Now that we have reviewed antimicrobial basics, we will take a closer look at specific antimicrobial classes and administration considerations, therapeutic effects, adverse effects, and specific teaching needed for each class of antimicrobials. But before we do that, let’s reexamine the importance of the nursing process in guiding the nurse who administers antimicrobial medications. The nursing process consists of assessment, diagnosis, outcome identification, planning, implementation of interventions, and evaluation. Because diagnosis, outcome identification, and planning are specifically tailored to the individual client, we will broadly discuss considerations related to assessment, implementation of interventions, and evaluation when administering antimicrobials.
Assessment
Although there are numerous details to consider when administering medications, it is always important to first think more broadly about what you are giving and why. As a nurse who is administering an antimicrobial, you must remember some important broad considerations.
First, let’s think of the WHY? Recognizing cues…
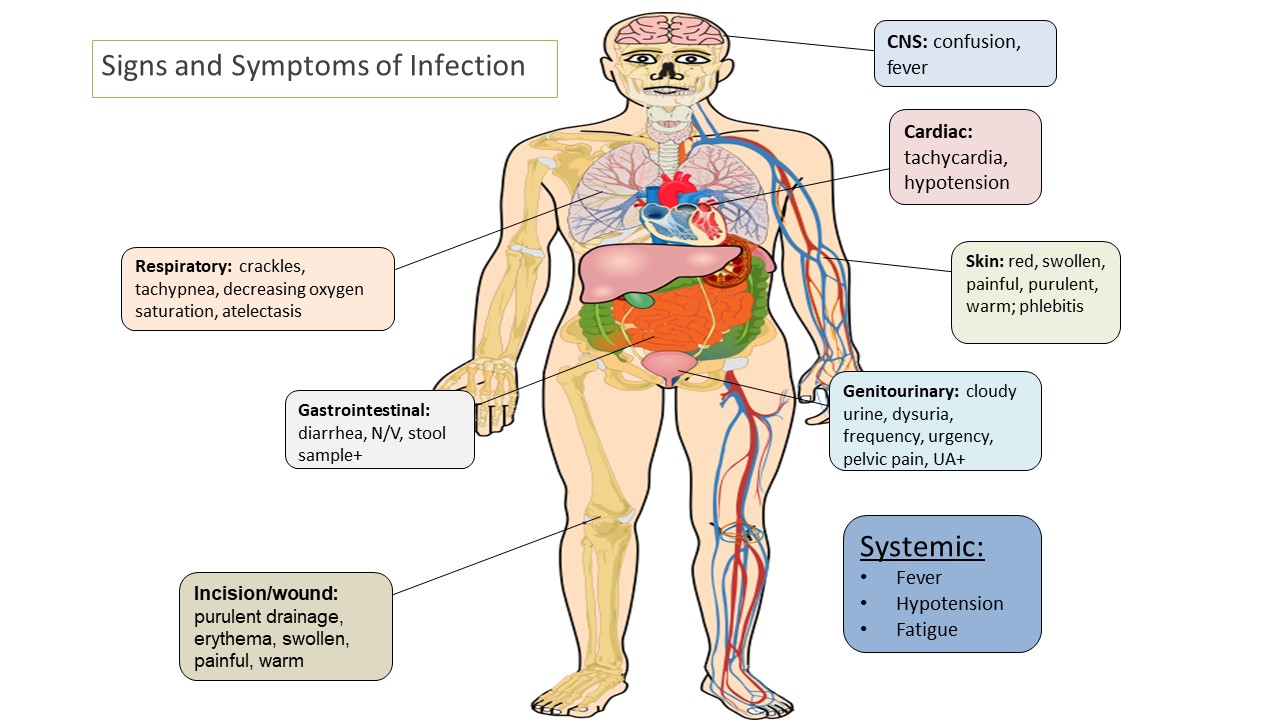
Antimicrobials are given to prevent or treat infection. If a client is prescribed an antimicrobial, an important piece of the nursing assessment is to recognize and analyze cues. The nurse should look for signs and symptoms of infection, and always know WHY the client is receiving an antimicrobial to effectively evaluate whether the client is improving or deteriorating. Remember, the nurse must assess how this medication is working, and having pre-administration assessment information is an important part of this process.
In order to define a baseline, typical data that a nurse collects at the start of a shift include:
- temperature
- heart rate
- blood pressure
- respiratory rate, and
- white blood cell count.
Focused assessments are then made based on the type of infection. For example, if it is a wound infection, the wound should be assessed for redness, inflammation, drainage type and amount, and pain. If it is a respiratory infection, the nurse should assess the client’s lung sounds, and type/consistency of respiratory expectorate. If a client has a urinary tract infection (UTI), the urine and symptoms related to a UTI (pain with urination, cloudy urine, foul-smelling urine) should be assessed.
