Thyroid Basics: A&P Review
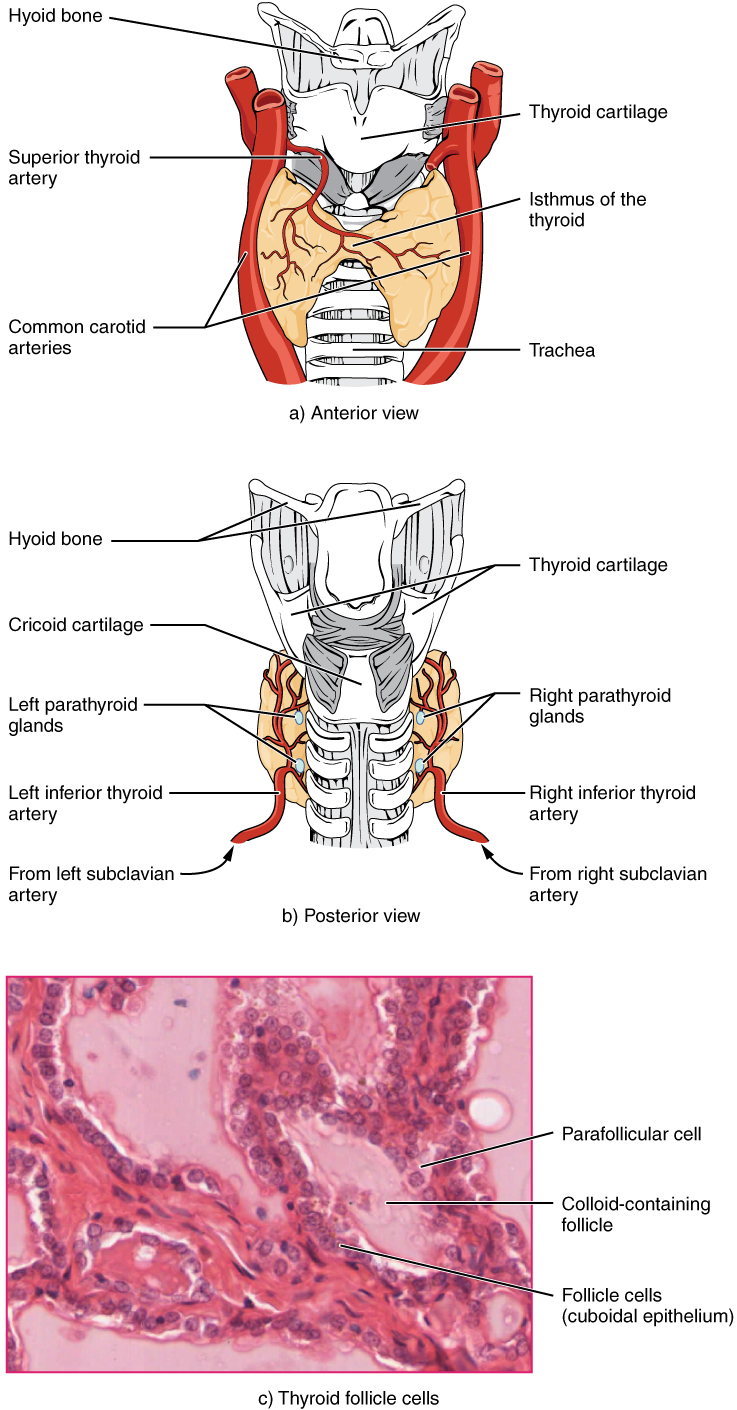
The thyroid is a butterfly-shaped organ located anterior to the trachea, just inferior to the larynx (see Figure 9.6a).[1] Each of the thyroid lobes is embedded with parathyroid glands.
Synthesis and Release of Thyroid Hormones
Thyroid hormone production is dependent on the hormone’s essential component: iodine. T3 and T4 hormones are produced when iodine attaches to a glycoprotein called thyroglobulin. The following steps outline the hormone’s assembly: Binding of TSH to thyroid receptors causes the cells to actively transport iodide ions across their cell membrane from the bloodstream. As a result, the concentration of iodide ions “trapped” in the thyroid cells is many times higher than the concentration in the bloodstream. The iodide ions undergo oxidation (i.e., their negatively charged electrons are removed) and enzymes link the iodine to tyrosine to produce triiodothyronine (T3), a thyroid hormone with three iodines, or thyroxine (T4), a thyroid hormone with four iodines. These hormones remain in the thyroid follicles until TSH stimulates the release of free T3 and T4 into the bloodstream. In the bloodstream, less than one percent of the circulating T3 and T4 remains unbound. This free T3 and T4 can cross the lipid bilayer of cell membranes and be taken up by cells. The remaining 99 percent of circulating T3 and T4 is bound to specialized transport proteins called thyroxine-binding globulins (TBGs), to albumin, or to other plasma proteins. This “packaging” prevents their free diffusion into body cells. When blood levels of T3 and T4 begin to decline, bound T3 and T4 are released from these plasma proteins and readily cross the membrane of target cells. T3 is more potent than T4, and many cells convert T4 to T3 through the removal of an iodine atom.
