Oral Histology
What is Histology?
Histology is the study of body tissues—groups of cells that are specialized for a specific body function. For a specimen from a particular organ to be studied histologically, it must be subjected to several preliminary steps: It is fixed (preserved), sliced into very thin layers, placed it on a microscopic slide, and stained. Now, using a microscope, the histologist can differentiate tissues from the lung and the kidney, for example.
This is very important when a biopsy has been obtained from a suspected tumor. Colon cancer, for example, can travel (metastasize) to distant organs such as the liver. If the colon cancer has not been diagnosed but an x-ray of the abdomen shows a suspicious area in the liver, a biopsy of the liver is ordered. Detection of cells from the colon in the liver biopsy specimen proves that the patient has metastatic colon cancer that has reached the liver, and the physician can proceed to identify where the primary tumor originated in the colon and prescribe treatment.
Anatomical vs. Clinical Crown
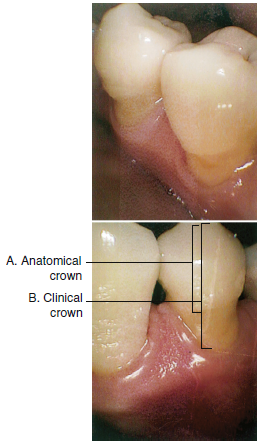
Two terms that often confuse dental assisting students are the anatomical crown and the clinical crown. The concept is very simple: the anatomical crown of the tooth is that part of the tooth that is covered by enamel and remains the same and the clinical crown of the tooth is that part of the tooth that is visible in the mouth and may vary because of changes in the position of the gingiva.
The clinical crown and the anatomic crown can be the same if the cementoenamel junction (CEJ) of the tooth is at the gingival margin. In the case of gingival recession, the clinical crown will be larger than the anatomic crown because some of the cementum-covered root extends beyond the gingival margin.
For an extended period after eruption, the gingiva covers a portion of the anatomic crown. In this case, the clinical crown is smaller than the anatomic crown. Below is an image of teeth indicating the difference between an anatomical crown and a clinical crown.
The Tooth Root
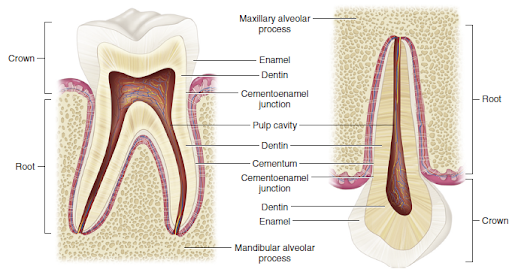
All teeth have at least one and often more than one root. The root is covered by cementum and embedded in the alveolar process. Between the bone of the alveolar process and the cementum is the periodontal ligament, which suspends the tooth and provides it with nourishment.
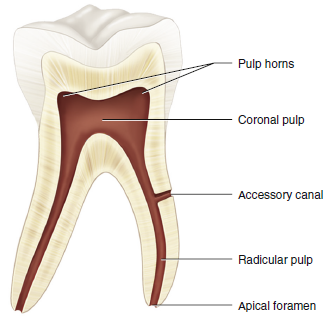
The end of the root is called its apex; the hole in the apex through which blood, lymph vessels, and nerves pass is called the apical foramen. The term apical is used to describe something that has to do with the apex. A dentist who notes that the patient’s gingiva is receding apically means that the gum tissue is moving along the tooth toward the apex of the root.
What’s the opposite of apical? Structures associated with the tooth’s crown are termed coronal. Here’s how to use it in a sentence: “The endodontist removed the coronal pulp tissue first from the patient’s painful molar.”
Finally, the term radicular means “having to do with the tooth root.” The radicular pulp is the pulp contained in the root.
Tissues of the Tooth
Activity 1: Histology Terminology
Enamel
As we learned in Module 1, the enamel that covers the anatomic crown is produced by the ameloblasts of the enamel organ. The ameloblasts don’t remain after enamel production is complete, meaning that new enamel can’t be formed later when needed. Dentin, on the other hand, is continually produced throughout life.
Enamel is overwhelmingly composed of the mineral calcium hydroxyapatite (~96%) with only a small amount of organic matrix (think of this as tissue fibers). The enamel is translucent and allows the color of the underlying dentin to show through to a varying degree, depending on the thickness of the enamel. Here are some interesting histologic features of enamel:
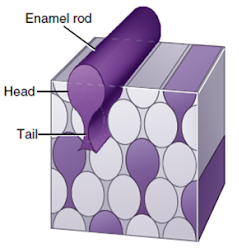
Enamel prisms (or rods) are very small key-shaped structures that extend from the dentin to the surface of the enamel. Millions of prisms are tightly packed together with small amounts of weak interprismatic substance (containing organic matrix) between them. Each enamel rod is surrounded by a very thin prism sheath contained in an interprismatic substance.