The following image summarizes some common signs and symptoms of infection (by system) that a nurse needs to monitor for.
Additionally, whenever a client has an infection, it is important to continually monitor for the development of sepsis, a life-threatening condition caused by severe infection. As you recall from the previous chapter, early signs of sepsis include new-onset confusion, elevated heart rate, decreased blood pressure, increased respiratory rate, and elevated fever.
Additional baseline information to collect prior to the administration of any new medication order includes a client history, current medication use, including herbals or other supplements, and history of allergy or previous adverse response. Many clients with an allergy to one type of antimicrobial agent may experience cross-reactivity to other classes. This information should be appropriately communicated to the prescribing provider prior to the administration of any antimicrobial medication.
When a nurse has completed a thorough assessment, they are able to prioritize their concerns/hypotheses before implementing further intervention.
Interventions
With administration of the antimicrobial medication, it is important for the nurse to anticipate any additional interventions associated with the medications. For example, antimicrobials often cause gastrointestinal upset (GI) such as nausea, diarrhea, etc. The nurse may need to refine their assessments and interventions, accordingly. The client should be educated about these potential side effects, and proper interventions should be taken to minimize these occurrences. For example, the nurse may instruct the client to take certain antimicrobials with food to diminish the chance of GI upset, whereas other medications should be taken on an empty stomach for optimal absorption.
Hypersensitivity/allergic reactions are always a potential adverse reaction, especially when administering the first dose of a new antibiotic, and the nurse should monitor closely for these symptoms and respond appropriately by immediately notifying the prescriber. Hypersensitivity reactions are immune responses that are exaggerated or inappropriate to an antigen and can range from itching to anaphylaxis. Anaphylaxis is a medical emergency that can cause life-threatening respiratory failure. Early signs of anaphylaxis include, but are not limited to, hives and itching, the feeling of a swollen tongue or throat, shortness of breath, dizziness, and low blood pressure.
Evaluation
Finally, it is important to always evaluate the client’s response to a medication. With antimicrobial medications, the nurse should assess for the absence of or decreasing signs of infection, indicating the client is improving. It is important to document these findings to reflect the client’s trended response.
Additionally, it is also important for the nurse to promptly identify and communicate signs of worsening infection to the provider. For example, increasing white blood cell count, temperature, heart rate, and respiratory rate may indicate that the client’s body is experiencing a life-threatening response to the infection. These signs of worsening clinical assessment require prompt intervention to prevent further clinical deterioration. Additionally, clients receiving antibiotics should be closely monitored for developing a complication called “C. diff,” resulting in frequent, foul-smelling stools. C. diff stands for Clostridioides difficile, which is a spore-forming, gram-positive bacterium that colonizes the human intestinal tract after the normal gut flora has been disrupted (frequently in association with antibiotic therapy). C. diff is one of the most common health care-associated infections and a significant cause of morbidity and mortality, especially among older adult hospitalized clients. Management of C-diff requires the implementation of modified contact precautions, including the use of soap and water, not hand sanitizer (as this does not kill the spores), as well as antibiotic therapy. [1]
Image Description
Figure 3.4 Summary of common signs and symptoms of infection: A diagram showing a cartoon version of a human body. This diagram gives an internal view of the body, including organs, veins and arteries, and bones. Indicating various points on the body, this diagram lists common signs and symptoms of infection based on where in the body they can originate. These include:
- Respiratory (lungs): crackles, tachypnea, decreasing oxygen saturation, atelectasis.
- Gastrointestinal (digestive system): diarrhea, N/V (nausea and vomiting), stool sample positive.
- Incision/wound: purulent drainage, erythema, swollen, painful, warm.
- Central nervous system (brain): confusion, fever.
- Cardiac (heart): tachycardia, hypotension.
- Skin: red, swollen, painful, purulent, warm; phlebitis.
- Genitourinary (bladder): cloudy urine, dysuria, frequency, urgency, pelvic pain, urinalysis positive.
- Systemic: fever, hypotension, fatigue.
- Kelly, C.P., Lamon, J.T., & Bakken, J.S. (2019). Clostridioides (formerly Clostridium) difficile infection in adults: Treatment and prevention. UpToDate. Retrieved on July 8, 2019, from https://www.uptodate.com/contents/clostridioides-formerly-clostridium-difficile-infection-in-adults-treatment-and-prevention?search=Clostridioides%20(formerly%20Clostridium)%20difficile%20infection%20in%20adults&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 ↵

