Key Takeaways
By the end of this section, you will be able to:
Describe how the kidney modifies filtrate to influence urine production
- Describe the characteristics of a normal urine sample
- Explain the role of the loop of Henle, the vasa recta, and the countercurrent multiplication mechanisms in urine production
- Explain the role of aldosterone and ADH in urine production
- Identify the ureters, urinary bladder, and urethra, as well as their location, structure, histology, and function
- Describe the micturition reflex
- Describe voluntary and involuntary neural control of micturition
Urine is the end product once the filtrate has been fully manipulated by the nephrons. Until the filtrate passes through the renal papilla into the minor calyx, it can be affected by nephron processes. This is how kidneys produce anywhere from .4 L of urine/day to as much as 20L urine/day, all while balancing plasma composition and excreting potential toxins in the urine.
Composition of Urine
The two kidneys filter your entire blood volume many times each day to remove wastes as urine. Characteristics of urine can be variable (Table 25.1) depending on water intake and losses, nutrient intake, and other factors described in this chapter, though cells, proteins and blood are not normally found in the urine. Some of the characteristics such as color and odor are rough descriptors of your state of hydration. For example, if you exercise or work outside, and sweat a great deal, your urine will turn darker and produce a slight odor. Alternatively, a well hydrated person will have light or clear colored urine with little odor (Figure 25.8.1).
| Normal Urine Characteristics (Table 25.1) | |
|---|---|
| Characteristic | Normal values |
| Color | Pale yellow to deep amber |
| Odor | Odorless |
| Volume | 750–2000 mL/24 hour |
| pH | 4.5–8.0 |
| Specific gravity | 1.003–1.032 |
| Osmolarity | 40–1350 mOsmol/kg |
| Urobilinogen | 0.2–1.0 mg/100 mL |
| White blood cells | 0–2 HPF (per high-power field of microscope) |
| Leukocyte esterase | None |
| Protein | None or trace |
| Bilirubin | <0.3 mg/100 mL |
| Ketones | None |
| Nitrites | None |
| Blood | None |
| Glucose | None |
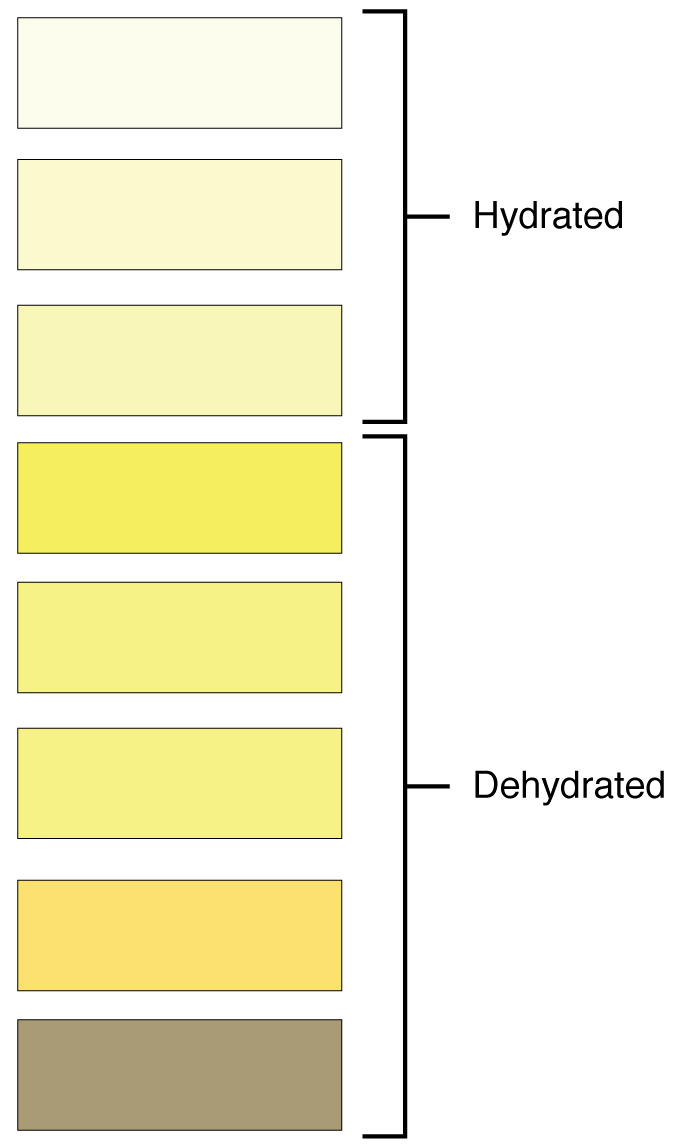
The pH (hydrogen ion concentration) of the urine can vary more than 1000-fold, from a normal low of 4.5 to a maximum of 8.0 depending on actions of specific cells of the kidney. Urine osmolarity is the number of osmoles or milliosmoles per liter of fluid (mOsmol/L). Urine osmolarity ranges from a low of 50–100 mOsmol/L to as high as 1200 mOsmol/L H2O. The color of urine is determined mostly by the breakdown products of red blood cell destruction (Figure 25.8.1). The “heme” of hemoglobin is converted by the liver into water-soluble forms that can be excreted into the bile and indirectly into the urine. This yellow pigment is urochrome.
