12.5 Psychedelics, Medicine & Research
From Cannabis to Psychedelics
The term psychedelic was coined in 1957 by Dr. Humphrey Osmond, a psychiatrist, to mean “mind manifesting”, due to the ability of this class of substances to stimulate “changes in thought, perception, mood” (Osmond, 1957, p. 418).
The introduction of legal cannabis policies, combined with other experiments in drug policy (e.g., Portugal’s full decriminalization of drugs in 2001), the implementation of harm reduction measures (e.g., safe consumption sites, drug testing facilities, safe supply, etc.), and an increase in scientific research about psychoactive substances and their effects, have helped open the discussion about other progressive policy changes. One class of drugs receiving much attention are psychedelics (e.g., Psilocybin, Ketamine, MDMA, LSD, Ayahuasca) for medical purposes. Recent reviews of research on medical use of psychedelics from the middle of the 20th century, combined with a rapid growth in research on psychedelics, has fueled the latest push for policy reform and the legalization of certain psychedelic drugs for a variety of mental health conditions. Along side efforts to medicalize psychedelics, a legal psychedelic industry has begun to take shape.
VIDEO: How psychedelics work, explained in under 6 minutes – Matthew Johnson.
In the following video Johns Hopkins professor, Dr. Matthew Johnson, provides a quick explanation of the science of psychedelics substances.
Psychedelics as Medicine
First Wave: Traditional Medicines

The use of psychedelics for spiritual, mystic, health and healing purposes (e.g., mescaline, psilocybin, peyote, ayahuasca) by Indigenous communities long predates western-centric medicine and medical practices, and written historical accounts (Samorini, 2001; Strauss et al., 2022). This first wave of psychedelics as medicine is evidenced in fossils and rock art discovered by anthropologists around the world (Samorini, 1992, 2001), including the use of psilocybin mushrooms as far back as 9000 BCE in North Africa (Beck, 2021; Longrich, July 16, 2021; POPLAR, December 12, 2021) (see image above). Although there is much diversity in the specific rituals, practices, and beliefs across Indigenous groups, some similarities include psychedelics being viewed as sacred, “often administered through the guidance of a knowledgeable spiritual leader;… and carefully passed down across generations” (George et al., 2020, p. 5). Despite being one among an abundance of plant-based medicines integrated into modern Indigenous cultural and spiritual practices, such traditional knowledge and expertise, and the first wave more generally, is often overlooked in discussions of psychedelic medicine today (George et al., 2020; Sessa, 2006).
Second Wave: Western-Centric Medicine, 1940-60s
The event that precipitated the western-centric medical exploration of psychedelic substances, and the second wave of psychedelic medicine, occurred in the 1940s, when Dr. Albert Hoffman accidentally discovered the hallucinogenic properties of LSD (Lysergic Diethylamide). This discovery heralded the start of research into LSD-assisted psychotherapy. By the 1950s, Britain had a rich history in the area of psychedelic assisted mental health research and treatment (Sessa, 2006, p. 6) and studies in the area were taking place in other parts of the world (Costandi, September 2, 2014). From the 1950s-1965 the body of western-centric research grew, with studies finding that psychedelics could be used to treat a number of mental health and substance use issues. During this period of time, over 40,000 patients received LSD as part of their psychotherapeutic treatment. The studies of those treatments formed the basis for several dozen books and more than 1,000 published research reports (Costandi, September 2, 2014), some of which appeared in the newly founded Journal of Psychedelic Drugs (now known as the Journal of Psychoactive Drugs) (Smith, 2019).
Among the sources of promising research findings of the times, were Canadian studies at the University Hospital of Saskatchewan in early 1950s. These studies found LSD therapy to be an effective treatment for people experiencing alcohol use disorder (AUD), with some participants significantly reducing their consumption of alcohol, finding stable employment, and increasing their engagement with family and peers (MacDonald, June 12, 2007). Unfortunately, two issues emerged in the mid-1960s impacting psychedelic research: (1) a number of the studies of this time were critiqued for their lack of control groups and potential research bias (Costandi, September 2, 2014); and (2) in the 1960s LSD became embroiled in the politics of the counter-cultural movement, with its use demonized and blamed as the cause of social change occurring around the globe. By the end of the 1960s, LSD was criminalized in most countries and medical research in the area became extremely unpopular and difficult to conduct (Doblin et al., 2019; Sessa, 2006).
Click the link below to learn more about early Canadian research on psychiatric use of psychedelics:
Peaking on the prairies![]() (Warning: some stigmatizing terms are used, including the term “alcoholic”, “mental hospital”, “mental disorder”, etc.)
(Warning: some stigmatizing terms are used, including the term “alcoholic”, “mental hospital”, “mental disorder”, etc.)
Third Wave: Western-Centric Medicine, Late 1990s+
Following a similar western-centre approach to medicine as the second wave, the third wave of psychedelic medicine (also referred to as the “psychedelic renaissance”) began in the 1990s, with a rapid growth in research studies and publications (Dobin et al., 2019) applying contemporary research methods to the study of psychedelics. The research “came from two parallel directions. One was the development of neuroimaging and psychopharmacological studies… and the… [other] from some small exploratory clinical studies” (Nutt, 2019, p. 141.). In the second decade of the 21st century, psychedelic medicine is showing much promise for treating a variety of mental health conditions, becoming a separate field in the literature (Hadar et al., 2023).
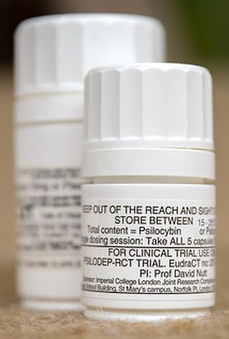
Clinical trials have been exploring the efficacy of various psychedelic substances (e.g., psilocybin, MDMA, ketamine) to treat conditions such as: PTSD; SUD, including OUD and AUD; depression; social anxiety; eating disorders and body dysmorphic disorders; grief; death distress and anxiety, etc., with promising results (Rush et al., 2022a). For example, in a 2022 publication in the Journal of Psychopharmacology, the researchers report evidence that suggests “that psilocybin-assisted treatment for MDD produces large and stable antidepressant effects throughout at least 12 months after treatment” (Gukasyan et al., 2022, p. 157). A 2016 study of psilocybin treatment among patients with a life threatening cancer diagnosis found that “under psychological supportive conditions…, a single dose of psilocybin produced substantial and enduring decreases in depressed mood and anxiety, along with increases in quality of life and decreases in death anxiety in patients” (Griffiths et al, 2016, p. 1195).
Click the link below to learn more about the state of knowledge based on medical psychedelic research from Homewood Research Institute & Queen’s University:
BCE stands for ‘Before Common Era’. As with its precursor, ‘BC’, these ways of measuring time reflect a Eurocentric ‘Christian’ perspective that does not appropriately consider the multitude of different ways that the notion of time has been understood by cultures globally.
Post Traumatic Stress Disorder
Opiate Use Disorder
Alcohol Use Disorder
Major depressive disorder (Gukasyan et al., 2022).