Regulation of Thyroid Hormone Synthesis
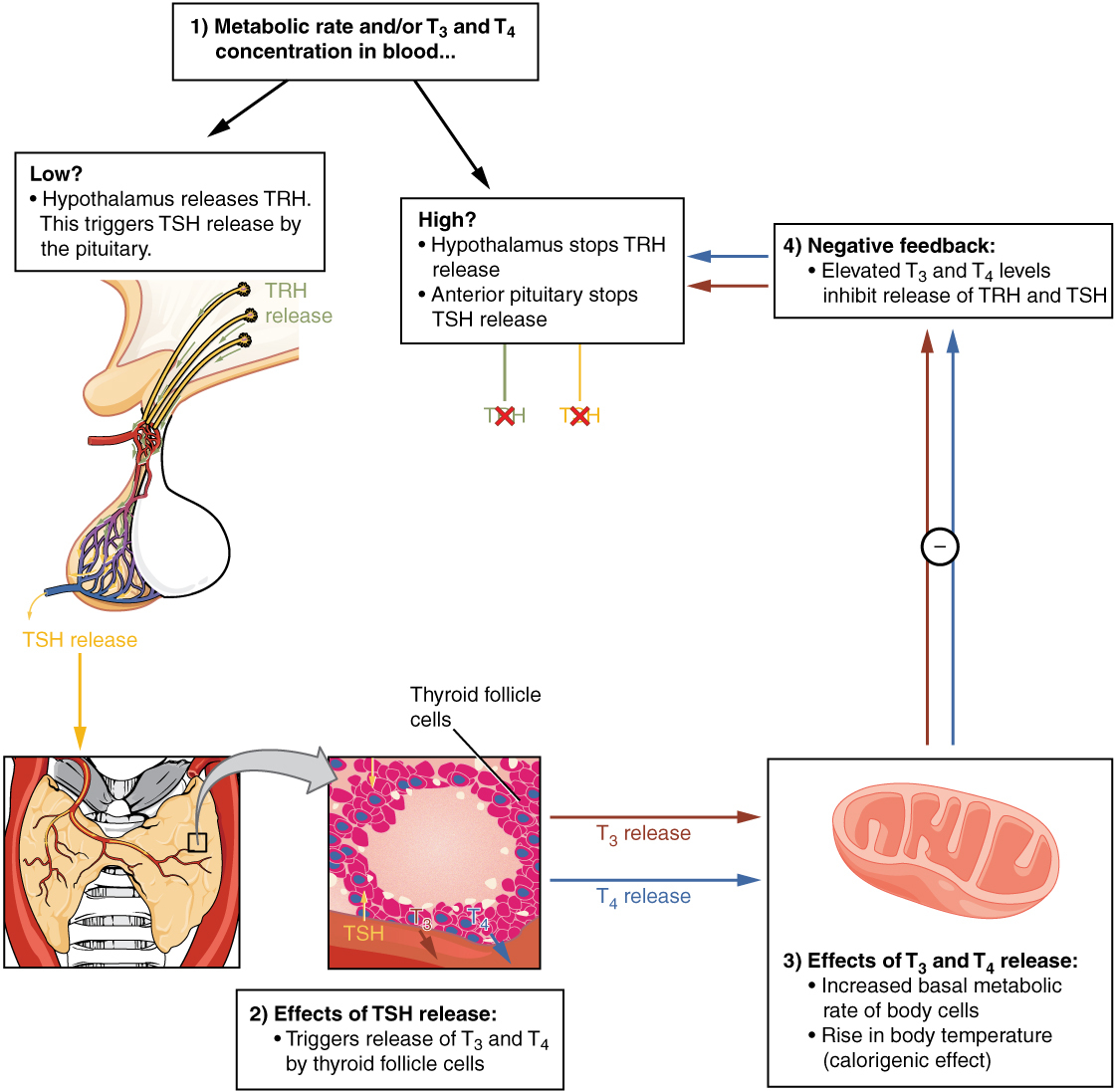
A negative feedback loop controls the regulation of thyroid hormone levels. As shown in Figure 9.6b,[2] low blood levels of T3 and T4 stimulate the release of thyrotropin-releasing hormone (TRH) from the hypothalamus, which triggers secretion of TSH from the anterior pituitary. In turn, TSH stimulates the thyroid gland to secrete T3 and T4. The levels of TRH, TSH, T3, and T4 are regulated by a negative feedback system in which increasing levels of T3 and T4 decrease the production and secretion of TSH.
