Learning Objectives: Birth
|
Preparation for Childbirth
Prepared childbirth refers to being not only in good physical condition to help provide a healthy environment for the baby to develop, but also helping individuals to prepare to accept their new roles as parents. Additionally, parents can receive information and training that will assist them for delivery and life with the baby. The more future parents can learn about childbirth and the newborn, the better prepared they will be for the adjustment they must make to a new life.
One of the most common methods for preparing for childbirth is The Lamaze Method. This method originated in Russia and was brought to the United States in the 1950s by Fernand Lamaze. The emphasis of this method is on teaching the woman to be in control in the process of delivery. It includes learning muscle relaxation, breathing though contractions, having a focal point (usually a picture to look at) during contractions and having a support person who goes through the training process with the mother and serves as a coach during delivery (Eisenberg, Murkoff, & Hathaway, 1996).
Choosing Where to Have the Baby and Who Will Deliver: The vast majority of births occur in a hospital setting. However, one percent of women choose to deliver at home (Martin, Hamilton, Osterman, Curtin, & Mathews, 2015). Women who are at low risk for birth complications can successfully deliver at home. More than half (67%) of home deliveries are by certified nurse midwifes. Midwives are trained and licensed to assist in delivery and are far less expensive than the cost of a hospital delivery. However, because of the potential for a complication during the birth process, most medical professionals recommend that delivery take place in a hospital. Despite the concerns, in the United States women who have had previous children, who are over 25, and who are white are more likely to have out-of-hospital births (MacDorman, Menacker, & Declercq, 2010). In addition to home births, one-third of out-of- hospital births occur in freestanding clinics, birthing centers, in physician’s offices, or other locations.
Real Life: Planning a Birth in the GTA
Expecting families have a number of options to pick from when planning the birth experience in the Greater Toronto Area. From pain management practices, to location and service provider, to labour and delivery options, to post-birth procedures, there are a number of choices to make. If you were expecting a baby, what sorts of choices would you make? Work through the following three guiding questions now.
Would you prefer to be attended by your current family doctor, a specialist in obstetrics and gynecology, or a midwife? Use the following links to learn from real expectant mothers’ experiences, as you try to formulate your answer.
Would you hire a doula?
The following article includes a description of doulas in comparison to midwives. Read before you decide.
What would your birth plan look like?
Expectant mothers and their partners have the right to make informed decisions about their own labour and delivery experience, including pain management preferences, labouring options, and post-delivery care. Just some of the many post-delivery care options to choose from are:
-
-
- immediate skin-to-skin contact between one or more parents and the newborn.
- delayed cord clamping to ensure that the most possible cord blood is absorbed in the body before the umbilical cord is clamped and cut.
- stem cell collection.
- placement of infant in nursery.
-
Stages of Birth for Vaginal Delivery
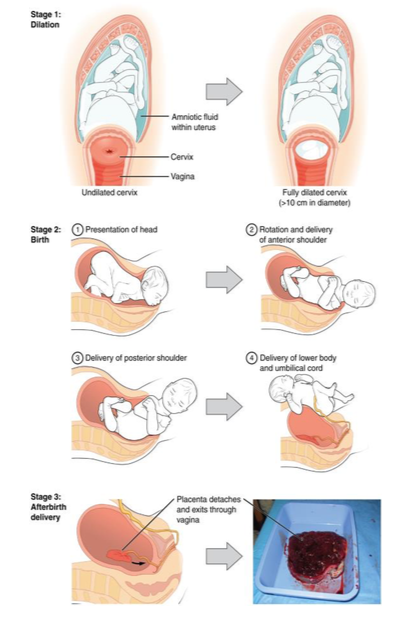
The First Stage of labor begins with uterine contractions that may initially last about 30 seconds and be spaced 15 to 20 minutes apart. These increase in duration and frequency to more than a minute in length and about 3 to 4 minutes apart. Typically, doctors advise that they be called when contractions are coming about every 5 minutes. Some women experience false labor or Braxton-Hicks Contractions, especially with the first child. These may come and go. They tend to diminish when the mother begins walking around. Real labor pains tend to increase with walking. Labor may also be signaled by a bloody discharge being expelled from the cervix. In one out of 8 pregnancies, the amniotic sac or water in which the fetus is suspended may break before labor begins. In such cases, the physician may induce labor with the use of medication if it does not begin on its own in order to reduce the risk of infection. Normally this sac does not rupture until the later stages of labor.
The first stage of labor is typically the longest. During this stage the cervix or opening to the uterus dilates to 10 centimeters or just under 4 inches (See Figure 2.16). This may take around 12-16 hours for first children or about 6-9 hours for women who have previously given birth. Labor may also begin with a discharge of blood or amniotic fluid.
The Second Stage involves the passage of the baby through the birth canal. This stage takes about 10-40 minutes. Contractions usually come about every 2-3 minutes. The mother pushes and relaxes as directed by the medical staff. Normally the head is delivered first. The baby is then rotated so that one shoulder can come through and then the other shoulder. The rest of the baby quickly passes through. At this stage, an episiotomy or incision made in the tissue between the vaginal opening and anus, may be performed to avoid tearing the tissue of the back of the vaginal opening (Mayo Clinic, 2016). The baby’s mouth and nose are suctioned out. The umbilical cord is clamped and cut.
The Third Stage is relatively painless. During this stage, the placenta or afterbirth is delivered. This is typically within 20 minutes after delivery. If an episiotomy was performed it is stitched up during this stage.
More than 50% of women giving birth at hospitals use an epidural anesthesia during delivery (American Pregnancy Association, 2015). An epidural block is a regional analgesic that can be used during labor and alleviates most pain in the lower body without slowing labor. The epidural block can be used throughout labor and has little to no effect on the baby. Medication is injected into a small space outside the spinal cord in the lower back. It takes 10 to 20 minutes for the medication to take effect. An epidural block with stronger medications, such as anesthetics, can be used shortly before a C-section or if a vaginal birth requires the use of forceps or vacuum extraction. A Cesarean Section (C-section) is surgery to deliver the baby by being removed through the mother’s abdomen. In the United States, about one in three women have their babies delivered this way (Martin et al., 2015). Most C-sections are done when problems occur during delivery unexpectedly. These can include:
-
-
- Health problems in the mother.
- Signs of distress in the baby.
- Not enough room for the baby to go through the vagina.
- The position of the baby, such as a breech presentation where the head is not in the downward position.
-
C-sections are also more common among women carrying more than one baby. Although the surgery is relatively safe for mother and baby, it is considered major surgery and carries health risks. Additionally, it also takes longer to recover from a C-section than from vaginal birth. After healing, the incision may leave a weak spot in the wall of the uterus. This could cause problems with an attempted vaginal birth later. However, more than half of women who have a C-section can give vaginal birth later.
An Induced Birth: Sometimes a baby’s arrival may need to be Induced or delivered before labor begins. Inducing labor may be recommended for a variety of reasons when there is concern for the health of the mother or baby. For example:
-
-
- The mother is approaching two weeks beyond her due date and labor has not started naturally.
- The mother’s water has broken, but contractions have not begun.
- There is an infection in the mother’s uterus.
- The baby has stopped growing at the expected pace.
- There is not enough amniotic fluid surrounding the baby.
- The placenta peels away, either partially or completely, from the inner wall of the uterus before delivery.
- The mother has a medical condition that might put her or her baby at risk, such as high blood pressure or diabetes (Mayo Clinic, 2014).
-

