Learning Objectives
Describe the process of tissue response to injury.
By the end of this section, you will be able to:
- Identify the cardinal signs of inflammation
- List the body’s response to tissue injury
- Explain the process of tissue repair
- Discuss the progressive impact of aging on tissue
- Describe cancerous mutations’ effect on tissue
Tissues of all types are vulnerable to injury and, inevitably, aging. In the former case, understanding how tissues respond to damage can guide strategies to aid repair. In the latter case, understanding the impact of aging can help in the search for ways to diminish its effects.
Tissue Injury and Repair
Inflammation is the standard, initial response of the body to injury. Whether biological, chemical, physical, or radiation burns, all injuries lead to the same sequence of physiological events. Inflammation limits the extent of injury, partially or fully eliminates the cause of injury, and initiates repair and regeneration of damaged tissue. Necrosis, or accidental cell death, causes inflammation. Apoptosis is programmed cell death, a normal step-by-step process that destroys cells no longer needed by the body. By mechanisms still under investigation, apoptosis does not initiate the inflammatory response. Acute inflammation resolves over time by the healing of tissue. If inflammation persists, it becomes chronic and leads to diseased conditions. Arthritis and tuberculosis are examples of chronic inflammation. The suffix “-itis” denotes inflammation of a specific organ or type. For example, peritonitis is the inflammation of the peritoneum, and meningitis refers to the inflammation of the meninges, the tough membranes that surround the central nervous system.
The four cardinal signs of inflammation—redness (at least for people with light colored skin), swelling, pain, and local heat—were first recorded in antiquity. Cornelius Celsus is credited with documenting these signs during the days of the Roman Empire, as early as the first century AD. A fifth sign, loss of function, may also accompany inflammation.
Upon tissue injury, damaged cells release inflammatory chemical signals that evoke local vasodilation, the widening of the blood vessels. Increased blood flow can change the color of the integument and result in a localized temperature increase. In response to injury, mast cells present in tissue degranulate, releasing the potent vasodilator histamine. Increased blood flow and inflammatory mediators recruit white blood cells to the site of inflammation. The endothelium lining the local blood vessel becomes “leaky” under the influence of histamine and other inflammatory mediators allowing neutrophils, macrophages, and fluid to move from the blood into the interstitial tissue spaces. The excess liquid in tissue causes swelling, properly called edema. The swollen tissues stimulate mechanical receptors, which can cause the perception of pain. Prostaglandins released from injured cells also activate pain pathways. Non-steroidal anti-inflammatory drugs (NSAIDs) reduce perceived pain because they inhibit the synthesis of prostaglandins. High levels of NSAIDs reduce inflammation. Antihistamines decrease allergies by blocking histamine receptors and as a result, the histamine response.
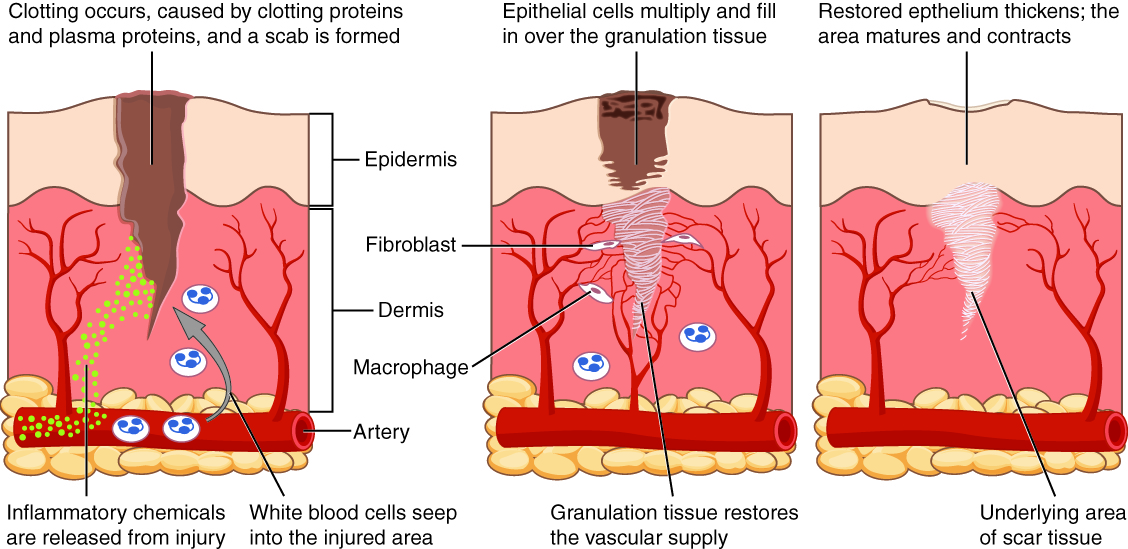