Functions of Thyroid Hormones
The thyroid hormones T3 and T4 are often referred to as metabolic hormones because their levels influence the body’s basal metabolic rate, which is the amount of energy used by the body at rest. When T3 and T4 bind to intracellular receptors located on the mitochondria, they cause an increase in nutrient breakdown and the use of oxygen to produce ATP. In addition, T3 and T4 initiate the transcription of genes involved in glucose oxidation. Although these mechanisms prompt cells to produce more ATP, the process is inefficient, and an abnormally increased level of heat is released as a byproduct of these reactions. This calorigenic effect (calor- = “heat”) raises body temperature.
Adequate levels of thyroid hormones are also required for protein synthesis and for fetal and childhood tissue development and growth. They are especially critical for normal development of the nervous system both in utero and in early childhood, and they continue to support neurological function in adults. Thyroid hormones also have a complex interrelationship with reproductive hormones, and deficiencies can influence libido, fertility, and other aspects of reproductive function. Finally, thyroid hormones increase the body’s sensitivity to catecholamines (epinephrine and norepinephrine) from the adrenal medulla by upregulation of receptors in the blood vessels. When levels of T3 and T4 hormones are excessive, this effect accelerates the heart rate, strengthens the heartbeat, and increases blood pressure. Because thyroid hormones regulate metabolism, heat production, protein synthesis, and many other body functions, thyroid disorders can have severe and widespread consequences.
Disorders of the Thyroid Gland: Iodine Deficiency, Hypothyroidism, and Hyperthyroidism
As discussed above, dietary iodine is required for the synthesis of T3 and T4. For much of the world’s population, foods do not provide adequate levels of iodine because the amount varies according to the level in the soil in which the food was grown, as well as the irrigation and fertilizers used. Marine fish and shrimp tend to have high levels because they concentrate iodine from seawater, but many people in landlocked regions lack access to seafood. Thus, the primary source of dietary iodine in many countries is iodized salt. Fortification of salt with iodine became mandatory in Canada in 1949, and international efforts to iodize salt in the world’s poorest nations continue today.
Dietary iodine deficiency can result in the impaired ability to synthesize T3 and T4, leading to a variety of severe disorders. When T3 and T4 cannot be produced, TSH is secreted in increasing amounts. As a result of this hyperstimulation, thyroglobulin and colloid accumulate in the thyroid gland and increase the overall size of the thyroid gland, a condition called a goiter (see Figure 9.6c[3]). A goiter is only a visible indication of the deficiency. Other disorders related to iodine deficiency include impaired growth and development, decreased fertility, and prenatal and infant death. Moreover, iodine deficiency is the primary cause of preventable mental retardation worldwide. Neonatal hypothyroidism (cretinism) is characterized by cognitive deficits, short stature, and sometimes deafness and muteness in children and adults born to mothers who were iodine-deficient during pregnancy.

In areas of the world with access to iodized salt, dietary deficiency is rare. Instead, inflammation of the thyroid gland is a common cause of hypothyroidism, or low blood levels of thyroid hormones. Hypothyroidism is a disorder characterized by a low metabolic rate, weight gain, cold extremities, constipation, reduced libido, menstrual irregularities, and reduced mental activity, and requires long-term thyroid hormone replacement therapy. In contrast, hyperthyroidism—an abnormally elevated blood level of thyroid hormones—is often caused by a pituitary or thyroid tumor. In Graves’ disease, the hyperthyroid state results from an autoimmune reaction in which antibodies overstimulate the follicle cells of the thyroid gland. Hyperthyroidism can lead to an increased metabolic rate, excessive body heat and sweating, diarrhea, weight loss, tremors, and increased heart rate. The person’s eyes may bulge (called exophthalmos) as antibodies produce inflammation in the soft tissues of the orbits. The person may also develop a goiter. Hyperthyroidism is often treated by thyroid surgery or with radioactive iodine (RAI) therapy. Clients are asked to follow radiation precautions after RAI treatment to limit radiation exposure to others, especially pregnant women and young children, such as sleeping in a separate bed and flushing the toilet 2-3 times after use. The RAI treatment may take up to several months to have its effect. The end result of thyroid surgery or RAI treatment is often hypothyroidism, which is treated by thyroid hormone replacement therapy.[4]
Calcitonin
The thyroid gland also secretes another hormone called calcitonin. Calcitonin is released in response to elevated blood calcium levels. It decreases blood calcium concentrations by:
- Inhibiting the activity of osteoclasts (bone cells that breakdown bone matrix and release calcium into the circulation)
- Decreasing calcium absorption in the intestines
- Increasing calcium loss in the urine
Pharmaceutical preparations of calcitonin are prescribed to reduce osteoclast activity in people with osteoporosis. Osteoporosis is a disease that can be caused by glucocorticoids.
Calcium is critical for many other biological processes. It is a second messenger in many signaling pathways and is essential for muscle contraction, nerve impulse transmission, and blood clotting. Given these roles, it is not surprising that blood calcium levels are tightly regulated by the endocrine system. The parathyroid glands are primarily involved in calcium regulation.
