6 Respiratory Diseases of Cats
| Course priority #1 | Course priority #2 | Course priority #3 | |
| Cats |
|
|
|
viral respiratory diseases
- Feline herpesvirus (feline rhinotracheitis virus). Herpesvirus infections often are latent after the initial infection is cleared by the immune response, but recrudescence may occur during stressful periods, causing disease and/or infecting other cats. Intranuclear inclusion bodies are often present in diseased tissues.
- Feline calicivirus. Calicivirus infections may be chronic, and infected cats shed the virus almost continuously. Other rare but highly virulent strains of feline calicivirus cause severe systemic and fatal disease.
These viruses mainly infect the upper respiratory tract and conjunctival epithelium, causing necrosis of epithelial cells. In some cases, particularly in kittens, either of these viruses can infect the lung to cause primary viral pneumonia.
Upper respiratory viral infections are very common in young cats, and in older cats with impaired defences. The clinical signs are mucopurulent nasal and ocular discharge and sneezing, with or without fever. There may be secondary bacterial bronchopneumonia, or chronic rhinitis and sinusitis.
Why can upper respiratory infections become chronic?
- Persistent infections. Latent herpesvirus infection may be reactivated in times of stress. Calicivirus and Bordetella infections are often persistent.
- Respiratory defences are impaired. FeLV or FIV infections impair nasal defences. Chronic rhinitis destroys ciliated epithelium and excavates turbinate bone, impairing clearance of mucus from the nasal cavity.
- Infections of sinuses (sinusitis) and of bony tissue (osteomyelitis) may be difficult to eliminate.
Diagnosis: the specific cause is often not investigated, but may be useful in group situations to implement control procedures. Oral ulcers suggest calicivirus infection. Marked conjunctivitis is said to suggest chlamydiosis. Histologic observation of intranuclear inclusion bodies indicates herpesvirus. PCR testing of conjunctival or oropharyngeal swabs is useful to detect herpes- and calici-viruses. Bacterial cultures will identify Bordetella.
Question:
What are the two main viruses causing upper respiratory disease in cats? (Answers are provided at the end of the chapter).
Question:
Describe two reasons that viral upper respiratory infections of cats cause chronic disease. (Answers are provided at the end of the chapter).