Urine color may also be affected by certain foods like beets, berries, and fava beans. Dehydration produces darker, concentrated urine that may also possess the slight odor of ammonia. Ammonia (NH3) is a toxic byproduct of protein metabolism. It is formed as amino acids are deaminated by liver hepatocytes. That means that the amine group, NH2, is removed from amino acids as they are broken down. Most of the resulting ammonia is converted into urea by liver hepatocytes. Urea is not only less toxic but is utilized to aid in the recovery of water by the loop of Henle and collecting ducts to control urine volume.
Urine volume varies considerably. The normal range is one to two liters per day. The kidneys must produce a minimum urine volume of about 400 mL/day to rid the body of wastes. Output below this level may be caused by severe dehydration or renal disease. The regulation of urine volume reflects regulation of urine and blood composition as described below.
Blood is filtered, and the filtrate is transformed into urine at a relatively constant rate throughout the day. Urine is stored until a convenient time for excretion. All structures involved in the transport and storage of the urine are large enough to be visible to the naked eye. This transport and storage system not only stores the waste, but it protects the tissues from damage due to the wide range of pH and osmolarity of the urine.
Ureters
As urine is formed, it drains into the calyces of the kidney, which merge to form the funnel-shaped renal pelvis in the hilum of each kidney. The renal pelvis narrows to become the ureter of each kidney. As urine passes through the ureter, it does not passively drain into the bladder but rather is propelled by waves of peristalsis. As the ureters enter the pelvis, they pass laterally, hugging the pelvic walls. As they approach the bladder, they turn medially and join with the bladder wall obliquely. This is important because it creates an one-way valve (a physiological sphincter rather than an anatomical sphincter) that allows urine into the bladder but prevents reflux of urine from the bladder back into the ureter. Children born lacking this oblique course of the ureter through the bladder wall are susceptible to “vesicoureteral reflux,” which dramatically increases their risk of serious UTI. Pregnancy also increases the likelihood of reflux and UTI.