Calcium Regulation: Parathyroid Glands
The parathyroid glands are four tiny, round structures usually embedded in the posterior surface of the thyroid gland (see Figure 9.6d).[5] The primary function of the parathyroid glands is to regulate blood calcium levels by producing and secreting parathyroid hormone (PTH) in response to low blood calcium levels.
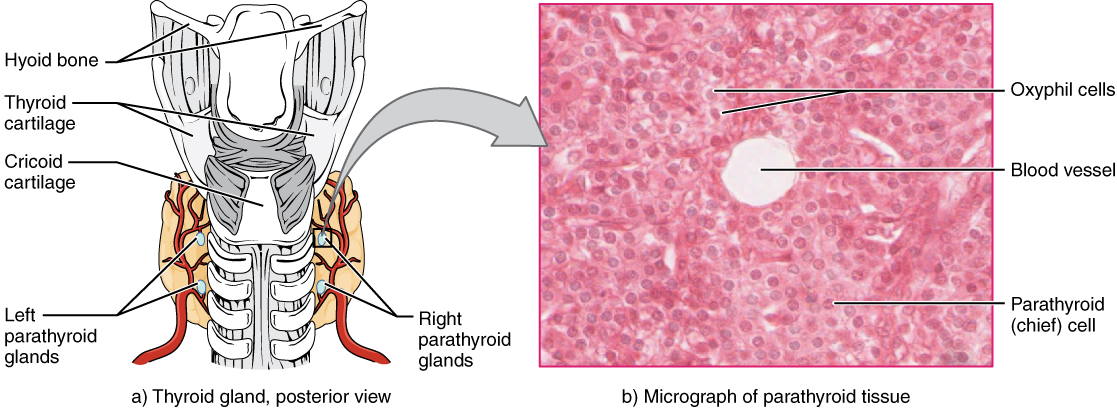
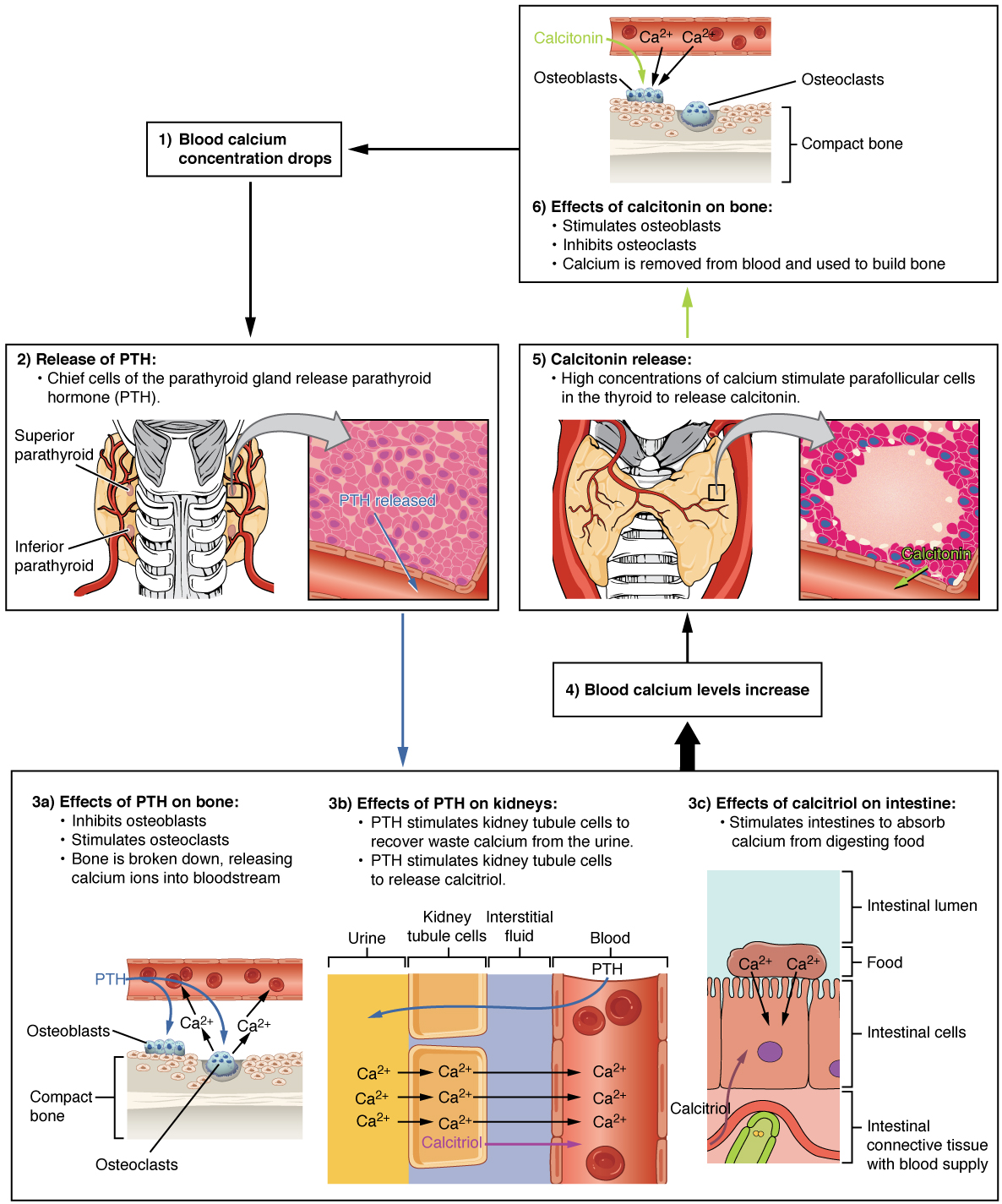
PTH secretion causes the release of calcium from the bones by stimulating osteoclasts that degrade bone and then release calcium into the bloodstream. PTH also inhibits osteoblasts, the cells involved in bone deposition, thereby keeping calcium in the blood. PTH also causes increased reabsorption of calcium (and magnesium) in the kidney and initiates the production of the steroid hormone calcitriol, which is the active form of vitamin D3. Calcitriol then stimulates increased absorption of dietary calcium by the intestines. A negative feedback loop regulates the levels of PTH, with rising blood calcium levels inhibiting further release of PTH. (See Figure 9.6e for an illustration of the role of parathyroid hormone in maintaining blood calcium homeostasis.)[6]
Disorders of the Parathyroid Glands
Abnormally high activity of the parathyroid gland can cause hyperparathyroidism, a disorder caused by an overproduction of PTH that results in excessive degradation of bone and elevated blood levels of calcium, also called hypercalcemia. Hyperparathyroidism can thus significantly decrease bone density, which can lead to spontaneous fractures or deformities. As blood calcium levels rise, cell membrane permeability to sodium is also decreased, and thus the responsiveness of the nervous system is reduced. At the same time, calcium deposits may collect in the body’s tissues and organs, impairing their functioning.
In contrast, abnormally low blood calcium levels may be caused by parathyroid hormone deficiency, called hypoparathyroidism, which may develop following injury or surgery involving the thyroid gland. Low blood calcium increases membrane permeability to sodium, thus increasing the responsiveness of the nervous system, resulting in muscle twitching, cramping, spasms, or convulsions. Severe deficits can paralyze muscles, including those involved in breathing, and can be fatal.
Nursing Considerations
Assessment
When administering thyroid replacement medications, the nurse should plan to monitor TSH levels before and during therapy for effectiveness. Drug interactions may occur with several other medications, so review drug labeling information carefully before administering.