After containment of an injury, the tissue repair phase starts with removal of toxins and waste products. Clotting (coagulation) reduces blood loss from damaged blood vessels and forms a network of fibrin proteins that trap blood cells and bind the edges of the wound together. A scab forms when the clot dries, reducing the risk of infection. Sometimes a mixture of dead leukocytes and fluid called pus accumulates in the wound. As healing progresses, fibroblasts from the surrounding connective tissues replace the collagen and extracellular material lost by the injury. Angiogenesis, the growth of new blood vessels, results in vascularization of the new tissue known as granulation tissue. The clot retracts pulling the edges of the wound together, and it slowly dissolves as the tissue is repaired. When a large amount of granulation tissue forms and capillaries disappear, a pale scar is often visible in the healed area. A primary union describes the healing of a wound where the edges are close together. When there is a gaping wound, it takes longer to refill the area with cells and collagen. The process called secondary union occurs as the edges of the wound are pulled together by what is called wound contraction. When a wound is more than one quarter of an inch deep, sutures (stitches) are recommended to promote a primary union and avoid the formation of a disfiguring scar. Regeneration is the addition of new cells of the same type as the ones that were injured (Figure 4.6.1 – Tissue Healing).
External Website

Watch this video to see a hand heal. Over what period of time do you think these images were taken?
Tissue and Aging
According to poet Ralph Waldo Emerson, “The surest poison is time.” In fact, biology confirms that many functions of the body decline with age. All the cells, tissues, and organs are affected by senescence, with noticeable variability between individuals owing to different genetic makeup and lifestyles. The outward signs of aging are easily recognizable. The skin and other tissues become thinner and drier, reducing their elasticity, contributing to wrinkles and high blood pressure. Hair turns gray because follicles produce less melanin, the brown pigment of hair and the iris of the eye. The face looks flabby because elastic and collagen fibers decrease in connective tissue and muscle tone is lost. Glasses and hearing aids may become parts of life as the senses slowly deteriorate, all due to reduced elasticity. Overall height decreases as the bones lose calcium and other minerals. With age, fluid decreases in the fibrous cartilage disks intercalated between the vertebrae in the spine. Joints lose cartilage and stiffen. Many tissues, including those in muscles, lose mass through a process called atrophy. Lumps and rigidity become more widespread. As a consequence, the passageways, blood vessels, and airways become more rigid. The brain and spinal cord lose mass. Nerves do not transmit impulses with the same speed and frequency as in the past. Some loss of thought, clarity, and memory can accompany aging. More severe problems are not necessarily associated with the aging process and may be symptoms of an underlying illness.
As exterior signs of aging increase, so do the interior signs, which are not as noticeable. The incidence of heart diseases, respiratory syndromes, and type 2 diabetes increases with age, though these are not necessarily age-dependent effects. Wound healing is slower in the elderly, accompanied by a higher frequency of infection as the capacity of the immune system to fend off pathogens declines.
Aging is also apparent at the cellular level because all cells experience changes with aging. Telomeres, regions of the chromosomes necessary for cell division, shorten each time cells divide. As they do, cells are less able to divide and regenerate. Because of alterations in cell membranes, transport of oxygen and nutrients into the cell and removal of carbon dioxide and waste products from the cell are not as efficient in the elderly. Cells may begin to function abnormally, which may lead to diseases associated with aging, including arthritis, memory issues, and some cancers.
The progressive impact of aging on the body varies considerably among individuals. However, studies indicate that exercise and healthy lifestyle choices can slow down the deterioration of the body that comes with old age.