Question:
Briefly explain the mechanism by which Feline herpesvirus-1 leads to failure of lung defences and secondary bronchopneumonia. (Answers are provided at the end of the chapter).
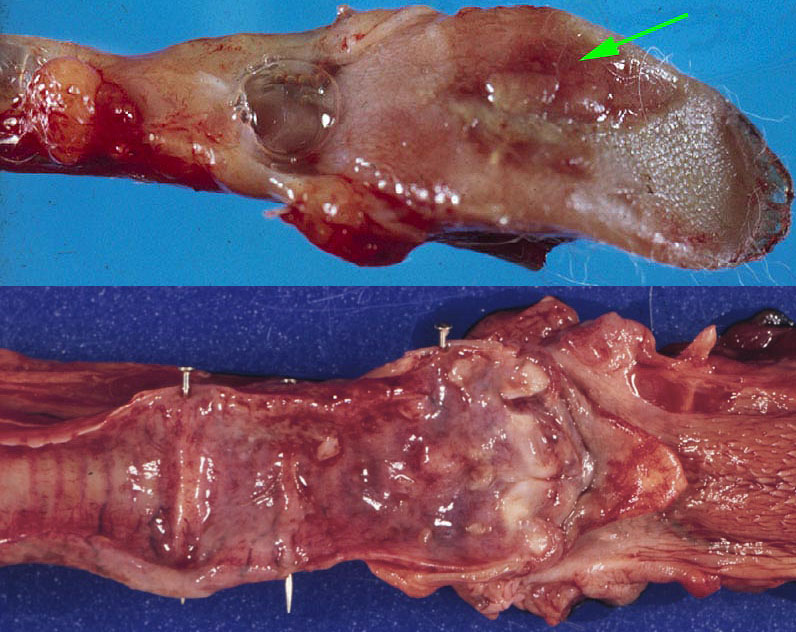
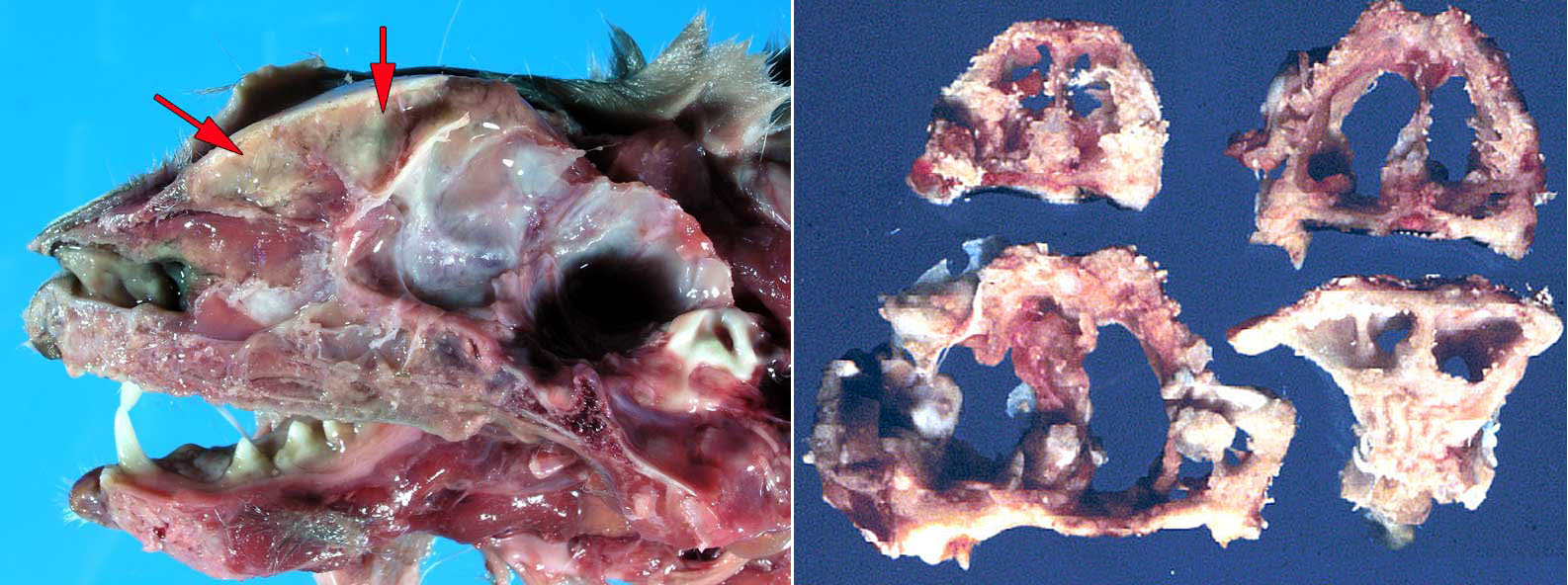
AUDITORY polyp
Auditory (nasopharyngeal) polyp is a common condition in young adult cats. The polyp typically arises in the middle ear or auditory (Eustachian) tube. It grows into the pharynx to cause gagging or dysphagia, or into the nasal cavity to cause stertor and nasal discharge, or into the middle ear to cause head tilt, head shaking, or Horner’s syndrome. It is important to distinguish this common condition of young cats from neoplasia.
Question:
What is the most common nasal mass in young cats? (Answers are provided at the end of the chapter).
Nasal neoplasia
The major nasal neoplasms of cats are primary nasal lymphoma and adenocarcinoma, in addition to squamous cell carcinoma and other tumours of the nasal planum. Sinonasal lymphoma typically begins in the nasal cavity (rather than arising elsewhere and spreading to nasal tissues). It remains localized to the nasal cavity in some cases, and in others it can spread to distant tissues.
Nasal neoplasia is covered in more detail in the sections on General pathology, and Diseases of dogs.

Nasal cryptococcosis
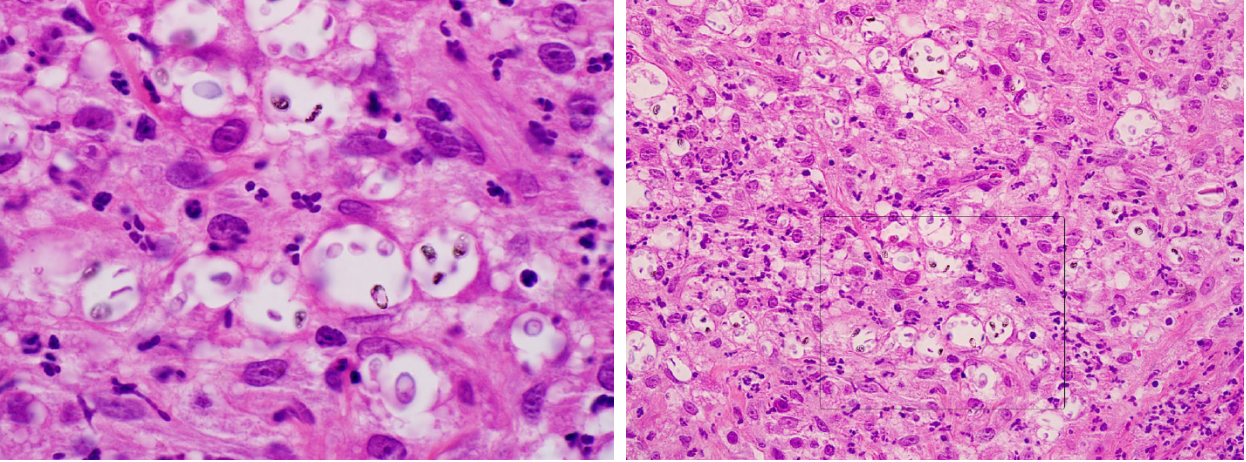
Cryptococcus neoformans is a fungus that is maintained in avian feces, and infects many mammalian species including cats, less commonly dogs, and humans. Cryptococcus gattii is an important pathogen of wild and domestic animals and humans in British Columbia, but is not found in Ontario. Cryptococcus has a thick capsule that invokes very little inflammation, so the gross lesions appear as a gooey gelatinous mass of yeast bodies. Infections are usually sporadic, and are typically not contagious or zoonotic.
Infection is mainly by inhalation, leading to nasal disease. The fungus can invade from the nasal cavity through the cribriform plate to cause meningoencephalitis. Aspiration of infected nasal mucus may cause pneumonia. In immunosuppressed individuals, hematogenous spread results in ulcerating cutaneous nodules, uveitis, or lesions in the viscera.
Diagnosis depends on identifying the organism cytologically in aspirates or impression smears, or histologically in affected tissues.