Implementation
Levothyroxine should be administered consistently every morning 30-60 minutes before a meal, in order to increase absorption.
Evaluation
Elevated levels of thyroid hormone can cause cardiac dysrhythmias; immediately report any symptoms of tachycardia, chest pain, or palpitations to the provider.
Thyroid and Osteoporosis Medication Classes
Thyroid Replacement Medication
Indications
Levothyroxine is a thyroid replacement drug used to treat hypothyroidism. See Figure 9.6f for an image of levothyroxine.[7]

Mechanism of Action
Oral levothyroxine sodium is a synthetic T4 hormone that exerts the same physiologic effect as endogenous T4, thereby maintaining normal T4 levels when a deficiency is present.
Specific Administration Considerations
Levothyroxine tablets should be taken with a full glass of water as the tablet may rapidly disintegrate. It should be administered as a single daily dose, on an empty stomach, one-half to one hour before breakfast, and at least 4 hours before or after drugs known to interfere with levothyroxine absorption.
Levothyroxine is contraindicated for clients with hyperthyroidism and adrenal insufficiency until the condition is corrected. Many clients who undergo treatment for hyperthyroidism may develop hypothyroidism. Overtreatment with levothyroxine may cause symptoms of hyperthyroidism with increased heart rate, cardiac wall thickness, and cardiac contractility that may precipitate angina or arrhythmias, particularly in clients with cardiovascular disease and in elderly clients. Levothyroxine therapy in this population should be initiated at lower doses. If cardiac symptoms develop or worsen, the nurse should withhold the medication, contact the health care provider, and anticipate a lower dose prescribed or the medication to be withheld for one week then restarted at a lower dose.
Addition of levothyroxine therapy in clients with diabetes mellitus may worsen glycemic control and result in the need for higher dosages of antidiabetic medication. Carefully monitor glycemic control, especially when thyroid therapy is started, changed, or discontinued.
Levothyroxine increases the response to oral anticoagulant therapy. Therefore, a decrease in the dose of anticoagulant may be warranted with correction of the hypothyroid state or when the levothyroxine dose is increased. Closely monitor INR results and anticipate dosage adjustments.
Levothyroxine can affect, or be affected by, several other medications, so carefully read drug label information when therapy is initiated.
