rectal cancer in a first-degree relative
- A personal history of cancer of the colon, rectum, or ovary
- Personal history of high-risk adenomas (colorectal polyps that are 1 cm or larger, or have abnormal cells)
- Inherited changes in certain genes that increase the risk (familial adenomatous polyposis or Lynch syndrome)
- Personal history of chronic ulcerative colitis or Crohn disease for 8 or more years
- 3 or more alcoholic drinks per day
- Smoking cigarettes
- Being black
- Being obese
- Older age
Which of these risk factors does Hugh possess?
Signs & Symptoms
- Change in bowel habits
- Blood (either bright red or very dark) in the stool
- Diarrhea, constipation, or feeling that the bowel does not empty
- Stools narrower than usual
- Frequent gas pains, bloating, fullness, or cramps
- Vomiting
- Unexplained weight loss
Diagnostic Tests for Hugh
- Physical exam and health history
- Sigmoidoscopy
- Digital rectal exam
- Guaiac FOBT
- Immunochemical FOBT
- Fecal occult blood test (FOBT)
- Barium enema
Hugh’s Colon Cancer Screening
Guaiac Fecal Occult Blood Test (FOBT): Development of blue colour indicates a POSITIVE result
Hemoglobin + Developer
Hb + 2H2O2 🡪 2H2O + O2
Oxidation of Guaiac
O2 + Guaiac (Colorless)🡪 Oxidized Guaiac (Blue)
QC test boxes need to show appropriate results
- Positive = BLUE
- Negative = COLOURLESS
FOBT
Juan is working in the lab and performs a FOBT. He performs the test appropriately according to the SOP and obtains the following results:
- Box A & B = colourless
- POS QC = colourless
- NEG QC = Colourless
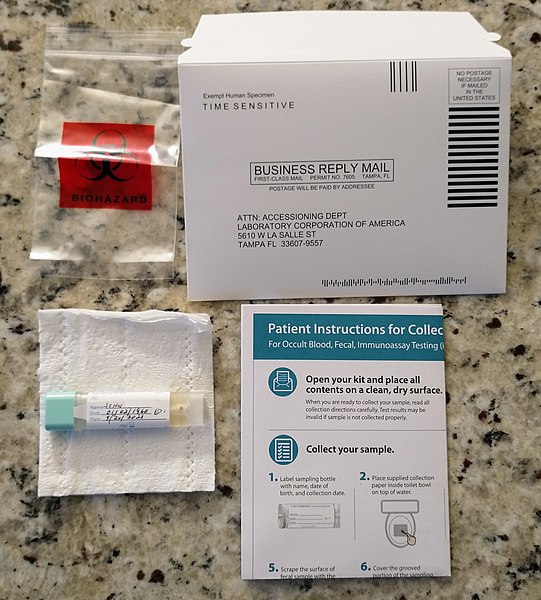
How should he interpret the results?
Ans: invalid, pos QC should be blue, rerun test
Troubleshooting:
Rerun test with a new ColoScreen card and ensure developer is not expired/contaminated. Use a new bottle of developer if necessary.
New results:
- Box A & B = blue,
- POS QC = blue,
- NEG QC = Colourless
How should he interpret the results?
Ans: positive
How does HTN increase the risk of developing Colon Cancer?
- Malabsorption and Chronic Malnutrition due to changes in the gut microbiome
- Resulting in conditions such as Peritonitis, GERD, GI Bleeds, GI Ulcers, GI Polyps, and recurrent inflammation of the bowel increasing risk of tumors present in Colorectal Cancer.
Hugh’s Surgical Treatment
- Resection of the colon with colostomy
- Unable to sew the 2 ends of the colon together
- A stoma (an opening) is made outside the body
- Waste passes through this opening a bag is placed around the stoma to collect the waste
- It can be reversed
How Will a Colostomy Change Hugh’s Life?
- Monitor your medications. Some meds can cause constipation or diarrhea.
- Eat a well-balanced diet. Avoid foods that cause a lot of gas.
- Live your life.
Concerns:
- Body image/self-esteem
- Relationships
- Self-care
After Hugh’s Surgical Treatment
With Gladys in long-term care, Hugh was living alone. Home care was ordered to teach him proper ostomy care.