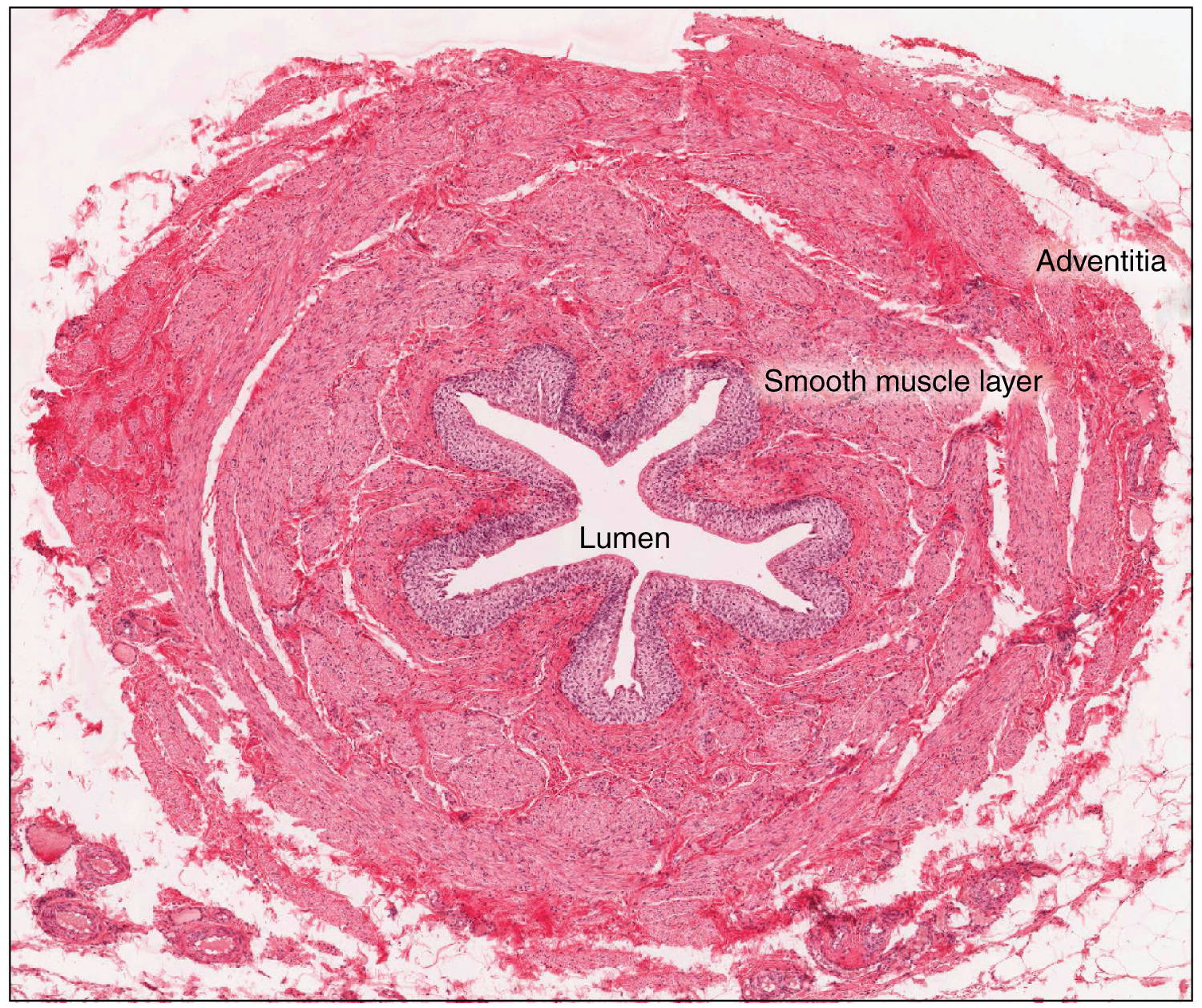
The ureters are approximately 30 cm long. The inner mucosa is lined with transitional epithelium (Figure 25.8.2) and scattered goblet cells that secrete protective mucus. The muscular layer of the ureter consists of longitudinal and circular smooth muscles that create the peristaltic contractions to move the urine into the bladder without the aid of gravity. Finally, a loose adventitial layer composed of collagen and fat anchors the ureters between the parietal peritoneum and the posterior abdominal wall.
