Module 1.2 Supportive Health Care
Learning Objectives
By the end of this module, you should be able to:
- Identify symptoms of infectious disease that is common during early childhood.
- Outline criteria for exclusion from care for ill children and educators.
- Describe considerations programs must make regarding caring for children that are mildly ill.
- Recall licensing requirements for handling medication in early learning and child care programs.
- Explain the communication about illness that should happen between families and early learning and child care programs.
Illness in Early Learning and Child Care Programs
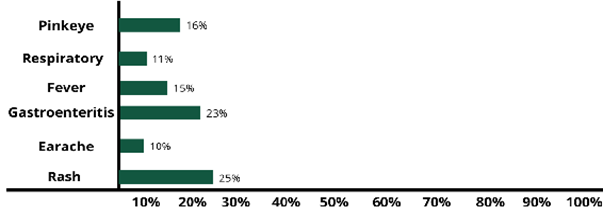
The most frequent infectious disease symptoms that are reported by early learning and child care programs are sore throat, runny nose, shortness of breath or cough, fever, vomiting and diarrhea (gastroenteritis), earaches, and rashes.
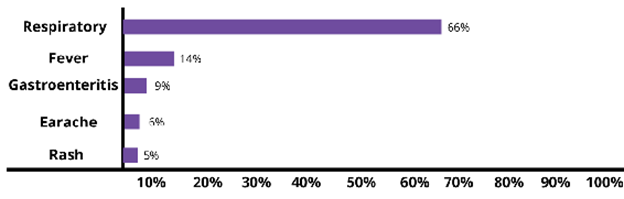
However, these are not the symptoms that necessarily lead to absences. In fact, although respiratory symptoms are most common, it’s rashes and gastrointestinal disease that more often keep children from attending their early learning and child care programs. This is more a reflection of exclusion policies than real risk of serious illness.
It’s important for early learning and child care programs to identify illness accurately and respond in ways that protect all children and staff health (whether it be to allow them to stay in care or to exclude them from care).
Identifying Infectious Disease
When you are familiar with different infectious diseases, it’s easier to identify them in children and know whether children (and educators) who are affected should be excluded from the early learning and child care program.
Common Cold
A child is sneezing and has a stuffy, runny nose. It’s quite likely that they have a common cold. Children get sick many times a year, probably between 4 and 12 times, depending on age and amount of time in child care. Many of these are likely due to the common cold. More than 200 viruses can cause a cold, but rhinoviruses are the most common type.
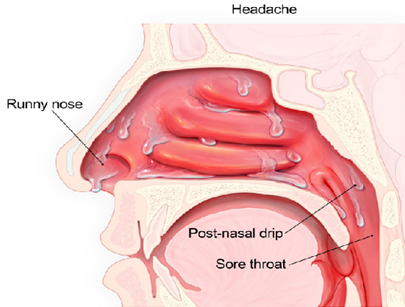
Symptoms of a cold usually peak within 2 to 3 days and can include:
- Sneezing
- Stuffy nose
- Runny nose
- Sore throat
- Coughing
- Mucus dripping down your throat (post-nasal drip)
- Watery eyes
- Fever (although most people with colds do not have fever)
When viruses that cause colds first infect the nose and air-filled pockets in the face (sinuses), the nose makes clear mucus. This helps wash the viruses from the nose and sinuses. After 2 or 3 days, mucus may change to a white, yellow, or green color. This is normal and does not mean an antibiotic is needed. Some symptoms, particularly runny nose, stuffy nose, and cough can last for up to 10 to 14 days, but those symptoms should be improving during that time.
There is no cure for a cold. It will get better on its own—without antibiotics. Because colds can have similar symptoms to flu, it can be difficult to tell the difference between the two illnesses based on symptoms alone. Flu and the common cold are both respiratory illnesses, but they are caused by different viruses.
Influenza (Flu)
In general, flu is worse than a cold, and symptoms are more intense. People with colds are more likely to have a runny or stuffy nose. Colds generally do not result in serious health problems, such as pneumonia, bacterial infections, or hospitalizations. Flu can have very serious associated complications.
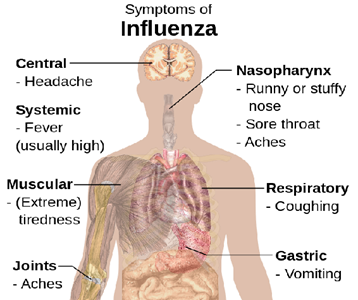
Flu can cause mild to severe illness, and at times can lead to death. Flu usually comes on suddenly. People who have flu often feel some or all these symptoms:
- Fever (common, but not always) or feeling feverish/chills
- Cough
- Sore throat
- Runny or stuffy nose
- Muscle or body aches
- Headaches
- Fatigue (tiredness)
- Some people may have vomiting and diarrhea, though this is more common in children than adults
Most people who get flu will recover in a few days to less than two weeks, but some people will develop complications (such as pneumonia) because of flu, some of which can be life-threatening and result in death.
Sinus and ear infections are examples of moderate complications from flu, while pneumonia is a serious flu complication that can result from either influenza virus infection alone or from co-infection of flu virus and bacteria. Other possible serious complications triggered by flu can include inflammation of the heart (myocarditis), brain (encephalitis) or muscle (myositis, rhabdomyolysis) tissues, and multi-organ failure (for example, respiratory and kidney failure). Flu virus infection of the respiratory tract can trigger an extreme inflammatory response in the body and can lead to sepsis, the body’s life-threatening response to infection. Flu also can make chronic medical problems worse. For example, people with asthma may experience asthma attacks while they have flu.
A yearly flu vaccine is the first and most important step in protecting against influenza and its potentially serious complications for everyone 6 months and older. While there are many different flu viruses, flu vaccines protect against the 3 or 4 viruses that research suggests will be most common. Flu vaccination can reduce flu illnesses, doctors’ visits, missed school due to flu, prevent flu-related hospitalizations, and reduce the risk of dying from influenza. Also, there are data to suggest that even if someone gets sick after vaccination, their illness may be milder.
Once a person has the flu, their health care provider may recommend antiviral drugs. When used for treatment, antiviral drugs can lessen symptoms and shorten the length of sickness by 1 or 2 days. They also can prevent serious flu complications, like pneumonia. For people at high risk of serious flu complications (including children), treatment with antiviral drugs can mean the difference between milder or more serious illness possibly resulting in a hospital stay.
COVID-19
COVID-19 is an infectious disease caused by SARS-CoV-2, the coronavirus that emerged in December 2019. The virus is spread in small liquid particles when an infected person coughs, sneezes, speaks, sings, or breathes. It can take anywhere from 5-14 days for symptoms to show in someone who is infected with the virus.
The most common symptoms include fever, cough, tiredness and loss of taste or smell. Less common symptoms include sore throat, headache, aches and pains, diarrhea, skin rash, discolouration of fingers and toes, red or irritated eyes. Serious symptoms are difficulty breathing or shortness of breath, loss of speech or mobility, confusion, and chest pain (WHO, 2023).
The Government of Ontario has provided guidelines for early learning and childcare programs for:
- Use of masks
- Cleaning practices
- Self-screening
- Ventilation
- COVID-19 testing
Avoiding Spreading Germs to Others
Early learning and childcare programs should teach children and model good cough and sneeze etiquette. Always sneeze or cough into a tissue that is discarded after use. If a tissue is not available, use your upper sleeve, completely covering the mouth and nose. Always wash hands after coughing, sneezing, and blowing noses.