Homeostatic Imbalances: Tissues and Cancer
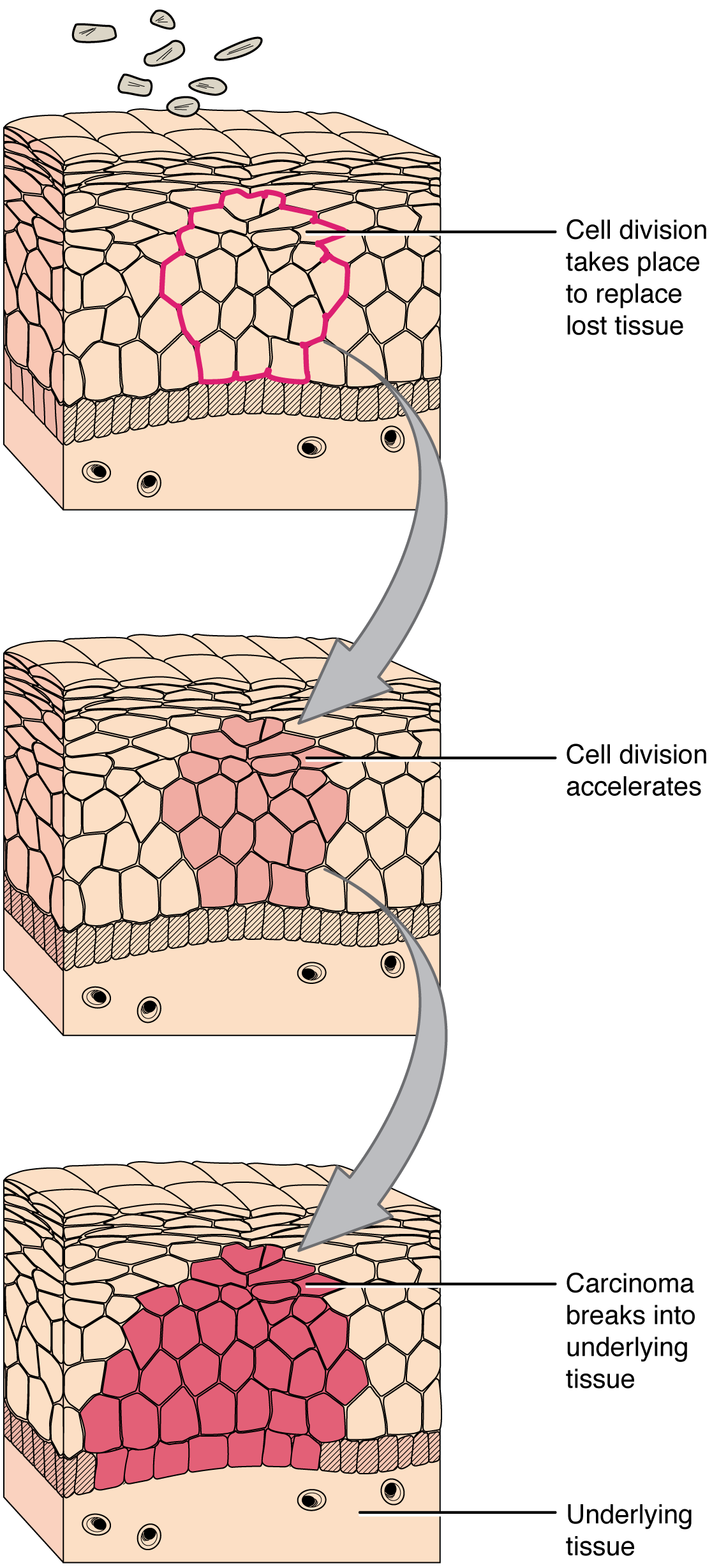
Cancer is a generic term for many diseases in which cells escape regulatory signals. Uncontrolled growth, invasion into adjacent tissues, and colonization of other organs, if not treated early enough, are its hallmarks. Health suffers when tumors “rob” blood supply from the “normal” organs.