Question:
How does the microscopic appearance of Cryptococcus differ from Blastomyces? (Answers are provided at the end of the chapter).
Question:
What respiratory infection of cats is most likely to result from immunosuppression? (Answers are provided at the end of the chapter).
Chronic bronchitis and asthma
These conditions most likely represent a chronic hypersensitivity response. Some define chronic bronchitis as more or less constant respiratory disease due to airway obstruction from chronic bronchial inflammation, whereas asthma is characterized by episodes of disease separated by periods of health (similar to asthma in humans). In humans, viral or bacterial infections play a role in exacerbations of chronic obstructive pulmonary disease, but the role of infections in exacerbations of chronic bronchitis and asthma in cats is not known.
Clinical signs include cough, wheeze, or dyspnea, as a result of increased airway resistance due to bronchoconstriction. The diagnosis is usually based on clinical findings.
In most cases, eosinophilic inflammation affects the bronchi and/or bronchioles, and there is goblet cell hyperplasia and increased mucus secretion. Airway obstruction is the result of bronchoconstriction, obstruction of airways by mucus and inflammatory cells, and edema of the airway wall.
Bacterial bronchopneumonia
Bacterial pneumonia is often secondary to upper respiratory infections. The major causes include Pasteurella multocida and Bordetella bronchiseptica. Bordetella seems to cause outbreaks in groups of cats, suggesting that it may act as a primary pathogen. The morphology of bronchopneumonia in cats is similar to that in other species.
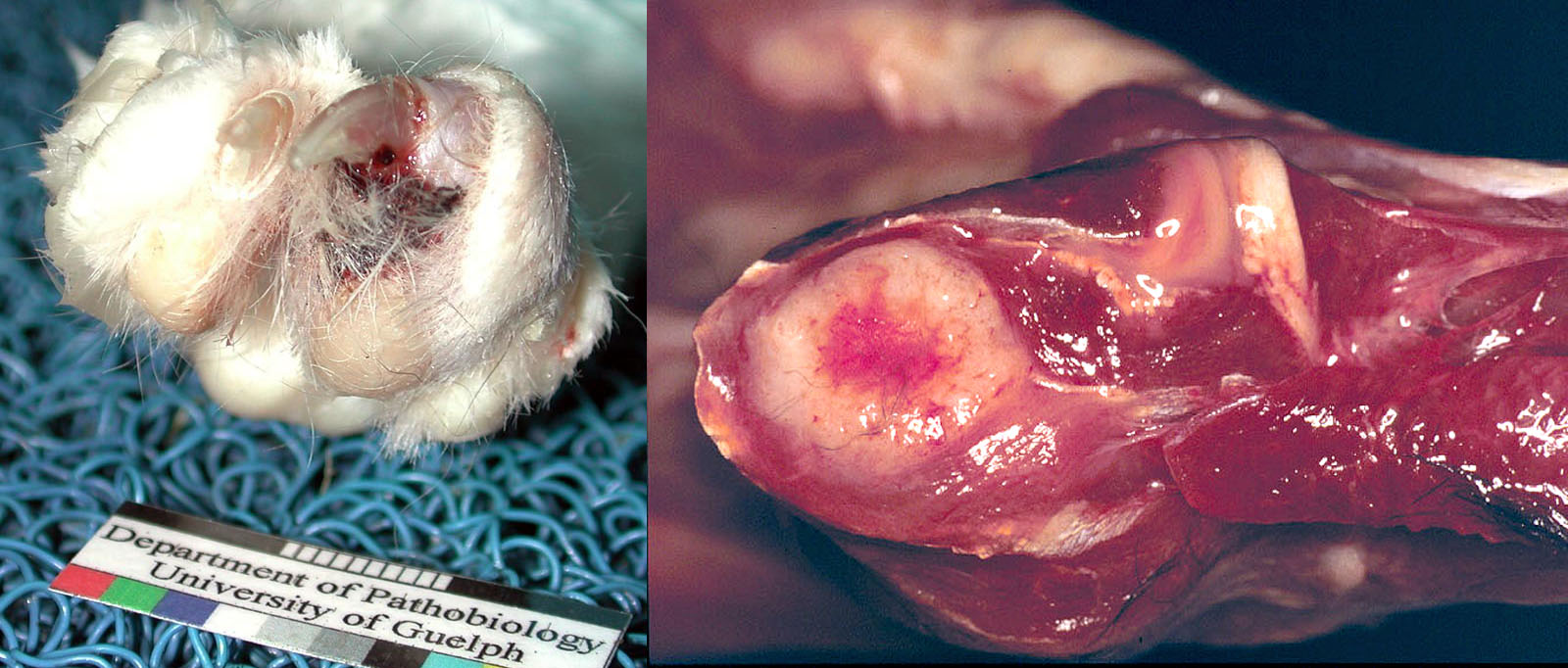
Pulmonary neoplasia
Pulmonary adenocarcinoma is a fairly common tumour in cats. It forms a focal lung mass, but frequently develops innumerable tiny metastases throughout the lung, or disseminates within the pleural cavity. Distant metastasis is frequent and targets unusual locations: footpad, skeletal muscle, bone, eye, brain, or skin. Some cats develop clinical signs referable to the presence of a pulmonary mass. Others show no evidence of respiratory disease but instead present for signs relating to the metastasis, such as lameness due to metastasis to a digit or to muscle.