Sinusitis (Sinus Infection)
Sinus infections happen when fluid builds up in the air-filled pockets in the face (sinuses), which allows germs to grow. Viruses cause most sinus infections, but bacteria can cause some sinus infections.
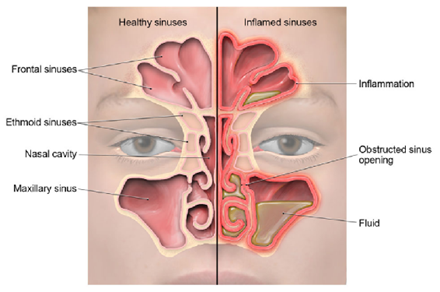
Common symptoms of sinus infections include:
- Runny nose
- Stuffy nose
- Facial pain or pressure
- Headache
- Mucus dripping down the throat (post-nasal drip)
- Sore throat
- Cough
- Bad breath
Most sinus infections usually get better on their own without antibiotics.
Pause to Reflect 💭
What was your last experience with an upper respiratory infection such as cold, flu, or sinus infection?
If a child had the same symptoms as you, would they have needed to be excluded from care?
Sore Throat
A sore throat can make it painful to swallow. A sore throat can also feel dry and scratchy. Sore throat can be a symptom of the common cold, allergies, strep throat, or other upper respiratory tract illness. Strep throat is an infection in the throat and tonsils caused by bacteria called group A Streptococcus (also called Streptococcus pyogenes).
Infections from viruses are the most common cause of sore throats. The following symptoms suggest a virus is the cause of the illness instead of the bacteria called group A strep:
- Cough
- Runny nose
- Hoarseness (changes in your voice that makes it sound breathy, raspy, or strained)
- Conjunctivitis (also called pink eye)
The most common symptoms of strep throat include:
- Sore throat that can start very quickly
- Pain when swallowing
- Fever
- Red and swollen tonsils, sometimes with white patches or streaks of pus
- Tiny red spots on the roof of the mouth
- Swollen lymph nodes in the front of the neck
A doctor can determine the likely cause of a sore throat. If a sore throat is caused by a virus, antibiotics will not help. Most sore throats will get better on their own within one week.
Since bacteria cause strep throat, antibiotics are needed to treat the infection and prevent rheumatic fever and other complications. A doctor cannot tell if someone has strep throat just by looking in the throat. If a doctor suspects strep throat, they may test to confirm diagnosis.
Ear Infection
There are different types of ear infections. Middle ear infection (acute otitis media) is an infection in the middle ear.
Another condition that affects the middle ear is called otitis media with effusion. It occurs when fluid builds up in the middle ear without being infected and without causing fever, ear pain, or pus build-up in the middle ear.
When the outer ear canal is infected, the condition is called swimmer’s ear, which is different from a middle ear infection.
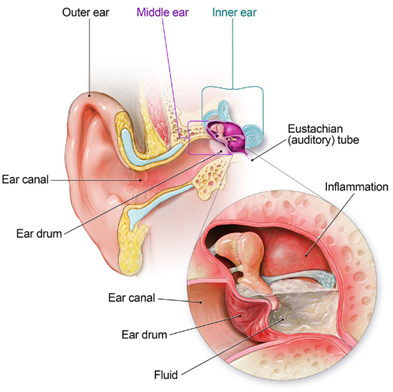
Middle Ear Infection
A middle ear infection may be caused by:
- Bacteria, like Streptococcus pneumoniaeand Haemophilus influenza (nontypeable) – the two most common bacterial causes
- Viruses, like those that cause colds or flu
Common symptoms of middle ear infection in children can include:
- Ear pain
- Fever
- Fussiness or irritability
- Rubbing or tugging at an ear
- Difficulty sleeping
A doctor can make the diagnosis of a middle ear infection by looking inside the child’s ear to examine the eardrum and see if there is pus in the middle ear. Antibiotics are often not needed for middle ear infections because the body’s immune system can fight off the infection on its own. However, sometimes antibiotics, such as amoxicillin, are needed to treat severe cases right away or cases that last longer than 2 – 3 days.
Swimmer’s Ear
Ear infections can be caused by leaving contaminated water in the ear after swimming. This infection, known as “swimmer’s ear” or otitis externa, is different from the common childhood middle ear infection. The infection occurs in the outer ear canal and can cause pain and discomfort for swimmers of all ages.
Symptoms of swimmer’s ear usually appear within a few days of swimming and include:
- Itchiness inside the ear.
- Redness and swelling of the ear.
- Pain when the infected ear is tugged or when pressure is placed on the ear.
- Pus draining from the infected ear.
Although all age groups are affected by swimmer’s ear, it is more common in children and can be extremely painful. If swimmer’s ear is suspected, a healthcare provider should be consulted. Swimmer’s ear can be treated with antibiotic ear drops.
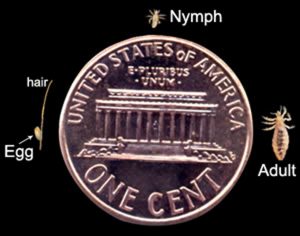
Head Lice
Head lice are parasitic insects that live on the head. They survive by feeding on human blood. Lice infestations are spread most by close person-to-person contact. Adult head lice are 2 – 3 mm in length. Head lice infest the head and neck and attach their eggs to the base of the hair shaft. Lice move by crawling; they cannot hop or fly.
Symptoms of a head lice infestation include:
- Tickling feeling of something moving in the hair.
- Itching, caused by an allergic reaction to the bites of the head louse.
- Irritability and difficulty sleeping; head lice are most active in the dark.
- Sores on the head caused by scratching. These sores can sometimes become infected with bacteria found on the person’s skin.
Head-to-head contact with a person who already has an infestation is the most common way to get head lice. Head-to-head contact is common during play at school, at home, and elsewhere (sports activities, playground, slumber parties, camp).
Although uncommon, head lice can be spread by sharing clothing or belongings. This happens when lice crawl, or the nits that are attached to shed hair hatch and get on the shared clothing or belongings. Examples include:
- Sharing clothing (hats, scarves, coats, sports uniforms) or articles (hair ribbons, barrettes, combs, brushes, towels, stuffed animals) recently worn or used by a person with an infestation.
- Lying on a bed, couch, pillow, or carpet that has recently been in contact with a person with an infestation.
Dogs, cats, and other pets do not play a role in the spread of head lice.
The diagnosis of a head lice infestation is best made by finding a live nymph or adult louse on the scalp or hair of a person. Because nymphs and adult lice are very small, move quickly, and avoid light, they can be difficult to find. Use of a magnifying lens and a fine-toothed comb may be helpful to find live lice.
If crawling lice are not seen, finding nits firmly attached within a ¼ inch of base of the hair shafts strongly suggests, but does not confirm, that a person is infested and should be treated. Nits that are attached more than ¼ inch from the base of the hair shaft are almost always dead or already hatched. Nits are often confused with other things found in the hair such as dandruff, hair spray droplets, and dirt particles. If no live nymphs or adult lice are seen, and the only nits found are more than ¼-inch from the scalp, the infestation is probably old and no longer active and does not need to be treated.
Treatment for head lice is recommended for persons diagnosed with an active infestation. All household members and other close contacts should be checked; those persons with evidence of an active infestation should be treated with an over the counter or prescription medication (following the provided instructions).
Hats, scarves, pillow cases, bedding, clothing, and towels worn or used by the person with the infestation in the 2-day period just before treatment is started can be machine washed and dried using the hot water and hot air cycles because lice and eggs are killed by exposure for 5 minutes to temperatures greater than 128.3°F. Items that cannot be laundered may be dry-cleaned or sealed in a plastic bag for two weeks. Items such as hats, grooming aids, and towels that come in contact with the hair of a person with an infestation should not be shared. Vacuuming furniture and floors can remove hairs that might have viable nits attached. Head lice do not survive long if they fall off a person and cannot feed.