Bladder
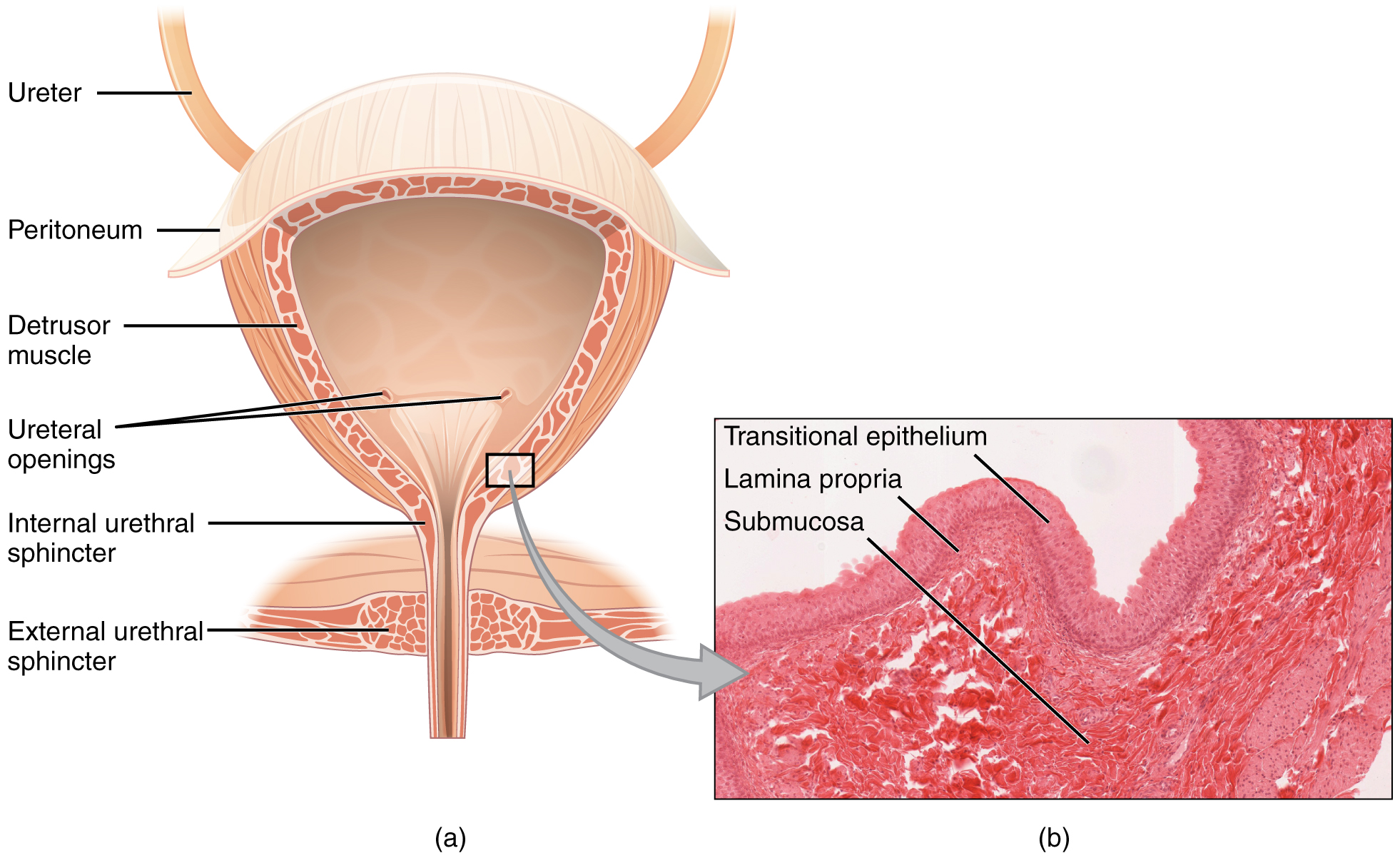
The urinary bladder collects urine from both ureters (Figure 25.8.3). The bladder lies posterior to the pubic bone and anterior to the rectum. The bladder is partially retroperitoneal (outside the peritoneal cavity) with its peritoneal-covered “dome” projecting into the abdomen when the bladder is distended with urine. When empty, the region of the bladder that does not collapse is called the trigone (Greek tri- = “triangle” and the root of the word “trigonometry”), which is delineated by the opening of the ureters and the urethra, forming a triangular area.
External Website

View the University of Michigan WebScope at http://141.214.65.171/Histology/Urinary%20System/212N_HISTO_40X.svs/view.apml to explore the tissue sample in greater detail.
The bladder is a highly distensible organ comprised of irregular crisscrossing bands of smooth muscle collectively called the detrusor muscle. The interior surface is made of transitional cellular epithelium that is structurally suited for the large volume fluctuations of the bladder. When empty, it resembles columnar epithelia, but when stretched, it “transitions” (hence the name) to a squamous appearance (see Figure 25.8.3). Volumes in adults can range from nearly zero to 500–600 mL.
The detrusor muscle contracts with significant force in the young. The bladder’s strength diminishes with age, but voluntary contractions of abdominal skeletal muscles can increase intra-abdominal pressure to promote more forceful bladder emptying. Such voluntary contraction is also used in forceful defecation and childbirth.