Common neoplasms that metastasize to the lung of cats include lymphosarcoma, mammary carcinoma, and oral squamous cell carcinoma.
Question:
What is the name/type and expected behaviour of the most common lung tumour of cats? (Answers are provided at the end of the chapter).
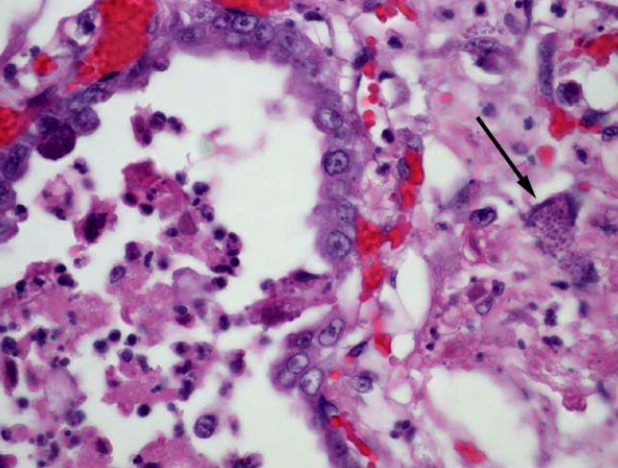
Toxoplasmosis
Toxoplasma gondii is an apicomplexan protozoan. Cats are the definitive host (they pass oocysts in feces). Disease occurs in cats, sheep, dogs, humans, and others. Infection is by ingestion of oocysts containing sporozoites (from contamination with cat feces), by ingestion of tissues of an intermediate host which contain bradyzoites, or by congenital infection. Asexual replication within host cells results in either release of tachyzoites by rupture of the cell (resulting in necrosis of tissue and
infection of adjacent cells), or formation of cysts containing bradyzoites that are infectious if ingested.
Cell-mediated immunity plays an important role in limiting protozoal replication, and disease occurs in animals that are immunosuppressed by infection (FeLV or FIV in cats, canine distemper in dogs) or by therapy (corticosteroids or other immunosuppressive drugs).