After treatment, it’s important to check the hair and comb with a nit comb to remove nits and lice every 2–3 days which will decrease the chance of self–reinfestation. Checking for 2–3 weeks will ensure that all lice and nits are gone.
Personal hygiene or cleanliness in the home or school has nothing to do with getting head lice. According to the Canadian Paediatric Society “Children with head lice should be treated and then attend school or childcare as usual. ‘No-nit’ policies that keep children with head lice or nits after treatment away from school are not necessary because:
- Head lice are common among young children. Many days of school would be missed if children had to stay home.
- People are often wrong when they think a child has head lice. It would be unfortunate to see children missing school when they don’t really have lice.
- Making children stay at home will not get rid of head lice. Often, other children in the class have lice but don’t have any symptoms. Without treatment, they will continue to spread lice.
- Head lice don’t spread disease. They are a nuisance and unpleasant, but they are not dangerous.” (Canadian Paediatric Society, 2022)
Pause to Reflect 💭
What experiences with or knowledge do you have about policies that specific early learning and childcare programs and schools have on head lice?
Are (or were) those policies “no nits” or in line with the recommendations above?
Other Illnesses
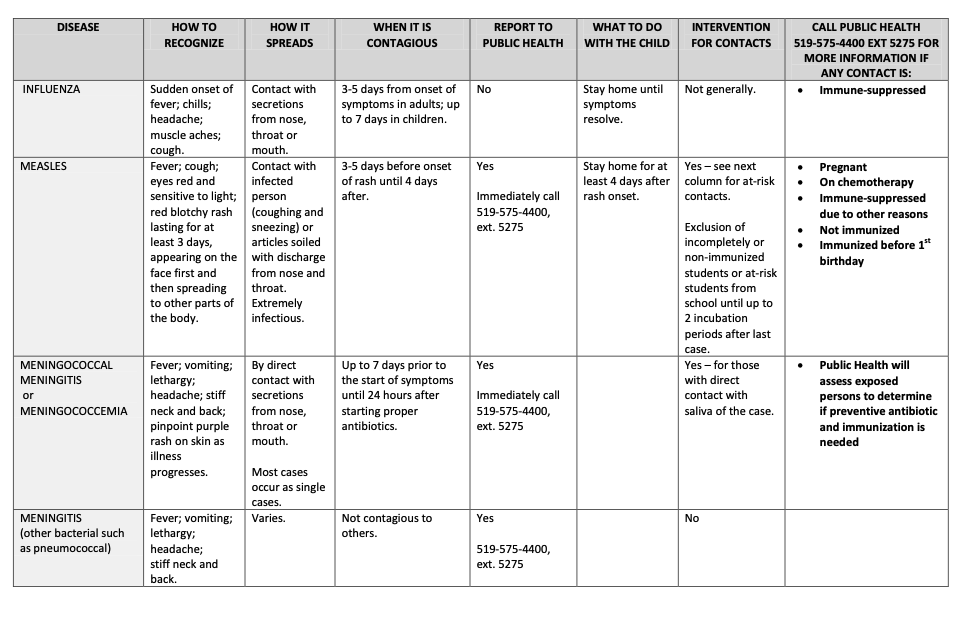
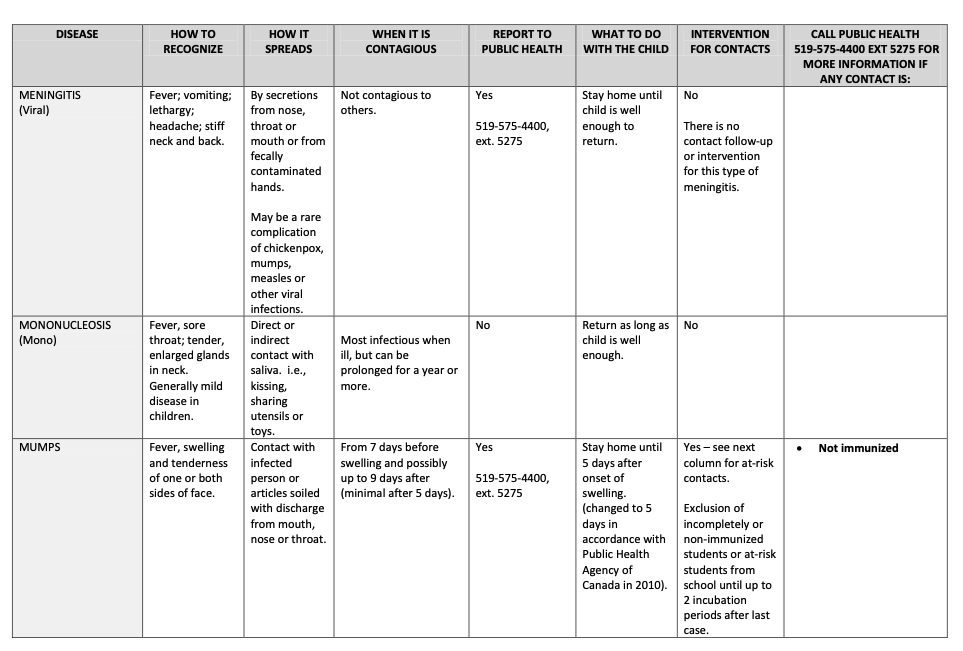
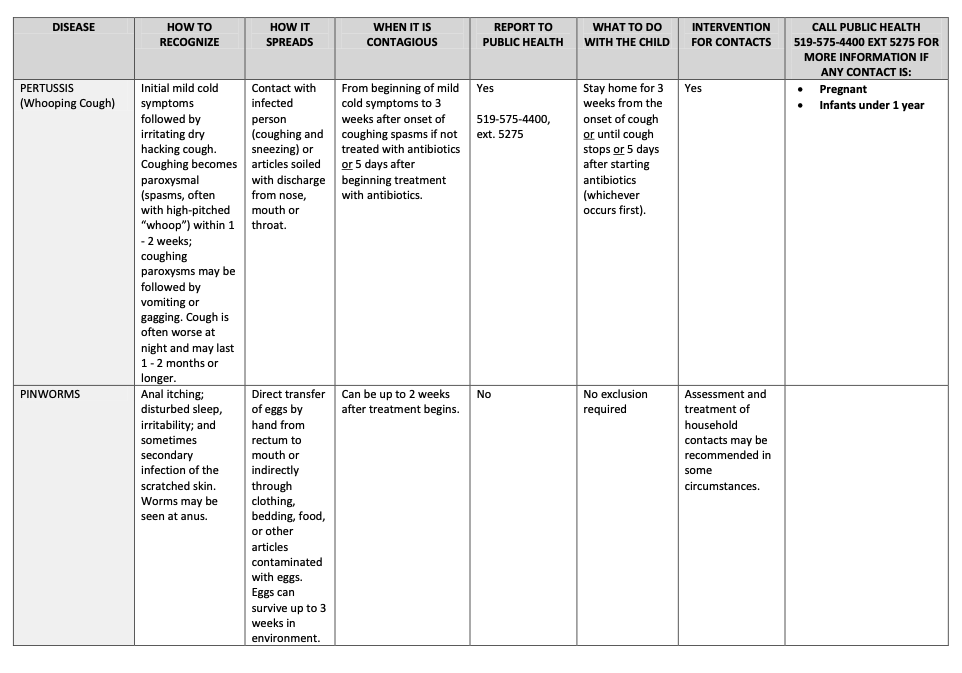
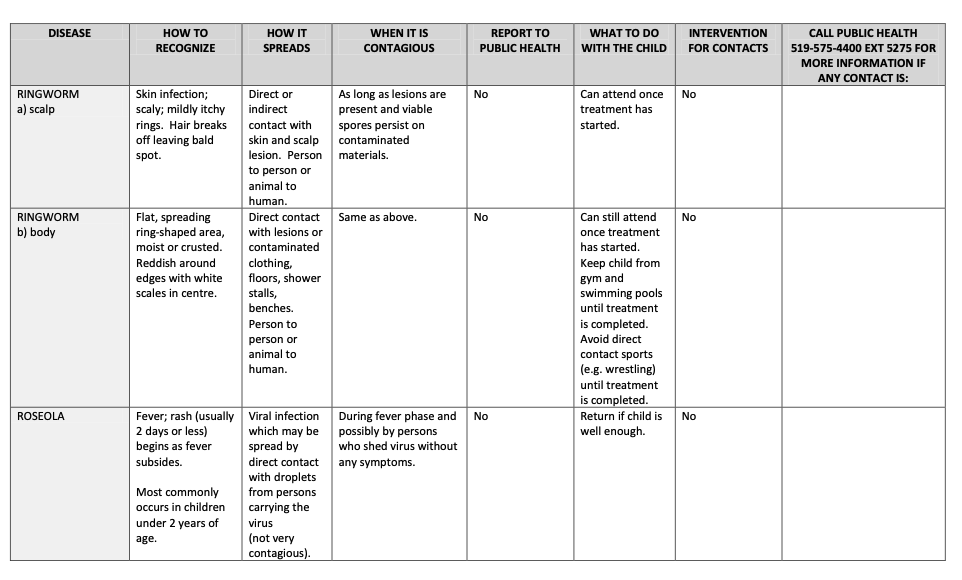
To learn more about the following illnesses, go to Appendix A at the end of Module 1.2.