Urethra
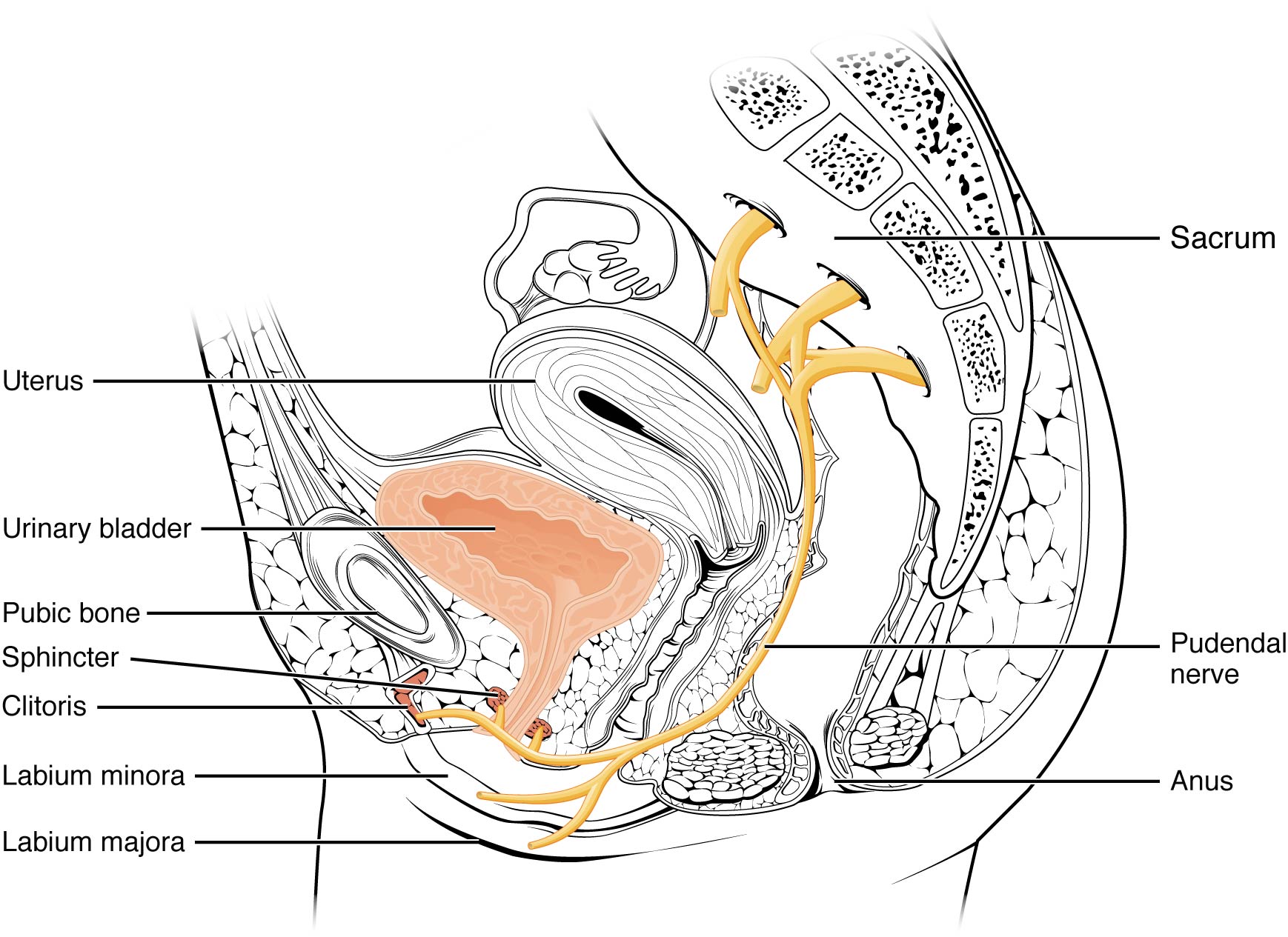
The urethra transports urine from the bladder to the outside of the body for disposal. The urethra is the only urologic organ that shows any significant anatomic difference between males and females; all other urine transport structures are identical (Figure 25.8.4).