Clinical signs are highly variable and may include respiratory, nervous, hepatic, pancreatic, cardiac, ocular, muscular, and/or enteric disease.
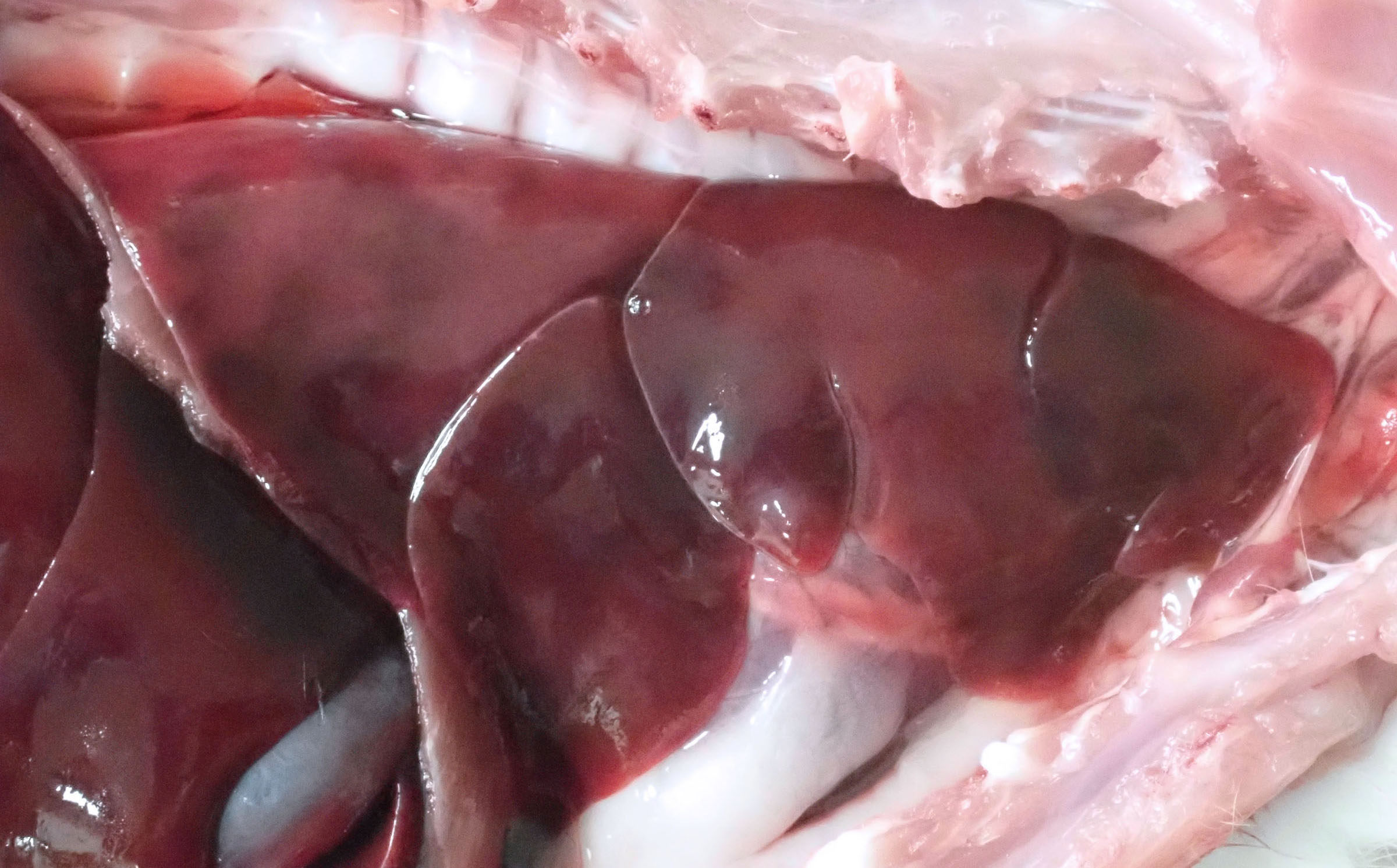
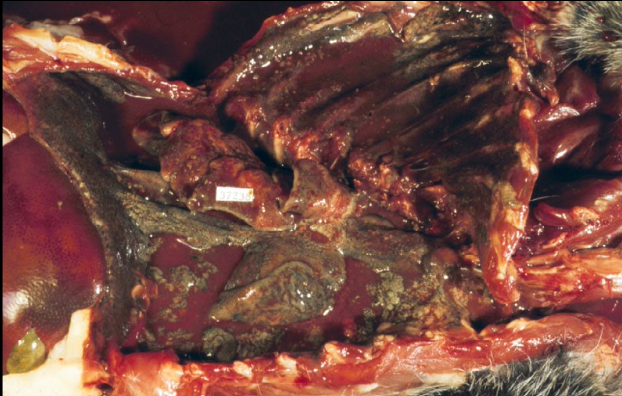
Lesions in the lungs are of diffuse interstitial pneumonia. The lungs are edematous, heavy, fail to collapse, diffusely firm and red. Other lesions include multifocal necrosis and inflammation in liver, heart, brain, muscle, and pancreas.
Question:
What 2 histologic lesions are expected with chronic interstitial lung disease in cats? (Answers are provided at the end of the chapter).
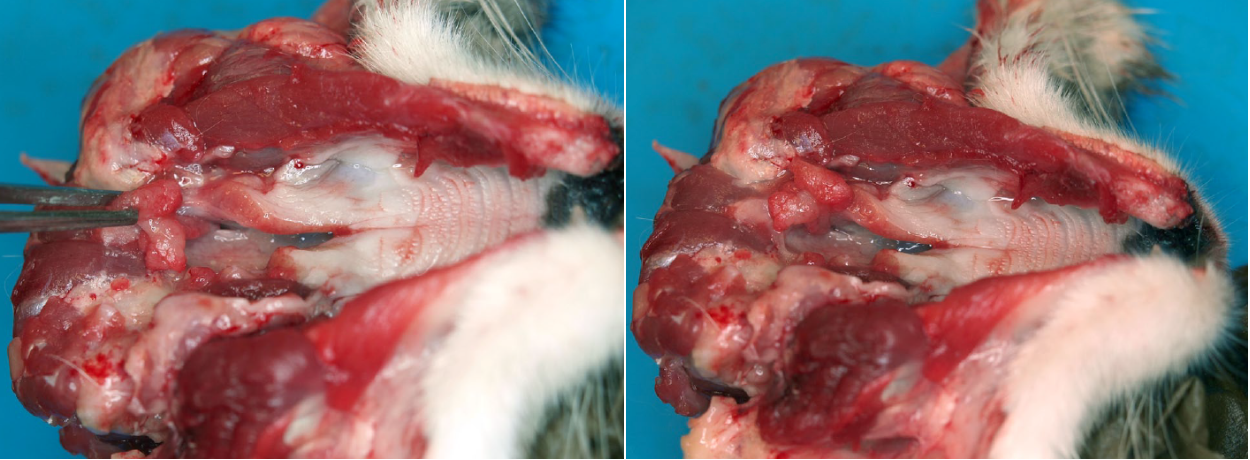
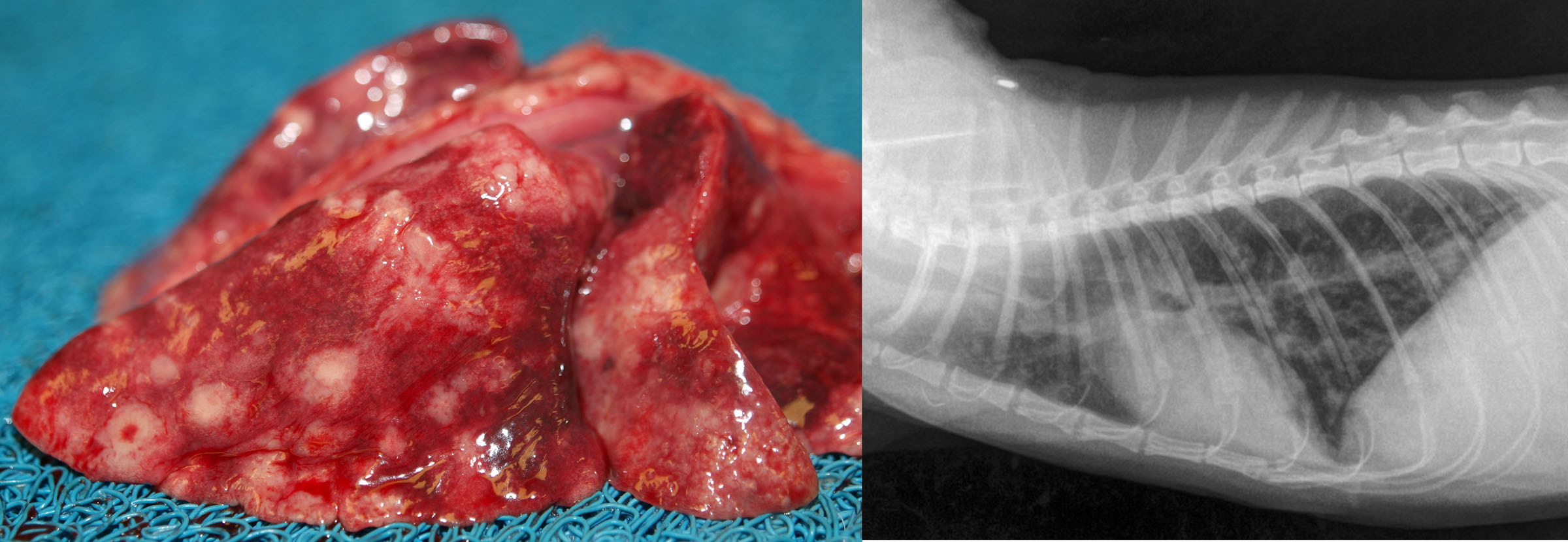
Aelurostrongylus abstrusus
Infection with this nematode is common in young cats with access to the snail or slug intermediate hosts, but this does not often cause clinical signs. It is reportedly the most common cause of anesthetic death when spaying/neutering humane society cats.