Pregnancy: There are risks to the mother and fetus associated with untreated hypothyroidism in pregnancy. Because TSH levels may increase during pregnancy, TSH should be monitored and levothyroxine dosage may require adjustment during pregnancy.[8]
Client Teaching & Education
Clients should take thyroid replacement medications at the same time each day. Clients should be aware that thyroid replacement medications do not cure hypothyroidism and therapy is lifelong. Clients should notify their healthcare provider if they experience signs of headache, diarrhea, sweating, or heat intolerance. Medications should be spaced four hours apart from medications like antacid, iron, or calcium supplements. Clients will be followed closely by their healthcare provider regarding their response to medication therapy and serum thyroid levels will be taken.[9]
Antithyroid Medication
Indications
Propylthiouracil (PTU) is an antithyroid medication used to treat hyperthyroidism or to ameliorate symptoms of hyperthyroidism in preparation for thyroidectomy or radioactive iodine therapy.
Mechanism of Action
Propylthiouracil inhibits the synthesis of thyroid hormones.
Specific Administration Considerations
Propylthiouracil is administered orally. The total daily dosage is usually given in 3 equal doses at approximately 8-hour intervals. Propylthiouracil can cause hypothyroidism necessitating routine monitoring of TSH and free T4 levels, with adjustments in dosing to maintain a euthyroid state.
Liver injury resulting in liver failure, liver transplantation, or death has been reported. Clients should be instructed to report any symptoms of hepatic dysfunction (anorexia, pruritus, and right upper quadrant pain), particularly in the first six months of therapy.
Agranulocytosis is a potentially life-threatening side effect of propylthiouracil therapy. Agranulocytosis typically occurs within the first 3 months of therapy. Clients should be instructed to immediately report any symptoms suggestive of agranulocytosis, such as fever or sore throat.
Cases of vasculitis resulting in severe complications and death have been reported in clients receiving propylthiouracil therapy. If vasculitis is suspected, discontinue therapy and initiate appropriate intervention.
Pregnancy: Propylthiouracil crosses the placenta and can cause fetal liver failure, goiter, and cretinism if administered to a pregnant woman.
Client Teaching & Education
Clients should take the medication as directed at regular dosing intervals. They should monitor their weight 2-3 times per week. Additionally, clients should be advised that medications may cause drowsiness, and they should report any signs of sore throat, fever, headache, jaundice, bleeding, or bruising.
Osteoporosis Medication: Calcitonin
Indications
Calcitonin is used to treat osteoporosis.
Mechanism of Action
Calcitonin is a calcitonin receptor agonist. Calcitonin is released by the thyroid gland. It acts primarily on bone and also has effects on the kidneys and the gastrointestinal tract.
Specific Administration Considerations
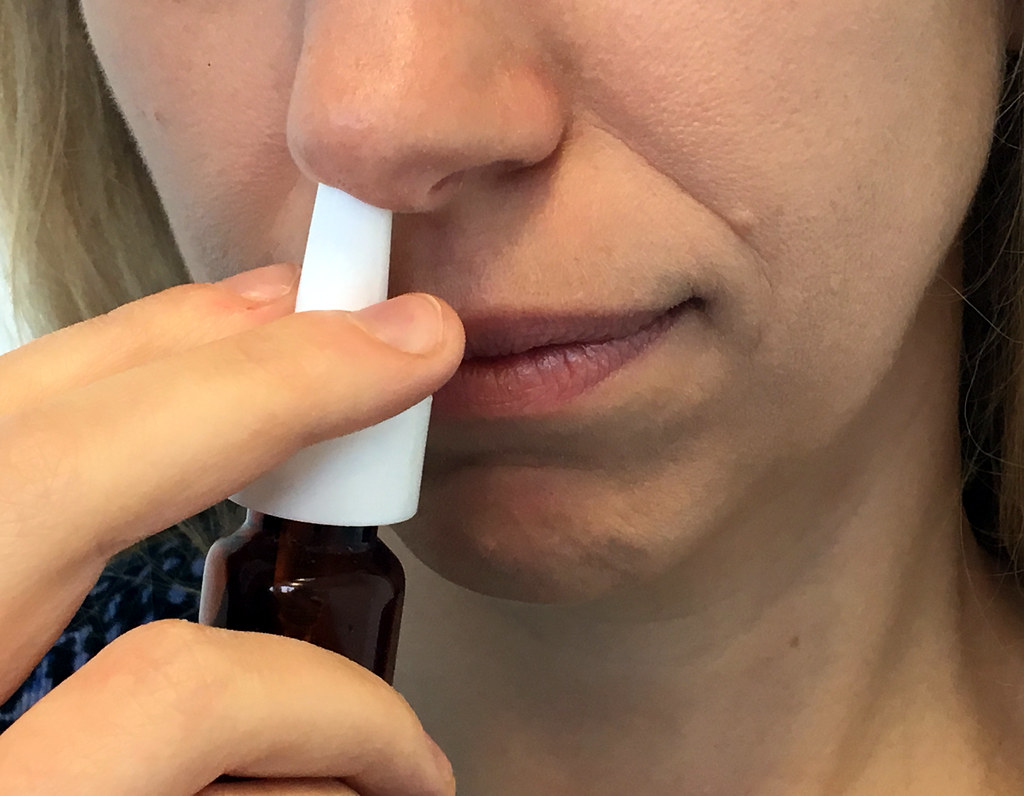
Calcitonin is administered via nasal spray with one spray in one side of the nose daily. See Figure 9.6g for an image of calcitonin nasal spray.[10] The nasal spray pump should be primed before the first administration. Unopened calcitonin can be stored in the refrigerator until opened, but should not be refrigerated between doses. Opened bottles stored at room temperature should be discarded after 30 days of initial dose.