- Bronchitis
- Chickenpox
- Conjunctivitis (Pink Eye)
- Fifth Disease (Slapped Cheek)
- Hand, Foot, and Mouth Disease
- Hepatitis A
- Impetigo
- Measles
- Meningitis
- Molluscum Contagiosum
- Mumps
- Norovirus
- Pertussis
- Pinworms
- Respiratory Syncytial Virus
- Ringworm
- Roseola
- Rotavirus
- Rubella (German Measles)
- Shigella
- Tuberculosis
Danger of Infectious Disease for Adults
Because early learning and childcare program employees are around children who are at higher risk of infectious diseases and have limited understanding of hygiene practices, those employees are also at greater risk for getting sick.
While most illness that are spread in early learning and childcare programs are not serious, some can be very dangerous. Knowledge about illness and how to prevent its spread helps. Being fully immunized (from childhood illness and or vaccines) protects adult health as well.
Employees that are or could become pregnant want to be especially careful because first time exposure to chickenpox, cytomegalovirus (CMV), Fifths disease, and Rubella can cause major damage to fetal health, birth defects, and even fetal death.
Reportable Diseases
Some diseases are enough of a threat to the community that it is required that diagnosed cases are reported to Public Health Ontario. For a complete list of reportable diseases, go to Public Health Ontario Reportable Diseases.
Exclusion Policies
Most children with mild illnesses can safely attend childcare. “Many health policies concerning the care of ill children [including exclusion policies] have been based upon common misunderstandings about contagion, risks to ill children, and risks to other children and staff. Current research clearly shows that certain ill children do not pose a health threat. Also, the research shows that keeping certain other mildly ill children at home or isolated at the childcare setting will not prevent other children from becoming ill.” (California Childcare Health Program, 2018)
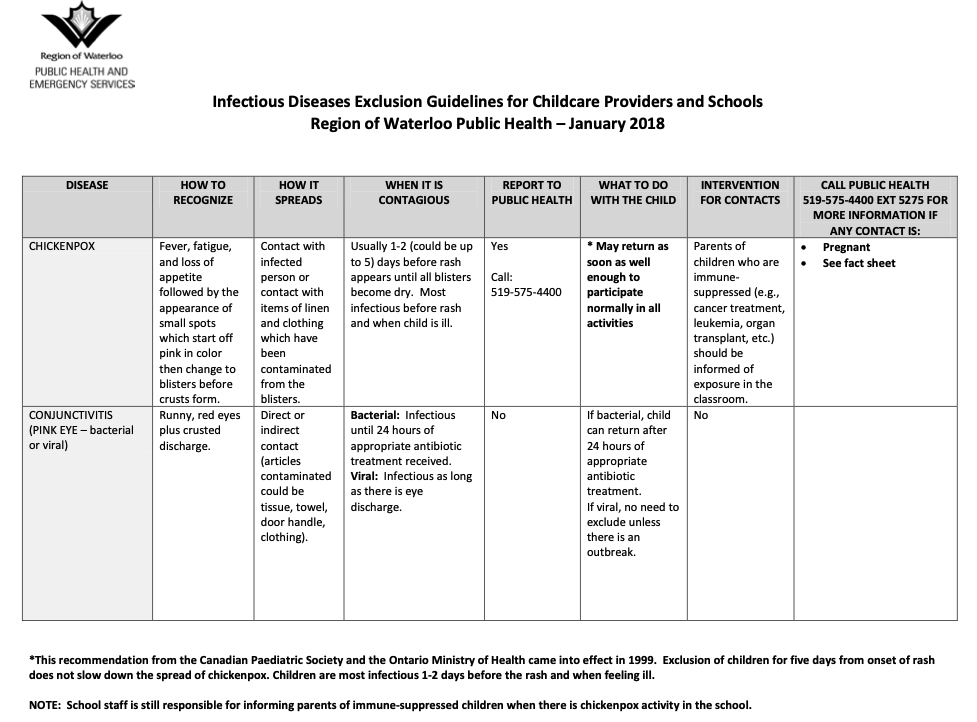
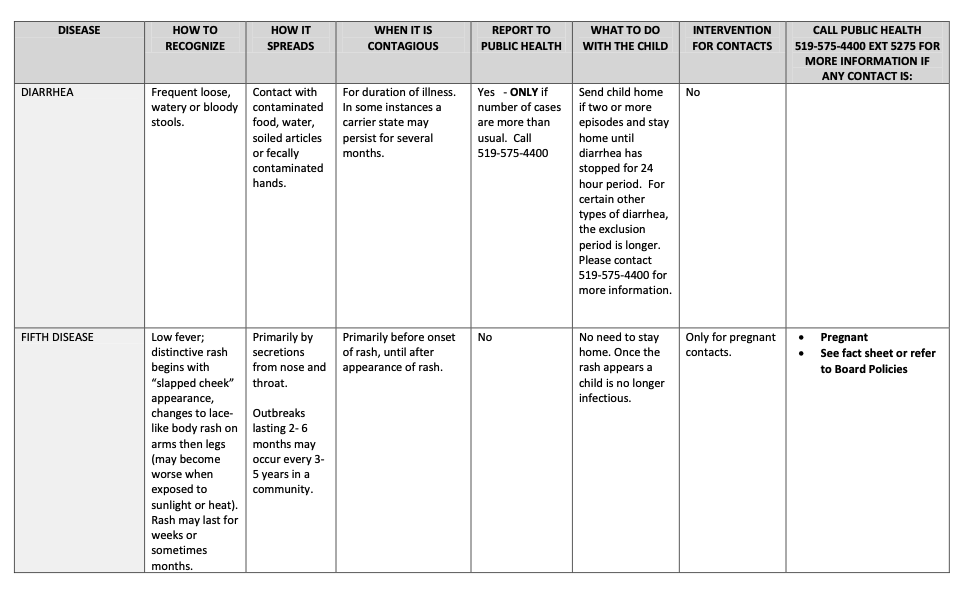
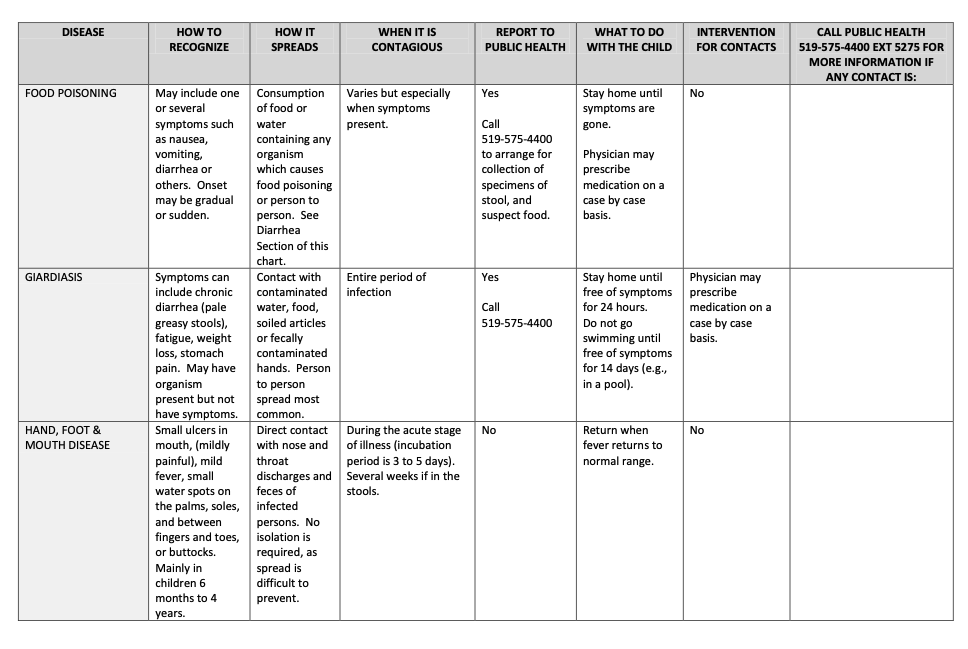
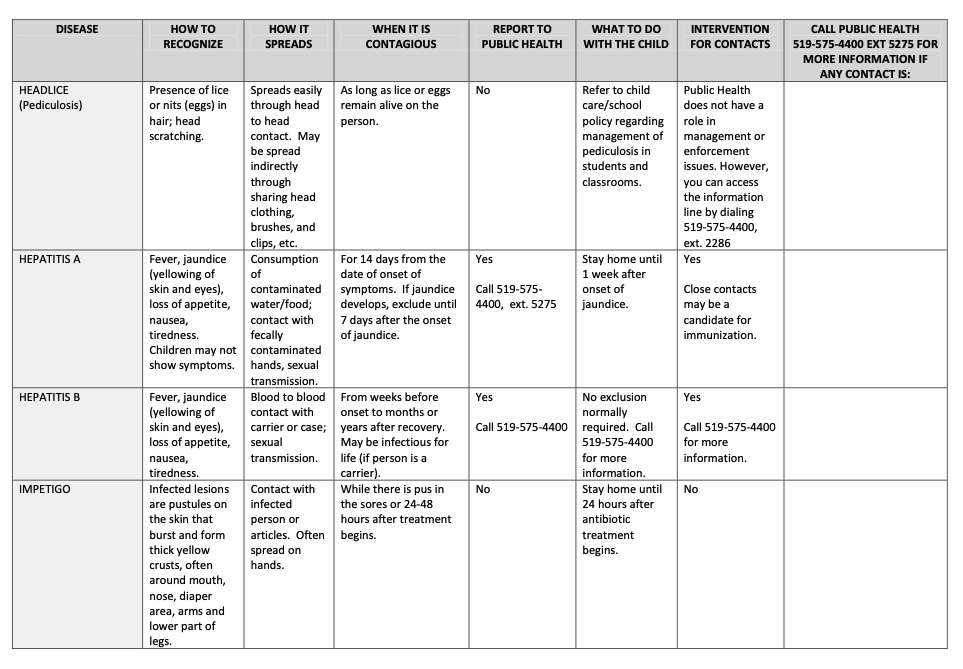
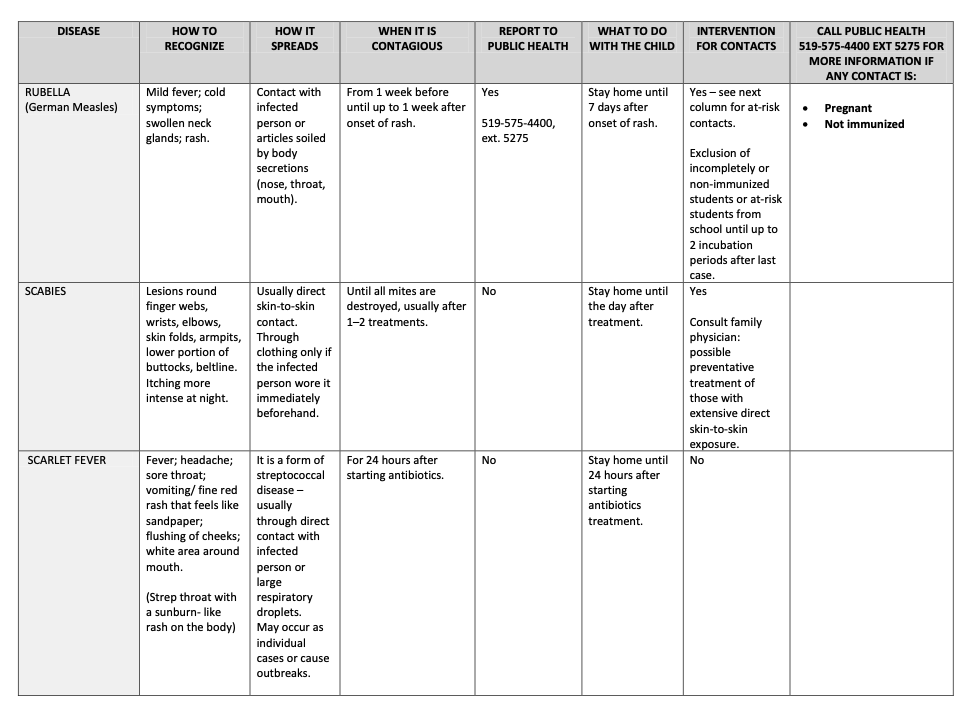
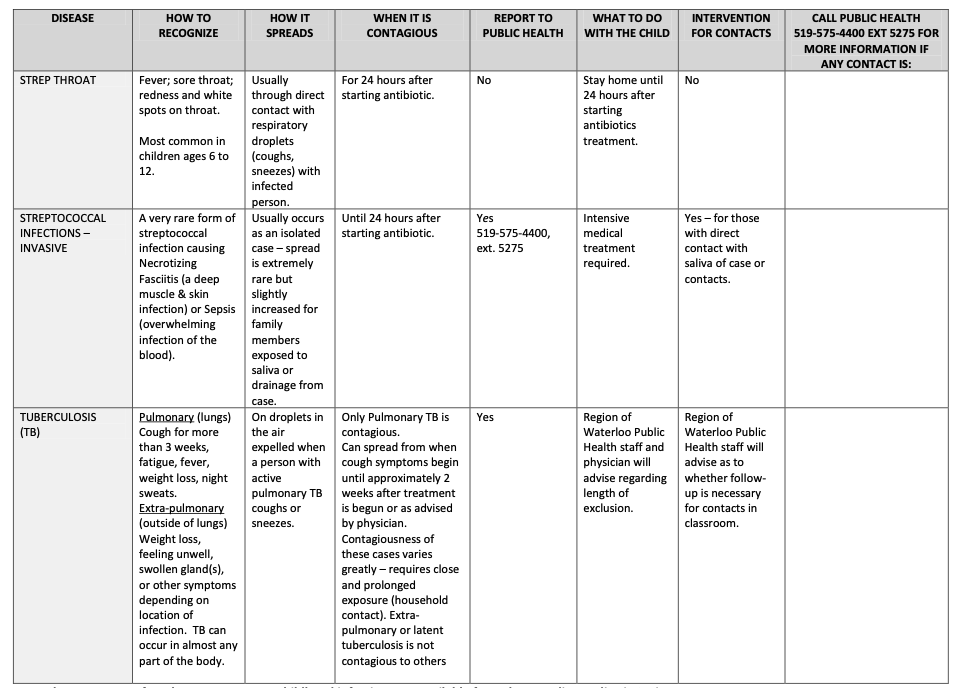
See Appendix B at the end of Module 1.2 for the Region of Waterloo Public Health Infectious Diseases Exclusion Guidelines for Childcare Providers and Schools. Please note that policies may differ between Public Health Units.