The gross appearance is of soft 2-5 mm diameter nodules beneath the pleura of the dorsal lung. The worms are too tiny to be seen grossly, but each nodule contains microscopic adults, larvae and eggs, and a granulomatous inflammatory response.
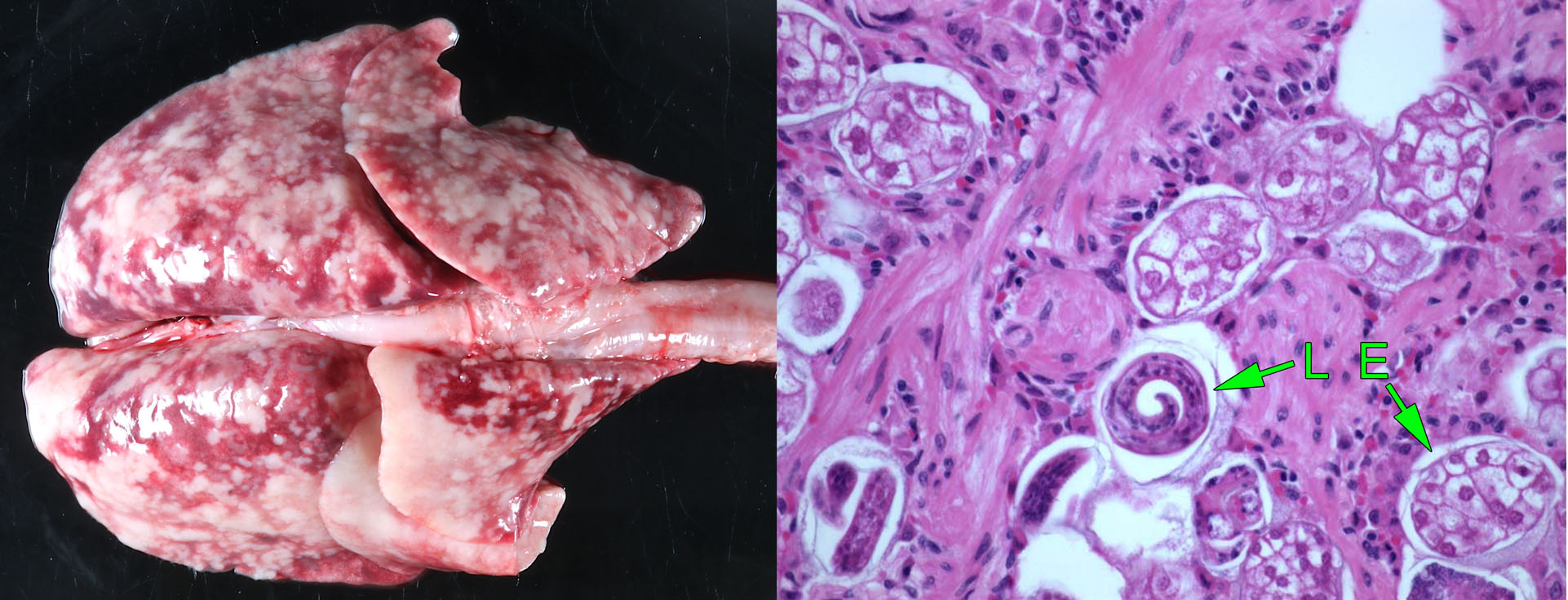
Paragonimus kellicotti
This trematode (fluke) parasite is acquired from crayfish intermediate host or from a paratenic host.
The adult flukes and their pigmented eggs reside in cyst-like cavitations in the lung. The cat’s illness is the crayfish’s revenge, although in truth most infected cats have no clinical signs. However, the infection can be significant in two ways:
- The cyst can be mistaken radiographically for a neoplasm, leading to unnecessary euthanasia.
- Rupture of the cysts causes pneumothorax with acute dyspnea.