Microscopic Features of Enamel
When viewed under a microscope, enamel has numerous features of interest, including:
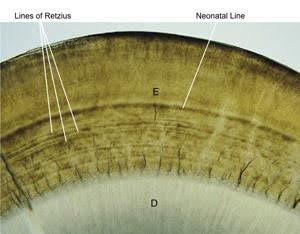
- Lines of Retzius – These alternating light and dark rings in the enamel appear like growth rings of a tree; they represent waves of enamel matrix apposition during tooth formation.
- Neonatal line – A very pronounced line of Retzius represents the shock of birth to the enamel production process.
- Enamel spindles – These spindles represent odontoblasts that have strayed into enamel-producing territory during apposition and become trapped.
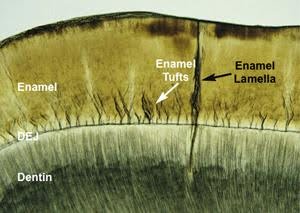
- Enamel tufts – These structures represent faulty mineralization in the area of the dentinoenamel junction (DEJ).
- Enamel lamellae – These sheets of poorly mineralized enamel extend from the DEJ to the surface of the tooth. The lamellae may represent weak areas of the enamel that could fracture from normal activity over time or as a result of trauma.
 |
 |
| A microscopic image showing a tooth’s enamel with the Lines of Retzius and the neonatal line labeled above the dentin layer. |
|
Dentin
Dentin is a hard, mineralized material that is most abundant in the tooth. It’s less mineralized (softer) than enamel but more mineralized (harder) than cementum. The coronal dentin is covered by enamel, which protects it; the radicular dentin is covered by cementum. The walls of the pulp chamber and root canals, formed by the innermost dentin of the tooth, are lined by odontoblasts.
Unlike enamel, dentin is a living tissue. It contains millions of dentinal tubules that extend from the DEJ to the pulp. Each dentinal tubule contains an extension of the odontoblast that produced it, as well as dentinal fluid and sensory nerves. The odontoblasts continue to produce dentin throughout life, starting with primary dentin (produced before the formation of the apex), secondary dentin (produced after the formation of the apex), and tertiary dentin (produced in response to injury to the tooth, such as decay or traumatic injury). Tertiary dentin also called reparative dentin, is hastily produced and of poor quality compared to other dentin. Its purpose is further to separate the pulp of the tooth from the injury.
 |
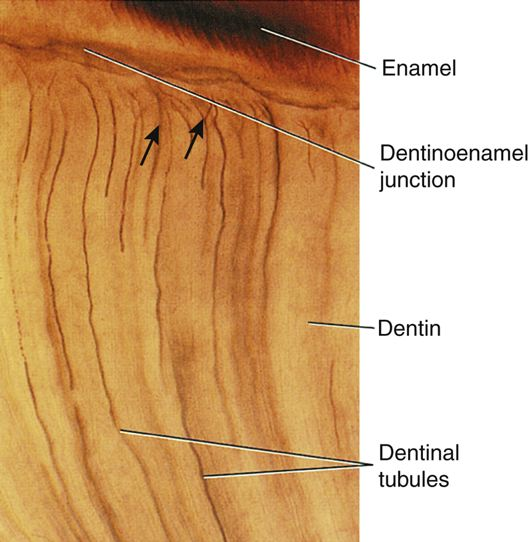 |
| A micrograph of dentin showing the dentinal tubules with odontoblastic processes, the layer of odontoblasts, and the adjacent pulp tissue. | A close-up image of a tooth section highlighting the enamel, the dentinoenamel junction, dentin, and the dentinal tubules. |
Cementum and Pulp
Cementum is formed by cementoblasts, which are attached to newly formed dentin beyond the enamel organ. It is softer than both enamel and dentin and its primary purpose is as an attachment material for the fibers of the periodontal ligament. Acellular (primary) cementum covers the whole root, whereas cellular (secondary) cementum is present on the apical third of the root and produces cementum throughout life. The cellular cementum is produced quickly, trapping cementoblasts within. These trapped cementoblasts are now called cementocytes. Hypercementosis is an overproduction of cementum at the tooth’s apex, often the result of a poor bite or grinding habit.
The coronal pulp, with its pulp horns that project into the cusps and incisal edges, and the radicular pulp are contained within dentin. The pulp tissue contains fibroblasts, blood vessels, lymph vessels, and nerves. As previously noted, the walls of the pulp chamber (and root canals) are lined with odontoblasts that continually produce dentin, thus shrinking the size of the pulp with age. The apical foramen is the portal of entry and exit for vessels and nerves to access the pulp.