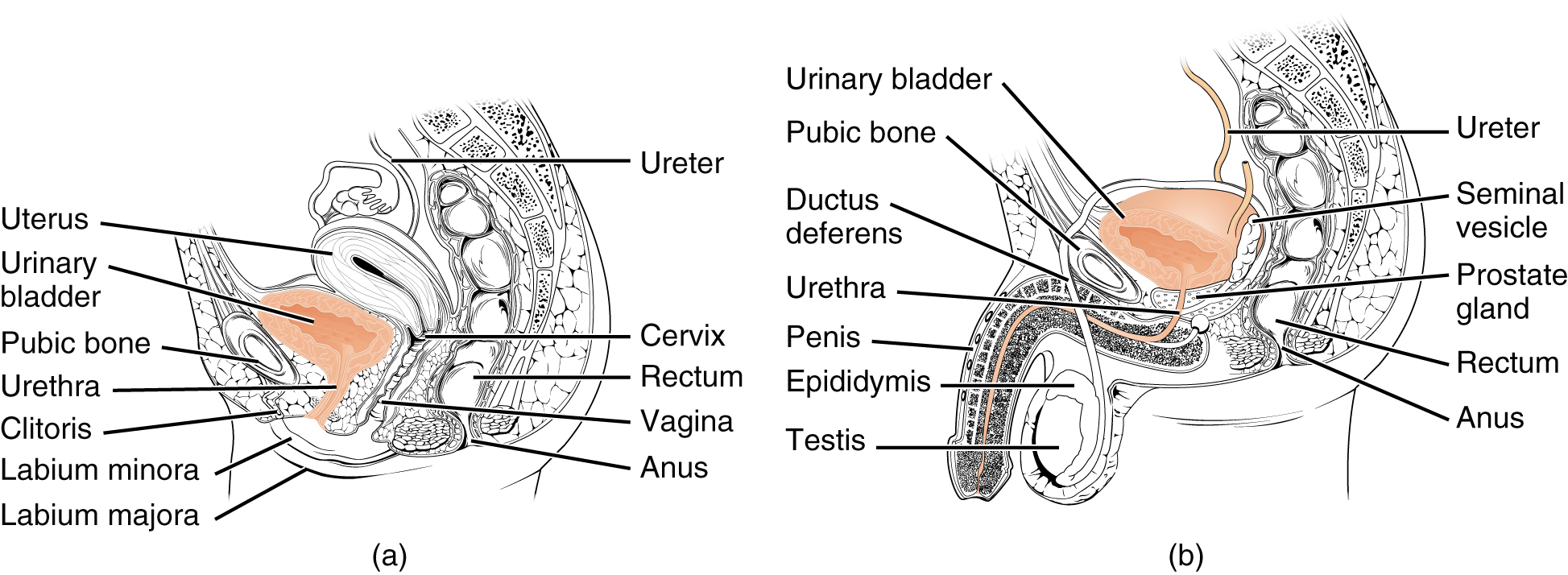
The urethra in both males and females begins inferior and central to the trigone. The urethra tracks posterior and inferior to the pubic symphysis (see Figure 25.8.4a). In both males and females, the proximal urethra is lined by transitional epithelium, whereas the terminal portion is a nonkeratinized, stratified squamous epithelium. In the male, pseudostratified columnar epithelium lines the urethra between these two cell types. Voiding is regulated by an involuntary autonomic nervous system-controlled internal urinary sphincter, consisting of smooth muscle and voluntary skeletal muscle that forms the external urinary sphincter below it. In females, the urethra’s short length, about 4 cm, is less of a barrier to fecal bacteria than the longer male urethra and the best explanation for the greater incidence of UTI in women. Voluntary control of the external urethral sphincter is a function of the pudendal nerve. It arises in the sacral region of the spinal cord, traveling via the S2–S4 nerves of the sacral plexus.
Micturition Reflex
Micturition is the physiological term for urination or voiding. It results from an interplay of involuntary and voluntary actions by the internal and external urethral sphincters. When bladder volume reaches about 150 mL, an urge to void is sensed but is easily overridden. Voluntary control of urination relies on consciously preventing relaxation of the external urethral sphincter to maintain urinary continence. As the bladder fills, subsequent urges become harder to ignore.