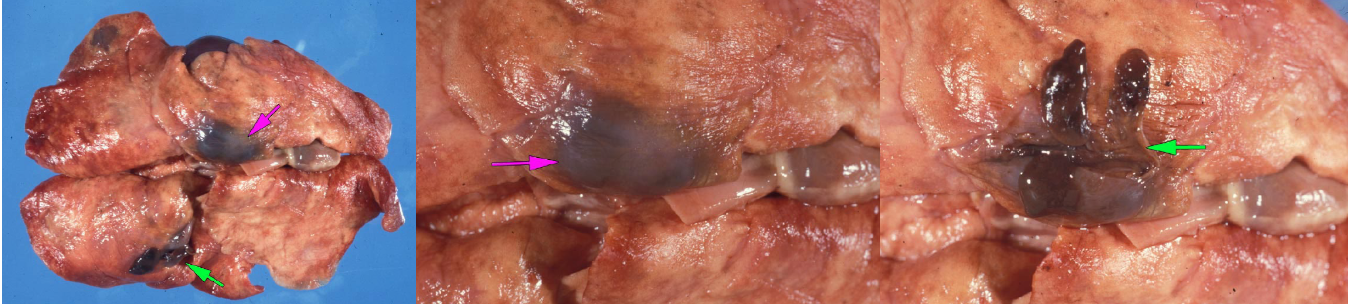
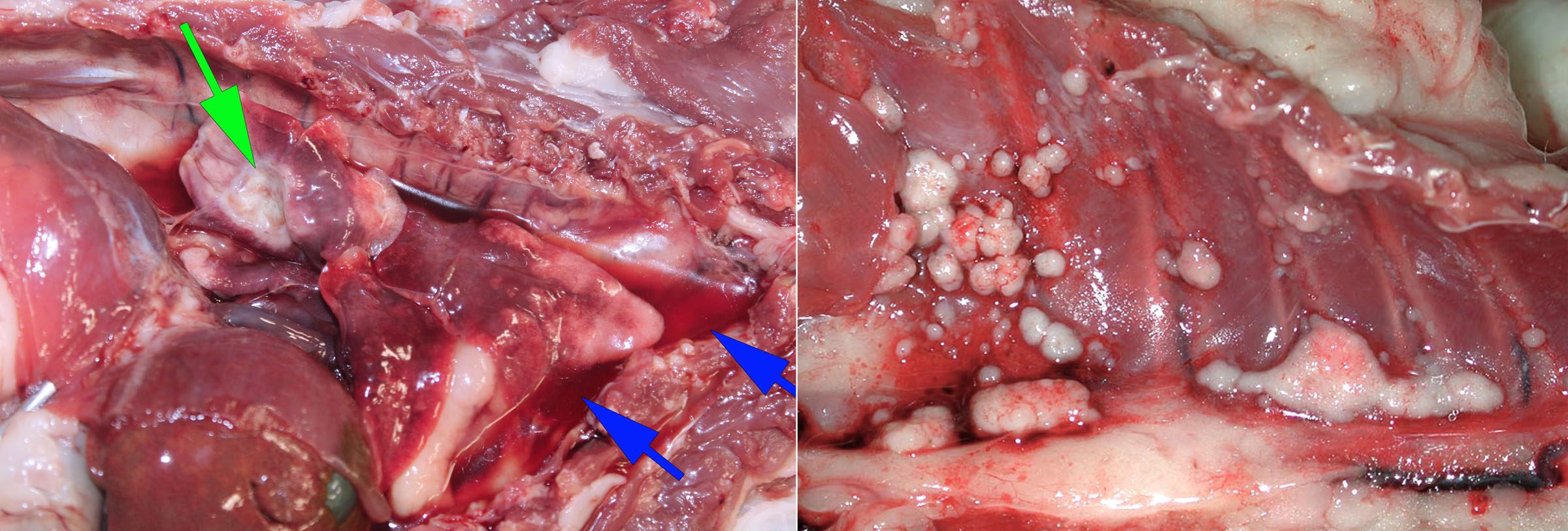
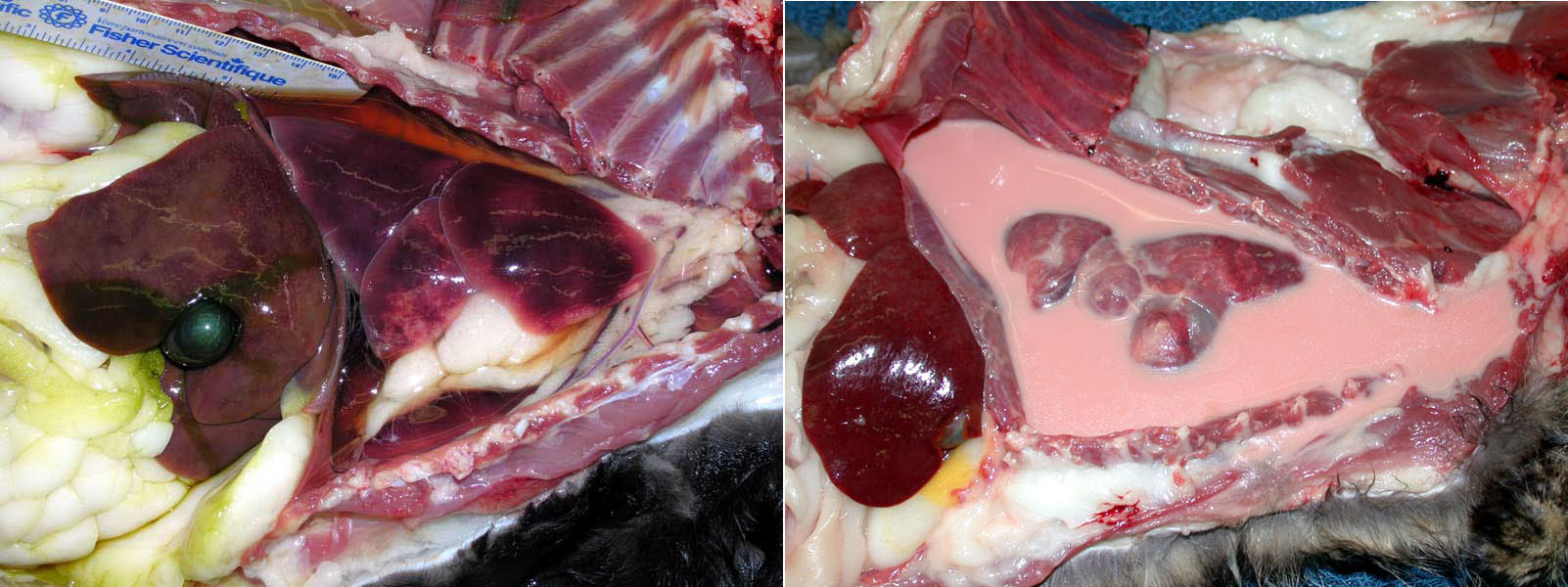
Feline infectious peritonitis (FIP)
Peritonitis, nephritis and lymphadenitis are common manifestations, but some cats with FIP have pleuritis with or without lesions in other tissues.