Periodontium: Periodontal Ligament
The periodontium consists of three structures (cementum, periodontal ligament, and the alveolar bone) that support the teeth in their position in the arches. We’ve already discussed the cementum, so let’s turn our attention to the periodontal ligament.
The periodontal ligament (PDL) is connective tissue that is located between the alveolar socket and the tooth’s root. It consists of Sharpey’s fibers that are embedded in both the alveolar bone and the cementum and provide cushioning to the tooth during mastication. In addition to its support role, the periodontal ligament provides proprioception (information related to the position of a structure in space), nutrition, and repair functions for the teeth.
The PDL consists of numerous groups of fibers, including the periodontal fiber group (extending from alveolar bone to cementum), the transseptal fiber group (extending between adjacent teeth above the crest of the bone), and the gingival fiber group (extending from the cementum into the gingival tissues).
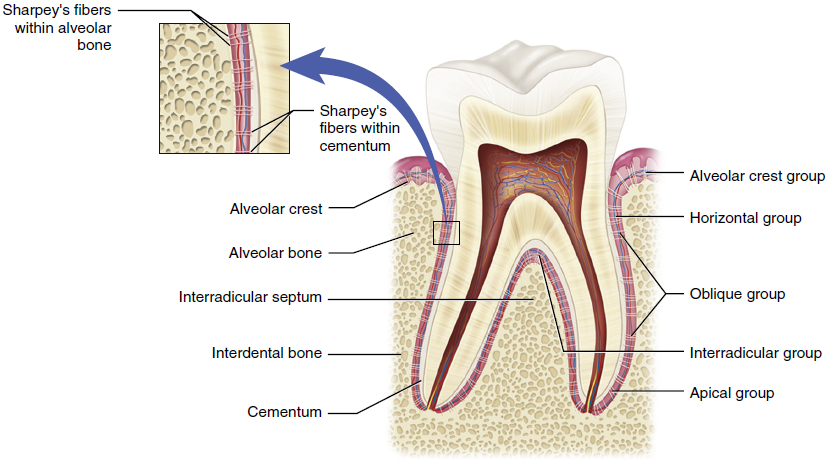
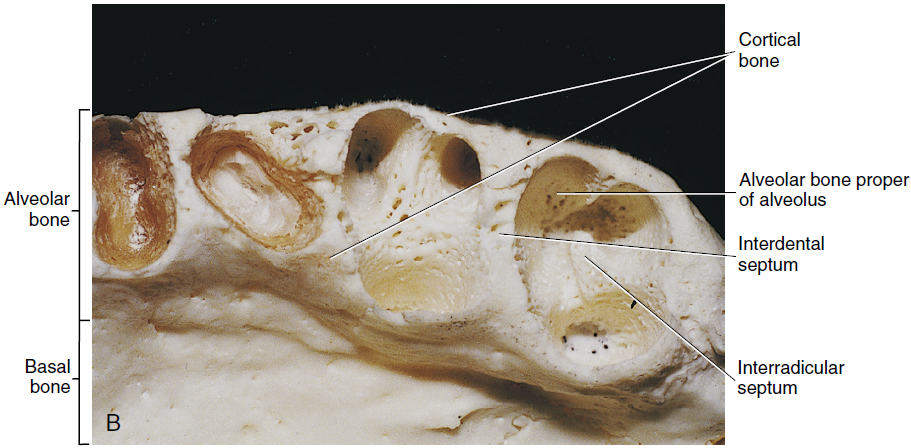
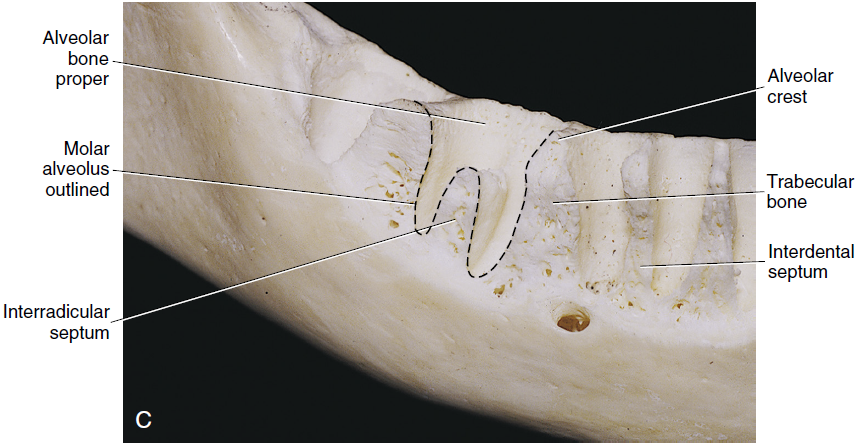
Periodontium: Alveolar Process
The alveolar processes are extensions of the dental arches that house the teeth. They have the following components:
- Cortical plate – This hard outer covering of the alveolar process protects the spongy inner bone.