A mutation is defined as a permanent change in the DNA of a cell. Epigenetic modifications, changes that do not affect the code of the DNA but alter how the DNA is decoded, are also known to generate abnormal cells. Alterations in the genetic material may be caused by environmental agents, infectious agents, or errors in the replication of DNA that accumulate with age. Many mutations do not cause any noticeable change in the functions of a cell, however, if the modification affects key proteins that have an impact on the cell’s ability to proliferate in an orderly fashion, the cell starts to divide abnormally. As changes in cells accumulate, they lose their ability to form regular tissues. A tumor, a mass of cells displaying abnormal architecture, forms in the tissue. Many tumors are benign, meaning they do not metastasize nor cause disease. A tumor becomes malignant, or cancerous, when it breaches the confines of its tissue, promotes angiogenesis, attracts the growth of capillaries, and metastasizes to other organs (Figure 4.6.2 Development of Cancer). The specific names of cancers reflect the tissue of origin. Cancers derived from epithelial cells are referred to as carcinomas. Cancer in myeloid tissue or blood cells form myelomas. Leukemias are cancers of white blood cells, whereas sarcomas derive from connective tissue. Cells in tumors differ both in structure and function. Some cells, called cancer stem cells, appear to be a subtype of cell responsible for uncontrolled growth. Recent research shows that contrary to what was previously assumed, tumors are not disorganized masses of cells, but have their own structures.
Cancer treatments vary depending on the disease’s type and stage. Traditional approaches, including surgery, radiation, chemotherapy, and hormonal therapy. The aim is to remove or kill rapidly dividing cancer cells, but these strategies have their limitations. Depending on a tumor’s location, for example, cancer surgeons may be unable to remove it. Radiation and chemotherapy are difficult, and it is often impossible to target only the cancer cells. The treatments inevitably destroy healthy tissue as well. To address this, researchers are working on pharmaceuticals that can target specific proteins implicated in cancer-associated molecular pathways.
Chapter Review
Inflammation is the classic response of the body to injury and follows a common sequence of events. The area is red, feels warm to the touch, swells, and is painful. Injured cells, mast cells, and resident macrophages release chemical signals that cause vasodilation and fluid leakage in the surrounding tissue. The repair phase includes blood clotting, followed by regeneration of tissue as fibroblasts deposit collagen. Some tissues regenerate more readily than others. Epithelial and connective tissues replace damaged or dead cells from a supply of adult stem cells. Muscle and nervous tissues undergo either slow regeneration or do not repair at all.
Age affects all the tissues and organs of the body. Damaged cells do not regenerate as rapidly as in younger people. Perception of sensation and effectiveness of response are lost in the nervous system. Muscles atrophy, and bones lose mass and become brittle. Collagen decreases in some connective tissue, and joints stiffen.
Interactive Link Questions
Watch this video to see a hand heal. Over what period of time do you think these images were taken?
Approximately one month.
Watch this video to learn more about tumors. What is a tumor?
A mass of cancer cells that continue to grow and divide.
Review Questions
Critical Thinking Questions
Why is it important to watch for increased redness, swelling and pain after a cut or abrasion has been cleaned and bandaged?
These symptoms would indicate that infection is present.
Aspirin is a non-steroidal anti-inflammatory drug (NSAID) that inhibits the formation of blood clots and is taken regularly by individuals with a heart condition. Steroids such as cortisol are used to control some autoimmune diseases and severe arthritis by down-regulating the inflammatory response. After reading the role of inflammation in the body’s response to infection, can you predict an undesirable consequence of taking anti-inflammatory drugs on a regular basis?
Since NSAIDs or other anti-inflammatory drugs inhibit the formation of blood clots, regular and prolonged use of these drugs may promote internal bleeding, such as bleeding in the stomach. Excessive levels of cortisol would suppress inflammation, which could slow the wound healing process.
As an individual ages, a constellation of symptoms begins the decline to the point where an individual’s functioning is compromised. Identify and discuss two factors that have a role in factors leading to the compromised situation.
The genetic makeup and the lifestyle of each individual are factors which determine the degree of decline in cells, tissues, and organs as an individual ages.
Discuss changes that occur in cells as a person ages.
All cells experience changes with aging. They become larger, and many cannot divide and regenerate. Because of alterations in cell membranes, transport of oxygen and nutrients into the cell and removal of carbon dioxide and waste products are not as efficient in the elderly. Cells lose their ability to function, or they begin to function abnormally, leading to disease and cancer.
References
Emerson, RW. Old age. Atlantic. 1862 [cited 2012 Dec 4]; 9(51):134–140.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.


