Appendix F: Thinking Like a Nurse
ASSIGNMENT OUTCOME
Using the Gordon’s Functional Health Patterns and Thinking Like a Nurse Model, students will prepare for client based care and informed clinical decision making by collecting, organizing and beginning to interpret data.
INSTRUCTIONS
There are three parts to this assignment. Follow the instructions for each, as indicated below. In order to achieve ‘Requirements Met’, students must achieve satisfactory in all criteria.
Part A: Gordon’s Functional Health Patterns
Part B: “Thinking like a Nurse”
Part C: The Reflection Process
Part A: Gordon’s Functional Health Pattern Assessment
Patient’s Initials: Age: Date:
Diagnosis: History:
| Assessment Criteria | Patient Data | Influencing Factors |
| COGNITIVE- PERCEPTUAL PATTERN
(Neurological) |
||
| PAIN | ||
| SLEEP-REST PATTERN | ||
| ACTIVITY-EXERCISE PATTER | ||
| NUTRITIONAL- METABOLIC PATTERN | ||
| ELIMINATION PATTERN | ||
| SKIN INTEGRITY | ||
| HEALTH PERCEPTIONMANAGEMENT PATTERN | ||
| SELF CONCEPT PATTERN | ||
| ROLES-RELATIONSHIPS PATTERN | ||
| REPRODUCTIVE- SEXUALITY PATTERN | ||
| COPING-STRESS TOLERANCE PATTERN | ||
| VALUE-BELIEF PATTERN |
Gordon, M. (2008). Assess Notes. Davis: Philadelphia, Pa.
Assignment Rubric – Part A: Gordon’s Functional Health Patterns
| Criteria | Unsatisfactory | Satisfactory | Good | Comments |
| Organization | Patient data inaccurately organized within Gordon’s Functional Health Patterns | Patient data contains minor inaccuracies within Gordon’s Functional Health Patterns | Patient data accurately organized within Gordon’s Functional Health
Patterns |
|
| Accuracy of information | Information collected is inaccurate based on
Clinical Connect data and SP interview. |
Information collected contains significant inaccuracies based on Clinical Connect data and SP interview.
Significant gaps in |
Information collected is accurate based on Clinical Connect data and SP interview. | |
| comprehensiveness | ||||
| and completion | Information is | |||
| Information is not comprehensive and is incomplete | comprehensive and complete |
Part B: THINKING LIKE A NURSE
Part 1: Preparing for Client Care |
| Knowing the Client’s Medical Conditions: What is the underlying pathophysiology of my client’s medical diagnoses? What is the typical / usual clinical course? What types of treatments (including medications) are used and why? What is the nursing role in caring for a client with this diagnosis? What types of communication skills will I likely need to provide safe and effective care for my client. |
|
Knowing the Individual . . . |
| Client as a Person What is my client’s story (narrative)? How do (or might) my client’s past experiences with health & illness influence his/her responses to the pathophysiology, treatment, and care? Are there other factors affecting my client’s health or response to care (e.g., age, social context, spirituality, personal preferences, family, etc.)? |
|
Noticing – Gathering Cues & Information You need to gather data/ cues/ information from a wide variety of areas in order to thoroughly determine the main issues that are affecting your client. Look for the following information: |
| Chart Data Interprofessional health team notes. | Plan of Care Why is your client receiving care? Which members of the interprofessional team would be involved? |
| Cues from my Client & his/her Family Client’s perception of the situation; my own observations about the client’s needs? Does she have family? | Lab & Diagnostic Reports |
| Part 2: Interpreting Data and Implementing of Care | |
| Assessments Identify the priority assessments for this client. | |
| Interpreting – Recognizing Patterns and Interpreting Data | |
| Clinical Reasoning & Decision Making What are the most important nursing issues for my client & family today? What are the major nursing assessments you will use to collect data? What are the priorities of care? What is the client at risk for? What complications may arise? | Planning Outcomes What expected outcomes have been identified in collaboration with the client and the Interprofessional Health Care Team?