What to do When a Child Requires Exclusion
When a child becomes ill enough to be excluded, they should be immediately isolated from other children.
36.(1) Every licensee shall ensure that a daily observation is made of each child receiving childcare in each childcare centre it operates and in each premises where it oversees the provision of home childcare before the child begins to associate with other children in order to detect possible symptoms of ill health.
(2) Every licensee shall ensure that where a child receiving childcare at a childcare centre it operates or at a premises where it oversees the provision of home childcare appears to be ill, the child is separated from other children and the symptoms of the illness noted in the child’s records.
(3) Where a child is separated from other children because of a suspected illness, the licensee shall ensure that,
(a) a parent of the child takes the child home; or
(b) where it is not possible for a parent of the child to take the child home or where it appears that the child requires immediate medical attention, the child is examined by a legally qualified medical practitioner or a nurse registered with the College of Nurses of Ontario. (O. Reg. 137/15: General)
The child’s authorized emergency contact shall be notified immediately when the child becomes ill enough to require isolation and shall be asked to have the child picked up from the center as soon as possible.
Pause to Reflect 💭
Consider the following situations. Should each child be excluded from care nor not? If so, why and when should the child return? If not, what should the educator do?
- Mario’s dad drops them off and lets Ms. Michelle know that they are a little under the weather. They are not running a fever but have a mild cough and a runny nose. But they ate a good breakfast and have a pretty typical level of energy.
- About an hour into the day, Li vomits. Mr. Abraham checks and they have a fever of 101.30. They look a little pale and just want to lay down. As they go to call Li’s family, Li vomits again.
- When Latanya goes to change Daniel’s diaper, they notice a rash on their stomach. They check his temperature, and they are not running a fever. They are not scratching at it or seemingly in any discomfort. They remember that they have a history of eczema and contact dermatitis.
- Apurva wakes up from naptime with discharge coming from a slightly swollen and bloodshot right eye. They tell Ms. Maria that their eye hurts and is “kind of itchy.”
- Now come up with your own examples of a child that should be excluded from care and that should not automatically be excluded.
Caring for Mildly Ill Children
Because young in early learning and childcare programs have high incidence of illness and may have conditions (such as eczema and asthmas), providers should be prepared to care for mildly ill children, at least temporarily. And since we know that excluding most mildly ill children doesn’t prevent the spread of illness and can have negative effects on families, programs should consider whether they can care for children with mild symptoms (not meeting the exclusion policy).
It’s important that programs recognize the families must weigh many things when trying to decide whether to send a child to childcare. They must consider how the child feels (physically and emotionally), whether the program can provide care for the specific needs of the child, what alternative care arrangements are available, as well as the income they may lose if they have to stay home.
Responding to Illness that Requires Medical Care
Some conditions, require immediate medical help. If the parents or designated emergency contact can be reached, tell them to come right away and to notify their medical provider.
Call Emergency Medical services (9-1-1) immediately and notify parents or the designated emergency contact if any of the following things happen:
- You believe a child needs immediate medical assessment and treatment that cannot wait for parents to take the child for care.
- A child has a stiff neck (that limits his ability to put his chin to his chest) or severe headache and fever.
- A child has a seizure for the first time.
- A child who has a fever as well as difficulty breathing.
- A child looks or acts very ill or seems to be getting worse quickly.
- A child has skin or lips that look blue, purple, or gray.
- A child is having difficulty breathing or breathes so fast or hard that they cannot play, talk, cry or drink.
- A child who is vomiting blood.
- A child complains of a headache or feeling nauseous, or is less alert or more confused, after a hard blow to the head.
- Multiple children have injuries or serious illness at the same time.
- A child has a large volume of blood in the stools.
- A child has a suddenly spreading blood-red or purple rash.
- A child acts unusually confused.
- A child is unresponsive or has decreasing responsiveness.
Tell the parents or designated emergency contact to come right away, and get medical help immediately, when any of the following things happen. If the parents or the designated emergency contact or the child’s medical provider is not immediately available, call 9-1-1 (EMS, Emergency Medical Services) for immediate help:
- A fever in any child who appears more than mildly ill.
- An infant under 2 months of age has an axillary (“armpit”) temperature above 100.4º F.
- An infant under four months of age has two or more forceful vomiting episodes (not the simple return of swallowed milk or spit-up) after eating.
- A child has neck pain when the head is moved or touched.
- A child has a severe stomach-ache that causes the child to double up and scream.
- A child has a stomach-ache without vomiting or diarrhea after a recent injury, blow to the abdomen or hard fall.
- A child has stools that are black or have blood mixed through them.
- A child has not urinated in more than eight hours, and the mouth and tongue look dry.
- A child has continuous, clear drainage from the nose after a hard blow to the head.
- A child has a medical condition outlined in his special care plan as requiring medical attention.
- A child has an injury that may require medical treatment such as a cut that does not hold together after it is cleaned.” (California Childcare Health Program, 2018)
Indigenous Perspective
Indigenous cultures often refer to a holistic approach to healing practices. This may include herbal remedies to minor illnesses.
Important Things to Remember
- Rashes, vomiting, and diarrhea results in the most absences from care as they are highly contagious.
- Identifying ear infections can be difficult, typically by a change in behaviour.
- Personal hygiene or cleanliness in the home or school has nothing to do with getting head lice, it comes from close contact with those infected.
- Being fully immunized (from childhood illness and or vaccines) protects adult health as well.
- Employees that are or could become pregnant want to be especially careful, as some illnesses can cause major damage to fetal health.
- O. Reg. 137/15: GENERAL, made under The Childcare and Early Years Act (CCEYA), identifies when a child needs to be excluded from programing and guides policies and procedures for Ontario early learning environments.