Micturition is a result of stretch receptors in the bladder wall that transmit nerve impulses to the sacral region of the spinal cord to generate a spinal reflex. The resulting parasympathetic neural outflow causes contraction of the detrusor muscle and relaxation of the involuntary internal urethral sphincter. At the same time, the spinal cord inhibits somatic motor neurons, resulting in the relaxation of the skeletal muscle of the external urethral sphincter. The micturition reflex is active in infants but with maturity, children learn to override the reflex by asserting external sphincter control, thereby delaying voiding (potty training).
Nerves involved in the control of urination include the hypogastric, pelvic, and pudendal (Figure 25.8.5). Voluntary micturition requires an intact spinal cord and functional pudendal nerve arising from the sacral micturition center. Since the external urinary sphincter is voluntary skeletal muscle, actions by cholinergic neurons maintain contraction (and thereby continence) during filling of the bladder. At the same time, sympathetic nervous activity via the hypogastric nerves suppresses contraction of the detrusor muscle. With further bladder stretch, afferent signals traveling over sacral pelvic nerves activate parasympathetic neurons. This activates efferent neurons to release acetylcholine at the neuromuscular junctions, producing detrusor contraction and bladder emptying.
Chapter Review
The urethra is the only urinary structure that differs significantly between males and females. This is due to the dual role of the male urethra in transporting both urine and semen. The urethra arises from the trigone area at the base of the bladder. Urination is controlled by an involuntary internal sphincter of smooth muscle and a voluntary external sphincter of skeletal muscle. The shorter female urethra contributes to the higher incidence of bladder infections in females. The bladder is largely retroperitoneal and can hold up to 500–600 mL urine. Micturition is the process of voiding the urine and involves both involuntary and voluntary actions. Voluntary control of micturition requires a mature and intact sacral micturition center. It also requires an intact spinal cord. Loss of control of micturition is called incontinence and results in voiding when the bladder contains about 250 mL urine. The ureters are retroperitoneal and lead from the renal pelvis of the kidney to the trigone area at the base of the bladder. A thick muscular wall consisting of longitudinal and circular smooth muscle helps move urine toward the bladder by way of peristaltic contractions.
Review Questions
1. Peristaltic contractions occur in the ________.
- urethra
- bladder
- ureters
- urethra, bladder, and ureters
2. Somatic motor neurons must be ________ to relax the external urethral sphincter to allow urination.
- stimulated
- inhibited
3. Which part of the urinary system is not completely retroperitoneal?
- kidneys
- ureters
- bladder
- nephrons
Critical Thinking Questions
1. Why are females more likely to contract bladder infections than males?
2. Describe how forceful urination is accomplished.
Glossary
- anatomical sphincter
- smooth or skeletal muscle surrounding the lumen of a vessel or hollow organ that can restrict flow when contracted
- detrusor muscle
- smooth muscle in the bladder wall; fibers run in all directions to reduce the size of the organ when emptying it of urine
- external urinary sphincter
- skeletal muscle; must be relaxed consciously to void urine
- internal urinary sphincter
- smooth muscle at the juncture of the bladder and urethra; relaxes as the bladder fills to allow urine into the urethra
- incontinence
- loss of ability to control micturition
- micturition
- also called urination or voiding
- physiological sphincter
- sphincter consisting of circular smooth muscle indistinguishable from adjacent muscle but possessing differential innervations, permitting its function as a sphincter; structurally weak
- retroperitoneal
- outside the peritoneal cavity; in the case of the kidney and ureters, between the parietal peritoneum and the abdominal wall
- sacral micturition center
- group of neurons in the sacral region of the spinal cord that controls urination; acts reflexively unless its action is modified by higher brain centers to allow voluntary urination
- trigone
- area at the base of the bladder marked by the two ureters in the posterior–lateral aspect and the urethral orifice in the anterior aspect oriented like points on a triangle
- urethra
- transports urine from the bladder to the outside environment
Solutions
Answers for Review Questions
- C
- B
- C
Answers for Critical Thinking Questions
- The longer urethra of males means bacteria must travel farther to the bladder to cause an infection.
- Forceful urination is accomplished by contraction of abdominal muscles.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.