- Alveolar crest – The farthest extension of the cortical plate is where facial and lingual cortical bone meets.
- Alveolar socket – This space within the alveolar process houses the roots of the teeth.
- Cribriform plate – This cortical bone lines the alveolar socket.
Radiographic examination of the periodontium provides an indication of health or disease. In the case of periodontal disease, for example, the alveolar crest becomes less pointed and more blunt.
 |
 |
 |
|
Mandibular arch with teeth removed |
||
Activity 2: Tissues of the Teeth
Gingival Unit
Oral mucosa almost continuously lines the oral cavity. It is composed of stratified squamous epithelium that overlies connective tissue. The oral mucosa is perforated in various regions of the oral cavity by the ducts of salivary glands.
There are three main types of oral mucosa in the oral cavity:
Mucosa
Click on the hotspots in the image below to see the A and B content.
Lining Mucosa
Lining mucosa is noted for its softer texture, moist surface, and ability to stretch and be compressed, thereby acting as a cushion for underlying structures. Lining mucosa covers the inside of the cheeks, vestibule, lips, soft palate, and ventral surface (underside) of the tongue. Because the lining mucosa is not firmly attached to bone, it can move freely. The lining mucosa is brighter red in colour due to the blood supply and thinness of the tissue.
Masticatory Mucosa
Masticatory mucosa is noted for its rubbery surface texture and resiliency. Masticatory mucosa includes the attached gingiva, hard palate, and dorsum (upper surface) of the tongue. Masticatory mucosa is light pink in colour and is keratinized, which means that it has a tough, protective outer layer. Beneath the masticatory mucosa is the submucosa. Masticatory mucosa is firmly attached to bone and it does not move.
Specialized Mucosa
On the top surface, or dorsal surface of the tongue, both masticatory mucosa and specialized mucosa are present in the form of lingual papillae. These papillae are associated with sensations of taste.
You have completed Module 2. Please return to Blackboard for the next steps.
Media Attributions
- Images from: Modern Dental Assisting, 13th and 14th Edition
Study of the structure and function of body tissues on a microscopic level.
Portion of the tooth that is covered with enamel.
The portion of the tooth that is visible in the oral cavity.
Area where enamel ends and the cementum begins.
Tapered end of each root tip.
Natural opening in the root.
Structures associated with the tooth's crown.
Chamber the space occupied by pulp.
Having to do with the tooth root.
Part of a developing tooth destined to produce enamel.
Mineral compound that is the principal inorganic component of bone and teeth.
Very small key-shaped structures that extend from the dentin to the surface of the enamel.
Incremental rings, similar to the growth rings on a tree that represent variations in the deposition of the enamel matrix during the formation of the tooth.
A very pronounced line of Retzius represents the shock of birth to the enamel production process.
The ends of odontoblasts (dentin-forming cells) that extend across the dentinoenamel junction a short distance into the enamel.
The hypocalcified or uncalcified ends of groups of enamel prisms that start at the dentinoenamel junction and may extend to the inner third of the enamel.
Thin, leaflike structures that extend from the enamel surface toward the dentinoenamel junction and consists of organic material with little mineral content.
Microscopic canals found in dentin.
Dentin that forms before eruption and that makes up the bulk of the tooth.
Dentin that forms after eruption and continues at a very slow rate throughout the life of the tooth.
Dentin that forms in response to irritation and appears as a localized deposit on the wall of the pulp chamber, so-called reparative dentin.
Is formed outward from the CEJ and covers the whole root.
Present on the apical third of the root and produces cementum throughout life.
An overproduction of cementum at the tooth's apex.
Structures that surround, support, and are attached to the teeth.
Tissues that anchor the periosteum to the bone.
Dense outer covering of spongy bone that makes up the central part of the alveolar process.
Highest point of the alveolar ridge.
Cavity within the alveolar process that surrounds the root of the tooth.
Cortical bone lines the alveolar socket.
Layers of flat, formed epithelium.
Mucous membrane that covers the inside of the cheeks, vestibule, lips, soft palate, and underside of the tongue and acts as a cushion for underlying structures.
Oral mucosa that covers the hard palate, dorsum of the tongue, and gingiva.
Mucous membrane on the tongue in the form of lingual papillae, which are structures associated with sensations of taste.