Resources for Further Exploration
Public Health Agency of Canada
COVID-19: health and safety measures for child care
Health conditions and treatments
10 Simple Steps to Prevent Infections During Pregnancy
Health Topics FAQ and Fact Sheets (Hastings Prince Edward Health Unit)
References
- California Childcare Health Program. (2018). Preventive Health and Safety in the Child Care Setting: A Curriculum for the Training of Child Care Providers (3rd ed.). University of California, San Francisco. https://cchp.ucsf.edu/sites/g/files/tkssra181/f/PHT-Handbook-Student-2018-FINAL.pdf
- Canadian Paediatric Society (2022). Head Lice. https://caringforkids.cps.ca/handouts/health-conditions-and-treatments/head_lice
- O. Reg. 137/15: General. https://www.ontario.ca/laws/regulation/150137
- World Health Organization (2023). Coronavirus disease (COVID-19). https://www.who.int/health-topics/coronavirus#tab=tab_3
Appendix A: Additional Infectious Disease Information |
Bronchitis (Chest Cold)
A chest cold occurs when the airways of the lungs swell and produce mucus in the lungs. That’s what produces the cough. A chest cold, often called acute bronchitis, lasts less than 3 weeks and is the most common type of bronchitis.
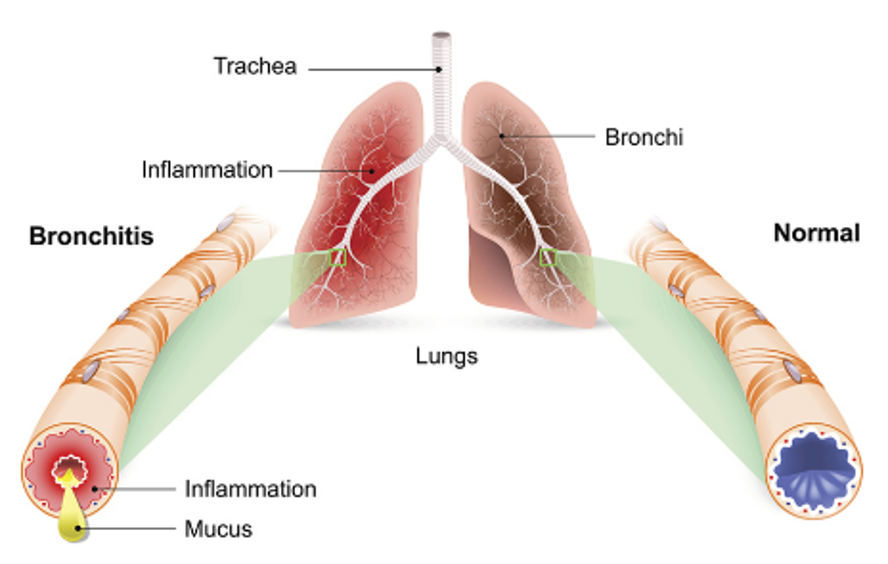
Acute bronchitis is usually caused by a virus and often occurs after an upper respiratory infection. Bacteria can sometimes cause acute bronchitis, but even in these cases, antibiotics are NOT recommended and will not help an infected person get better.
Symptoms of acute bronchitis last less than 3 weeks and can include:
- Coughing with or without mucus
- Soreness in the chest
- Feeling tired (fatigue)
- Mild headache
- Mild body aches
- Sore throat
Most chest colds will get better on their own within one week.
Chickenpox
Chickenpox is a highly contagious disease caused by the varicella-zoster virus (VZV). It can cause an itchy, blister-like rash. The rash first appears on the chest, back, and face, and then spreads over the entire body, causing between 250 and 500 itchy blisters. Chickenpox can be serious, especially in babies, adolescents, adults, pregnant women, and people with a weakened immune system. The best way to prevent chickenpox is to get the chickenpox vaccine.
The classic symptom of chickenpox is a rash that turns into itchy, fluid-filled blisters that eventually turn into scabs. The rash may first show up on the chest, back, and face, and then spread over the entire body, including inside the mouth, eyelids, or genital area. It usually takes about one week for all of the blisters to become scabs.

Other typical symptoms that may begin to appear 1-2 days before rash include:
- Fever
- Tiredness
- Loss of appetite
- Headache774
The virus spreads mainly through close contact with someone who has chickenpox (or shingles). It takes about 2 weeks (from 10 to 21 days) after exposure to a person with chickenpox or shingles for someone to develop chickenpox. A person with chickenpox is contagious beginning 1 to 2 days before rash onset until all the chickenpox lesions have crusted (scabbed).
Conjunctivitis (Pink Eye)
Pink eye, or conjunctivitis, is one of the most common and treatable eye conditions in the world. It can affect both children and adults. It is an inflammation of the thin, clear tissue that lines the inside of the eyelid (conjunctiva) and the white part of the eyeball. This inflammation makes blood vessels more visible and gives the eye a pink or reddish colour.
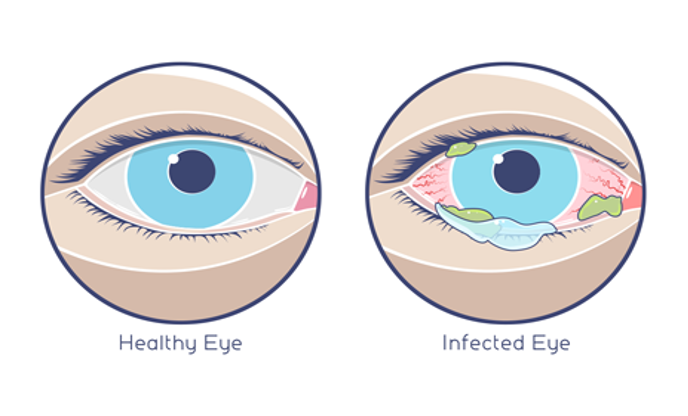
The symptoms may vary, but usually include:
- Redness or swelling of the white of the eye or inside the eyelids
- Increased amount of tears
- Eye discharge which may be clear, yellow, white, or green
- Itchy, irritated, and/or burning eyes
- Gritty feeling in the eye
- Crusting of the eyelids or lashes
- Contact lenses that feel uncomfortable and/or do not stay in place on the eye
There are four main causes of pink eye:
- Viruses
- Bacteria
- Allergens (like pet dander or dust mites)
- Irritants (like smog or swimming pool chlorine) that infect or irritate the eye and eyelid lining
It can be difficult to determine the exact cause of pink eye because some signs and symptoms may be the same no matter the cause. When pink eye is caused by a virus or bacteria, it is very contagious. It can spread easily and quickly from person to person (through contact with the discharge from the infected eye). Pink eye caused by allergens or irritants is not contagious.
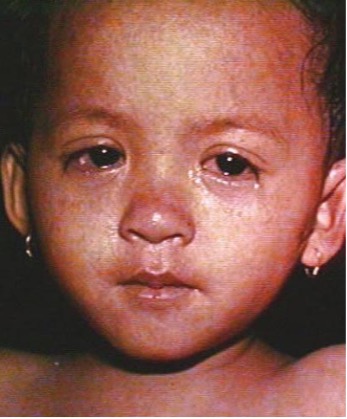
Fifth Disease (Slapped Cheek)
Fifth disease is a mild rash illness caused by parvovirus B19. It is more common in children than adults. A person usually gets sick with fifth disease within 14 days after getting infected with parvovirus B19.
The symptoms of fifth disease are usually mild and may include
- Fever
- Runny nose
- Headache
- Rash (on face and body)

Parvovirus B19—which causes fifth disease—spreads through respiratory secretions, such as saliva, sputum, or nasal mucus, when an infected person coughs or sneezes. You are most contagious when it seems like you have “just a fever and/or cold” and before you get the rash or joint pain and swelling. After you get the rash, you are not likely to be contagious. Fifth disease is usually mild and will go away on its own. Children and adults who are otherwise healthy usually recover completely.
