Chapter 1: Introduction to the Role of the Hospital Unit Coordinator
Overview of the HUC Role
In our first section, we will be reviewing the role of the hospital unit coordinator (HUC) in hospitals, as well as the role of other professionals that they will be interacting with in the hospital environment. Hospital unit coordinator or HUC is the term we will use for the health office administrative role within hospitals. You will see other terms used for the same role, including health unit coordinator, communication clerk, clerical associate, unit clerk, or clinical secretary.
“A new helper introduced to the nursing unit to take care of the many details of a secretarial nature that formerly made demands on the limited time of the nurse.”
— Abraham Oseroff, 1940[1]
The Evolution of the HUC Role
Prior to World War II, there were few support personnel employed in hospitals. As the nurse’s clinical role expanded, it became more difficult for them to manage the desk duties on the clinical unit. At that time, a support role called “floor clerk” was introduced to many hospital units to relieve some of the pressure on the nursing staff. Following the war, as healthcare facilities expanded and nursing shortages were experienced, more responsibilities were placed upon the “ward clerk.” Many of these duties were assumed from head nurses, including ordering supplies, preparing reports, doing staffing, and transcribing simple physician orders (National Association of Health Unit Coordinators, n.d.).
By the 1960s, formal education for the ward clerk role started to appear in vocational schools and community colleges. By the 1980s, formal diplomas and certificates were offered at many post-secondary institutions, and professional associations were developed. In the United States, a national professional organization named the National Association of Health Unit Coordinators (NAHUC) developed a professional Code of Ethics and Standards for Practice, National Certification Exam, professional certification and code of ethics specifically for the HUC, along with a national HUC day of recognition (National Association of Health Unit Coordinators, n.d.).
The financial pressure that hospitals experienced throughout the 1980s and 1990s increased their interest in utilizing their higher-paid nursing staff to their full advantage. This resulted in the reduction of nursing desk tasks and more administrative clinical tasks being assigned to the unit coordinator, such as transcription of medications, and as new electronic health records (EHRs) were developed, computerized order entry. With this increase in responsibility, the unit coordinator role also had increased expectations for formal education. Hospitals are now moving towards an increased level of computerization, which will change some of the HUC’s clinical role; however, the need for skilled HUCs still remains to effectively communicate and manage critical unit functions.
Take Note! HUC Week
August 23 to 29 is the annual “Health Unit Coordinator Week” in the United States.
Learn more on the NAHUC website.
HUC Duties
HUCs typically work in forward-facing roles in a variety of hospital settings and may complete a wide variety of tasks, such as
- managing the pre-registration, registration, transfer, and discharge processes for patients,
- using scheduling software to schedule inpatient and outpatient tests and surgical procedures,
- transcribing physician’s orders for medication, laboratory, diagnostic imaging, and treatments into computer systems and medication records,
- managing the staffing, scheduling and payroll functions for their unit,
- arranging for urgent and non-urgent patient transportation services,
- completing various administrative tasks such as sending emails, ordering supplies, scheduling meetings, taking minutes, and keeping statistics,
- completing various communication tasks such as answering telephones and call bells, utilizing paging systems, greeting patients, and updating bed boards and patient tracking systems,
- completing various health information management tasks such as scanning, filing, purging charts, and performing post-discharge processing of patient records, and
- applying security measures to ensure confidentiality and safety of patient information.
Working Conditions
The HUC usually works day and evening shifts seven days a week in hospitals and other health care facilities, such as long-term care. However, in some hospital critical care units, such as the emergency department (ED) or intensive care unit (ICU), they may be required to work rotating shifts that also include nights. The HUC’s schedule reflects the general staff utilization patterns in the hospital where they are employed and may change depending upon their status as full-time or part-time employees or changing hospital requirements. In general, the HUC may expect to work 4-, 8-, 10- or 12-hour shifts, or some mixture of these.
The HUC may experience a variety of workplace stressors. They work in very busy environments and continually interact with other people both in person and on the telephone. Accordingly, they must have the ability to work effectively despite frequent interruptions. They may experience a large variety of background noise, odours, and infectious materials in their typical day. The HUC may also face ongoing exposure to the emotional stress that illness or injury causes patients and their families and must effectively communicate with and support patients and families experiencing medical crises or loss (ALIS, 2021).
The HUC can expect that they will be moderately active in this role. While the majority of their work takes place at a desk (often called a communication centre/nursing station), they may also be standing and walking for a large portion of their shift as they retrieve patients from wait areas, escort patients and/or families to rooms, retrieve supplies, medications, and dietary trays, and deliver specimens to the laboratory.