What short and long term goals should the plan of care address to achieve expected outcomes? |
| Responding – Determining a Course of Action | |
| Actions What interventions selected in collaboration with the client and the interprofessional team would best address my client’s identified needs and goals? | Rationale Why are these interventions appropriate? Support with evidence informed practice. |
| After the Professional Practice Experience | |
| Reflection – On Action and Clinical Learning |
Assignment Rubric – Part B: Thinking Like a Nurse
| Criteria | Unsatisfactory | Satisfactory | Good |
| Completeness | Significant gaps in competing section(s) of the Thinking Like
a Nurse Tool |
Most sections of the TLN tool are completed according to instructions. | All sections of the Thinking Like a Nurse (TLN) tool completed according to instructions. |
| Accuracy of information | Significant errors in identifying client data from the interview and/or clinical connect chart data.
Significant flaws in understanding medical diagnosis, treatment, nursing role and communication skills. |
Most information gathered from Clinical Connect and Client interview are correct.
Minor gaps evident in understanding medical diagnosis, medications, nursing role, or communication strategies |
All information presented demonstrated accurate understanding of: Patient interview, chart data (from clinical connect), accurate novice understanding of diagnosis, medications, nursing role and communication strategies. |
| Interpretation | Recognizes few client issues.
Does not set priorities.
Relevant short and long term goals for the client not identified.
No interventions identified or no rationale provided. |
Recognizes some important client issues.
Sets priorities.
Identifies relevant short and long term goals for the client based on priority issues.
Identifies a few interventions supported with rationale. |
Recognizes the most important client issues.
Sets priorities using guidelines.
Identifies relevant SMART short and long term goals for the client based on priority issues.
Identifies relevant interventions supported with rationale. |
| Evidence | Resources are poor and/or incomplete
Several APA errors. |
Resources are lacking in number and quality
Minor APA errors. |
Effective use of resources in number and quality.
APA style adhered to. |
Assignment Rubric- Part C: The Reflection Process
The Reflection Process
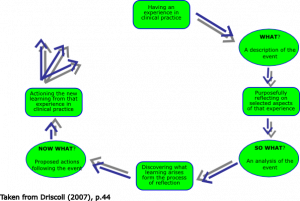
The What? Model of Structured Reflection (Driscoll, 2007)
This model offers a practical approach to reflection in the clinical setting. The model leads the student nurse through the reflection with the questions what?, so what?, and now what? (Bulman & Schutz, 2008).
In paragraph format, answer the following prompter questions that relate to your formative or summative reflection topic(s). Once completed, submit as a word document into the appropriate dropbox within MyCanvas.
What?
1. This is a description of the event Trigger questions:
- What is the purpose of returning to this situation?
- What happened?
- What did I see/do?
- What was my reaction to it?
- What did other people do who were involved in this?
So what?
2. This is an analysis of the event Trigger questions:
- How did I feel at the time of the event?
- Were those feelings I had different from other people who were also involved at the time?
- So what are my feelings now, after the event, different from what I experienced at the time?
- Do I feel troubled? If so, in what way?
- What were the effects of what I did (or did not do)?
- What positive effects now emerge for me from the event that happened in practice?
- What have I noticed in my behaviour in practice (knowledge, skills, and judgement) by taking a more measured look at it?
- How do the observations made by others impact my perceptions of the event?
Now what?
These are your proposed actions following the event Trigger questions:
- What are the implications for me and others in clinical practice based on what I have described and analyzed?
- What difference does it make if I choose to do nothing?
- Where can I get more information to face a similar situation again? Use a specific resource/research and use APA format to cite correctly?
- How could I modify my practice if a similar situation was to happen again?
- What help do I need to help me ‘action’ the results of my reflections?
- Which aspect should be tackled first?
- How will I notice that I am any different in my clinical practice?
- What is the main learning I take from reflecting on my practice this way?
http://www.nottingham.ac.uk/nmp/sonet/rlos/placs/critical_reflection/models/driscoll.html