Adverse effects include serious hypersensitivity reactions (bronchospasm, swelling of the tongue or throat, anaphylaxis and anaphylactic shock), hypocalcemia, nasal mucosa adverse events, and malignancy.
Pregnancy: Calcitonin should not be used during pregnancy.
Client Teaching & Education
Clients should be advised to take medications as directed. They should report any signs of hypercalcemia or an allergic response. Clients should receive instruction on the process of self-injection. They should also be advised that they may experience flushing and warmth following injection. Post-menopausal women should adhere to a diet high in calcium and vitamin D, and should be educated regarding the importance of exercise for reversing bone loss.[11]
Osteoporosis Medication: Alendronate
Indications
Alendronate is used for the prevention and treatment of osteoporosis in postmenopausal women, to increase bone mass in men with osteoporosis, and for glucocorticoid-induced osteoporosis.
Mechanism of Action
Alendronate is a bisphosphonate that inhibits osteoclast-mediated bone resorption. By preventing the breakdown of bone and enhancing the formation of new bone, alendronate assists in reversing bone loss and decreases the risk of fractures.
Specific Administration Considerations
Check dosages carefully because some formulations are administered daily, whereas others are administered one weekly. Alendronate should be taken upon arising for the day, but should be administered at least one-half hour before the first food, beverage, or medication of the day with plain water only. Other beverages (including mineral water), food, and some medications are likely to reduce the absorption of alendronate. Clients should not lie down for at least 30 minutes and until after their first food of the day. Clients may also require calcium and vitamin D supplementation, especially if concurrently taking glucocorticoids.
Alendronate is contraindicated in the following conditions: pregnancy, hypocalcemia, the inability to sit or stand for 30 minutes after swallowing, esophageal abnormalities that delay emptying, and clients at risk for aspiration. Alendronate is not recommended for clients with kidney disease with creatinine clearance less than 35 mL/min.
Discontinue alendronate if severe musculoskeletal pain occurs. A bone mineral density measurement should be made at the initiation of therapy and repeated after 6 to 12 months of combined alendronate and glucocorticoid treatment.
Client Teaching & Education
Clients should take medication as directed at the same time each day, first thing in the morning. Clients should remain upright after they take medication for 30 minutes to minimize stomach and esophageal irritation. Clients should eat a balanced diet and may seek advice from the healthcare provider regarding supplementation with calcium and vitamin D. Clients should participate in regular exercise to help increase bone strength.[12]
Medication Card Comparing Thyroid (levothyroxine, propylthiouracil) and Osteoporosis Medications (calcitonin, alendronate)
Now let’s take a closer look at the medication card comparing thyroid and osteoporosis medications in Table 9.6.[13] Medication cards are intended to assist students to learn key points about each medication. Because information about medication is constantly changing, nurses should always consult evidence-based resources to review current recommendations before administering specific medication. Basic information related to each class of medication is outlined below.
Medication Card 9.6: Comparing Thyroid (levothyroxine, propylthiouracil) and Osteoporosis Medications (calcitonin, alendronate)
| Class | Prototypes | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Thyroid replacement | levothyroxine | Take levothyroxine sodium tablets with a full glass of water as the tablet may rapidly disintegrate
Administer levothyroxine as a single daily dose, on an empty stomach, one-half to one hour before breakfast Administer levothyroxine at least 4 hours before or after drugs known to interfere with levothyroxine sodium tablets absorption Anticipate lower dosages in elderly clients with pre-existing cardiac disease May interact with several medications so read drug label thoroughly on initial administration for potential effects |
Increases T4 levels in hypothyroidism | Hypersensitivity reactions
Cardiac dysrhythmias |
| Antithyroid | propylthiouracil (PTU) | Usually administered every 8 hours
May cause hypothyroidism so TSH and T4 levels should be monitored If a client becomes pregnant, immediately notify health care provider because it can cause fetal harm |
Inhibit production of T4 to treat hyperthyroidism | Hypothyroidism
Liver failure Agranulocytosis Vasculitis Fetal harm |
| Calcium regulator | calcitonin | Administer nasal spray with one spray in one side of the nose daily
Contraindicated during pregnancy Discard unrefrigerated bottle after 30 days of opening May store unopened bottles in refrigerator until expiration date |
Treats osteoporosis | Serious hypersensitivity reactions (bronchospasm, swelling of the tongue or throat, anaphylaxis, and anaphylactic shock)
Hypocalcemia Nasal mucosa adverse effects Malignancy |
| Bisphosphonates | alendronate | Administered upon arising and at least one-half hour before the first food, beverage, or medication of the day with plain water only
The client should sit or stand for 30 minutes after administration Contraindicated in pregnancy, hypocalcemia, and kidney disease Concurrent calcium and vitamin D supplements may be required |
Enhances bone mineral density in osteoporosis | Upper GI tract adverse events
Severe musculoskeletal pain Risk of osteonecrosis of the jaw |
A client has been diagnosed with hypothyroidism and receives a prescription for levothyroxine.