Hugh’s self-image was suffering. He did not go out, was not eating properly due to fear of leakage at the ostomy site. He led a very sedentary life. He had concerns about Brian’s welfare, who would look after him once Hugh was gone? Brian had Down’s syndrome and lived at home where he was schooled and cared for. He was unable to reach out to his son Paul, to discuss helping out with himself and Brian.
Phases of Psychological Adaptation
Almost every patient goes through 4 phases of recovery following an accident or illness that results in loss of function of an important part of the body.
The patient and family go through these phases, varying only in the time required for each phase.
Some people may skip certain phases entirely and some may move up and down at different times.
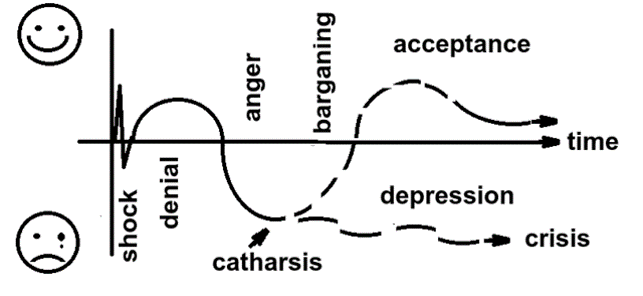
- Shock or panic-tearful, anxious and forgetful.
- Defense/retreat/denial-denies or minimizes the significance of the event, defends themselves against the implications of the event.
- Acknowledgement-begins to face the reality of the situation. Gives up the old life, and may enter a period of depression, of apathy, of agitation, of bitterness, and of high anxiety.
- Adaptation/resolution-acute grief begins to subside. Coping in a constructive manner and begins to establish new structures. Develops a new sense of worth.
Changing Hugh’s Lifestyle
- Diet change is hard. What works to motivate one person may not work for the next person
- Healthcare provider must educate on the benefits of a healthy lifestyle
- Referral to Dietitian
- Suggest small changes first – Provide evidence based health websites if they are interested in information or healthy recipes, but not yet ready to meet with a dietitian
Mediterranean Diet
Emphasis placed on:
- Plants, Fruits & vegetables
- Whole grains
- Legumes, Nuts, Seeds
- Fish & Poultry
- Low in saturated & trans fat
- Rich in unsaturated fat
- Rich in starch, fiber, whole grains
- Rich in nutrients and phytochemicals that support good health
Mediterranean diet may decrease an individual’s risk of complications from cardiac issues by 50-70%
Lifestyle modifications are the first line of therapy for hypertension management
- Reduced sodium uptake = 2000 mg/day
- Reduced alcohol intake = < 2 drinks/day
- Dietary Patterns (i.e. DASH) = DASH dietary pattern adherence
The Dash Diet Pattern
DASH = Dietary Approaches to Stop Hypertension
Significantly lowers blood pressure, especially when combined with a low sodium diet
| Food Group | Daily Serving | Examples |
| Whole grains | 6-8 | Whole wheat or mulitgrain breads, cereal, oatmeal, rice, pasta, quinoa, barley, etc. |
| Vegetables | 4-5 | Dark green and orange (fresh or frozen) |
| Fruit | 4-5 | Apricots, bananas, grapes, oranges, grapefruit, melons, peaches, berries, mango |
| Low fat/Fat free Milk & Alt | 2-3 | Skim, 1% milk, fortified soy beverage, yogurt, low fat cheese (6-18% MF) |
| Meat, Poultry, Fish | < 6 oz. | Select fresh lean meats. Choose fish like char, herring, mackerel, salmon, sardines and trout. Choose fresh unseasoned poultry and remove skin. For deli meat, choose lower sodium options. |
| Nuts, Seeds, Legumes | 4-5/wk | Almonds, peanuts, walnuts, sunflower seeds, lentils, chickpeas, dried peas/beans, tofu |
| Fats and Oils | 2-3 tsp | Soft margarines, mayonnaise, vegetable oils (i.e., olive, canola), salad dressing |
| Sweets | < 5 Tbsp/wk | Added sugar, honey, jelly, jam, hard candy, ice cream, syrups, sorbet, chocolate |