In all cats with pleural FIP, dry or wet form, tiny raised white granulomas are present on the pleural surface of the lung.
In the wet form, cloudy, protein-rich fluid fills the pleural cavity. This exudate is difficult to grossly distinguish from bacterial pleuritis, but granulomas on the pleural surface suggest a diagnosis of FIP.

Pyothorax
Penetrating injuries—such as cat bites— contaminate the pleural cavity with bacteria such as Pasteurella multocida, and elicit a suppurative inflammatory response that fills the pleural cavity with cloudy fluid.
Chylothorax
Chylothorax is accumulation of lymph fluid in the chest, with a characteristically high lymphocyte count and high triglyceride concentration compared to serum. The causes include:
- Heart failure, because increased central venous pressure reduces drainage from thoracic duct into vena cava. Hypertrophic cardiomyopathy is the most common heart disease causing chylothorax.
- Mediastinal masses (thymic lymphoma, thymoma).
- Thrombosis of the vena cava.
- Many cases are idiopathic.
Hydrothorax
Hydrothorax appears as clear, low-protein fluid in the chest, and is most commonly the result of right- or left-sided heart failure.
Question:
Some people speculate that chronic inhalation of kitty litter might contribute to idiopathic pulmonary fibrosis (chronic interstitial lung disease) of cats. What term is applied to lung disease due to inhalation of inorganic dust? (Answers are provided at the end of the chapter).
Question:
What is the most likely cause in a cat with fibrinous pleuritis, plaques of fibrin on the intestines, and foci of necrosis in the kidney? (Answers are provided at the end of the chapter).
Question:
What is the name of the parasite that causes cyst-like nodules in the lung of cats? (Answers are provided at the end of the chapter).
Question:
What is the name and gross appearance of the common nematode lungworm of cats? (Answers are provided at the end of the chapter).
Answer:
What are the two main viruses causing upper respiratory disease in cats?
Feline herpesvirus-1.
Feline calicivirus.
Answer:
Describe two reasons that viral upper respiratory infections of cats cause chronic disease.
Chronic viral infection (FHV-1 latency/recrudescence, persistent calicivirus infection); tissue remodelling impairs nasal defences; chronic sinusitis or osteomyelitis.
Answer:
Briefly explain the mechanism by which feline herpesvirus leads to failure of lung defences and secondary bronchopneumonia.
Destruction of ciliated epithelium, failure of mucociliary clearance.
Answer:
What is the most common nasal mass in young cats?
Nasopharyngeal polyp. Adenocarcinoma and lymphoma would be more frequent in older cats.
Answer:
How does the microscopic appearance of Cryptococcus differ from Blastomyces?
Cryptococcus: most isolates have a tiny cell surrounded by a thick capsule.
Blastomyces: larger, no capsule, thick cell wall.
Answer:
What respiratory infection of cats is most likely to result from immunosuppression?
Cryptococcus.
Answer:
What is the name/type and expected behaviour of the most common lung tumour of cats?
Adenocarcinoma, metastasis to footpads or other sites.
Answer:
What 2 histologic lesions are expected with chronic interstitial lung disease in cats?
Fibrosis of alveolar septa, proliferation of type II pneumocytes (the same as for other species).
Answer:
Some people speculate that chronic inhalation of kitty litter might contribute to idiopathic pulmonary fibrosis (chronic interstitial lung disease) of cats. What term is applied to lung disease due to inhalation of inorganic dust?
Pneumoconiosis.
Answer:
What is the most likely cause in a cat with fibrinous pleuritis, plaques of fibrin on the intestines, and foci of necrosis in the kidney?
Feline infectious peritonitis (coronavirus).
Answer:
What is the name of the parasite that causes cyst-like nodules in the lung of cats?
Paragonimus kellicotti
Answer:
What is the name and gross appearance of the common nematode lungworm of cats?
Aleurostrongylus abstrusus, soft nodules, generalized or dorsocaudal distribution.