What client education should the nurse provide regarding taking this medication?
Note: Answers to the activities can be found in the “Answer Key” sections at the end of the book.
Image Descriptions
Figure 9.6b Negative Feedback Loop: A flowchart demonstrating the negative feedback loop regulating thyroid hormone levels. It details the following steps:
- Metabolic rate and/or T3 and T4 concentration in blood:
- High? Hypothalamus stops TRH release. Anterior pituitary stops TSH release.
- Low? Hypothalamus releases TRH. This triggers TSH release by the pituitary.
- Effects of TSH release: Triggers release of T3 and T4 by thyroid follicle cells.
- Effects of T3 and T4 release:
- Increased basal metabolic rate of body cells.
- Rise in body temperature (calorigenic effect).
- Negative feedback:
- Elevated T3 and T4 levels inhibit release of TRH and TSH.
- If T3 and T4 are high:
- Hypothalamus stops TRH release.
- Anterior pituitary stops TSH release.
Figure 9.6e Parathyroid Hormone in Maintaining Blood Calcium Homeostasis: A flowchart demonstrating how parathyroid hormone (PTH) helps to maintain blood calcium homeostasis. It details the following steps:
- Blood calcium concentration drops.
- Release of PTH: chief cells of the parathyroid gland release parathyroid hormone (PTH).
- This has the following effects:
- Effects of PTH on bone:
- Inhibits osteoblasts.
- Stimulates osteoclasts.
- Bone is broken down, releasing calcium ions into bloodstream.
- Effects of PTH on kidneys:
- PTH stimulates kidney tubule cells to recover waste calcium from the urine.
- PTH stimulates kidney tubule cells to release calcitriol.
- Effects of calcitriol on intestine:
- Stimulates intestines to absorb calcium from digesting food.
- Effects of PTH on bone:
- Blood calcium levels increase.
- Calcitonin release: high concentrations of calcium stimulate parafollicular cells in the thyroid to release calcitonin.
- Effects of calcitonin on bone:
- Stimulates osteoblasts.
- Inhibits osteoclasts.
- Calcium is removed from blood and used to build bone.
- "1811 The Thyroid Gland.jpg" by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/17-4-the-thyroid-gland ↵
- "1813 A Classic Negative Feedback Loop.jpg" by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/17-4-the-thyroid-gland ↵
- "Goitre.jpg" by Almazi is licensed under CC0 ↵
- American Thyroid Association. (2019). Radioactive iodine. https://www.thyroid.org/radioactive-iodine/ ↵
- "1814 The Parathyroid Glands.jpg" by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/17-5-the-parathyroid-glands ↵
- "1817 The Role of Parathyroid Hormone in Maintaining Blood Calcium Homeostasis.jpg" by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/17-5-the-parathyroid-glands ↵
- "Levothyroxine 25mcg Tablets.jpg" by User:Ash is licensed under CC0 ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- "Nasal Spray" by NIAID is licensed under CC BY 2.0 ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- uCentral from Unbound Medicine. https://www.unboundmedicine.com/ucentral ↵
- This work is a derivative of Daily Med by U.S. National Library of Medicine in the public domain. ↵
A visible enlargement of the thyroid gland when there is hyperstimulation of TSH due to deficient levels of T3 and T4 hormones in the bloodstream or an autoimmune reaction in which antibodies overstimulate the follicle cells of the thyroid gland, causing hyperthyroidism.
Abnormally low blood levels of thyroid hormones T3 and T4 in the bloodstream.
Abnormally elevated blood level of thyroid hormones T3 and T4, often caused by a pituitary tumor, thyroid tumor, or autoimmune reaction in which antibodies overstimulate the follicle cells of the thyroid gland
The hormone released by parathyroid glands; involved in the regulation of blood calcium levels.
A disorder caused by an overproduction of PTH that results in excessive calcium resorption from bone, causing significantly decreased bone density and spontaneous fractures, decreased responsiveness of the nervous system, and calcium deposits in the body’s tissues and organs, impairing their functioning.
Abnormally low blood calcium levels caused by parathyroid hormone deficiency, which may develop following thyroid surgery. Low blood calcium can cause muscle twitching, cramping, spasms, or convulsions; severe deficits can paralyze muscles, including those involved in breathing, and can be fatal.