Required Knowledge, Skills, and Abilities
While each organization will have unique requirements, the basic qualifications for an HUC include the completion of a formal post-secondary medical administrative program that includes
- medical terminology and abbreviations,
- health information management, including filing, scanning, privacy laws, filing, and documentation methods,
- knowledge of common lab and diagnostic tests, including patient preparation,
- basic pharmacology, including the ability to read and transcribe physician medication orders,
- communication, including interpersonal, written, therapeutic, and conflict management, and
- computer skills, including database management, EHR, file management, and MS Office.
In addition, HUCs are usually expected to demonstrate:
- keyboarding skills (minimum of 50-60 wpm with 97% accuracy, which is often tested),
- completion of immunizations required under the Public Hospitals Act,
- completion of a recognized CPR course and a clear vulnerable sector (VSS) police check,
- strong customer service, organization, attention to detail, and prioritization skills, and
- strong attendance records.
References
ALIS. (2021, March 5). Occupations in Alberta: Unit clerk. Government of Alberta.
Gillingham, E. A., & Wadsworth Seibel, M.M. (2014). LaFleur Brooks’ health unit coordinating. (7th ed.). Elsevier.
National Association of Health Unit Coordinators. (n.d.). NAHUC history.
Attributions
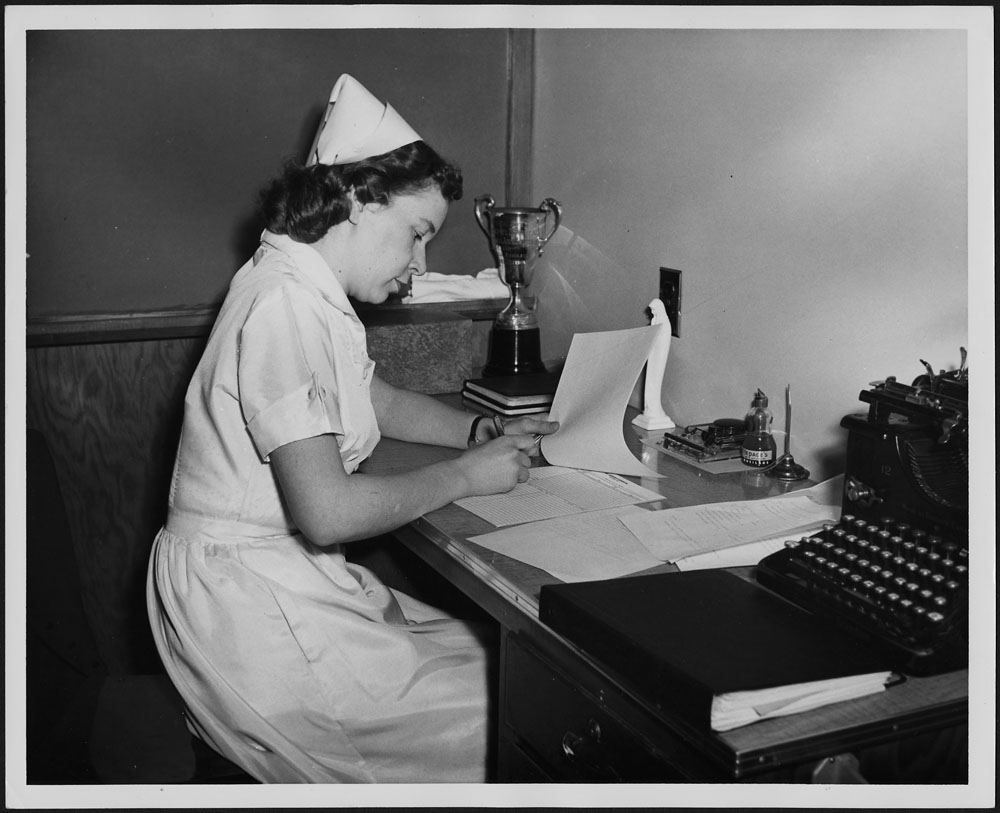
“A nurse filling out a patient report in the children’s ward at St. Joseph’s Hospital, Victoria, B.C.” by unknown. Canada Department of Manpower and Immigration. Library and Archives Canada, e010982306 on flickr; licensed Creative Commons – Attribution 2.0 Generic.
- As cited in National Association of Health Unit Coordinators, n.d., para. 3. ↵
a term for the health office administrative role within hospitals; also called health unit coordinator, communication clerk, clerical associate, unit clerk, or clinical secretary