Hand, Foot and Mouth Disease
Hand-foot-mouth disease is a common viral infection that most often begins in the throat. Hand-foot-mouth disease (HFMD) is most caused by a virus called coxsackievirus A16. Children under age 10 are most often affected.
Symptoms of HFMD include:
- Fever
- Headache
- Loss of appetite
- Rash with very small blisters on the hands, feet, and diaper area that may be tender or painful when pressed
- Sore throat
- Ulcers in the throat (including tonsils), mouth, and tongue


The virus can spread from person-to-person through tiny, air droplets that are released when the sick person sneezes, coughs, or blows their nose. You can catch hand-foot-mouth disease if:
- A person with the infection sneezes, coughs, or blows their nose near you.
- You touch your nose, eyes, or mouth after you have touched something contaminated by the virus, such as a toy or doorknob.
- You touch stools or fluid from the blisters of an infected person.
The virus is most easily spread the first week a person has the disease. The time between contact with the virus and the start of symptoms is about 3 to 7 days. Children with hand-foot-and-mouth disease usually do not need treatment and will get better on their own within a week.
Hepatitis A
Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus. It can range from a mild illness lasting a few weeks to a severe illness lasting several months. Although rare, hepatitis A can cause death in some people.
What is the difference between hepatitis A, hepatitis B, and hepatitis C?
Hepatitis A, hepatitis B, and hepatitis C are liver infections caused by three different viruses. Although each can cause similar symptoms, they have different modes of transmission and can affect the liver differently. Hepatitis A is usually a short-term infection and does not become chronic. Hepatitis B and hepatitis C can also begin as short-term, acute infections, but in some people, the virus remains in the body, resulting in chronic disease and long-term liver problems. There are vaccines to prevent hepatitis A and hepatitis B; however, there is no vaccine for hepatitis C.
Most children younger than age 6 do not have symptoms when they have hepatitis A. Older children and adults typically have symptoms. If symptoms develop, they usually start appearing 4 weeks after exposure, but can occur as early as 2 and as late as 7 weeks after exposure. Symptoms usually develop over a period of several days and can include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Diarrhea
- Clay-colored stools
- Joint pain
- Jaundice (yellowing of the skin and eyes)
Hepatitis A usually spreads when a person unknowingly ingests the virus from objects, food, or drinks contaminated by small, undetected amounts of stool from an infected person. A person can transmit the virus to others up to 2 weeks before symptoms appear.
Impetigo
Impetigo is a common contagious skin infection that may be caused by two germs—Streptococcus pyogenes and Staphylococcus aureus. Recommended treatment depends on which germs are causing impetigo. With the right treatment, impetigo usually goes away within two to three weeks.
The signs of impetigo include red sores that pop easily and leave a yellow crust, fluid-filled blisters, itchy rash, skin lesions, and swollen lymph nodes. The sores can be uncomfortable and painful.

Impetigo is typically spread through skin-to-skin contact with an individual who has impetigo, but it can also be spread by contact with objects someone with impetigo has touched (for example, towels, blankets, and toys).
Measles
Measles is a serious illness caused by a virus. The virus can last for one to two weeks. It is rare today because most children are immunized against it. However, the number of diagnosed cases has grown across the country. This increase is related to children not being vaccinated.
Measles starts with a fever that can get very high. Some of the other symptoms that may occur are:
- Fatigue
- Cough, runny nose, and red, watery eyes
- Rash of tiny, red spots that usually lasts five to six days, (the rash begins at the hairline, moves to the face and upper neck, and proceeds down the body)
- Diarrhea
- Ear infection
Measles spreads when a person infected with the measles virus breathes, coughs, or sneezes. It is very contagious from five days before until four days after the start of the rash. After exposure, it can take one to two weeks for the person to get sick.
Measles can spread by being in a room with a person with measles and up to two hours after that person is gone. It can also spread from an infected person even before they have a measles rash. Almost everyone who has not had the measles vaccine will get measles if they are exposed to the measles virus. People who have had measles or were immunized usually can’t catch it again.
Meningitis
Meningitis is inflammation of the thin tissue that surrounds the brain and spinal cord, called the meninges. There are several types of meningitis. The most common is viral meningitis. You get it when a virus enters the body through the nose or mouth and travels to the brain. Bacterial meningitis is rare but can be deadly. It usually starts with bacteria that cause a cold-like infection. It can cause stroke, hearing loss, and brain damage. It can also harm other organs. Pneumococcal infections and meningococcal infections are the most common causes of bacterial meningitis.
Other rare forms of meningitis include fungal meningitis, parasitic meningitis, amebic meningitis, and non-infectious meningitis. Children with meningitis generally feel too ill to attend childcare.
Molluscum Contagiosum
Molluscum contagiosum is an infection caused by a poxvirus (molluscum contagiosum virus). The result of the infection is usually a benign, mild skin disease characterized by lesions (growths) that may appear anywhere on the body. Within 6-12 months, Molluscum contagiosum typically resolves without scarring but may take as long as 4 years.
The lesions, known as Mollusca, are small, raised, and usually white, pink, or flesh-colored with a dimple or pit in the center. They often have a pearly appearance. They’re usually smooth and firm. In most people, the lesions range from about the size of a pinhead to as large as a pencil eraser (2 to 5 millimeters in diameter). They may become itchy, sore, red, and/or swollen.

Mollusca may occur anywhere on the body including the face, neck, arms, legs, abdomen, and genital area, alone or in groups. The lesions are rarely found on the palms of the hands or the soles of the feet.
Mumps
Mumps is best known for the puffy cheeks and tender, swollen jaw that it causes. It is one of the diseases that is vaccine preventable. This is a result of swollen salivary glands under the ears on one or both sides, often referred to as parotitis.

Other symptoms that might begin a few days before parotitis include:
- Fever
- Headache
- Muscle aches
- Tiredness
- Loss of appetite
Symptoms typically appear 16 – 18 days after infection, but this period can range from 12 – 25 days after infection.Some people who get mumps have very mild symptoms (like a cold), or no symptoms at all and may not know they have the disease. In rare cases, mumps can cause more severe complications. Most people with mumps recover completely within two weeks.
Mumps is a contagious disease caused by a virus. It spreads through direct contact with saliva or respiratory droplets from the mouth, nose, or throat. An infected person can likely spread mumps from a few days before their salivary glands begin to swell to up to five days after the swelling begins.
Norovirus
Norovirus is the most common cause of vomiting and diarrhea, and foodborne illness.
The most common symptoms of norovirus are:
- Diarrhea
- Vomiting
- Nausea
- Stomach pain
Other symptoms include fever, headache, and body aches.
Norovirus causes inflammation of the stomach or intestines. This is called acute gastroenteritis.
A person usually develops symptoms 12 to 48 hours after being exposed to norovirus. Most people with norovirus illness get better within 1 to 3 days.
If you have norovirus illness, you can feel extremely ill, and vomit or have diarrhea many times a day. This can lead to dehydration, especially in young children, older adults, and people with other illnesses.
You can get norovirus by accidentally getting tiny particles of feces or vomit from an infected person in your mouth. This can happen through contaminated food and water, touching contaminated surfaces and then putting your fingers in the mouth, and having direct contact with someone that is infected with norovirus.
If you get norovirus illness, you can shed billions of norovirus particles that you can’t see without a microscope. Only a few norovirus particles can make other people sick. You are most contagious:
- When you have symptoms of norovirus illness, especially vomiting, and
- During the first few days after you recover from norovirus illness
However, studies have shown that you can still spread norovirus for two weeks or more after you feel better.
Pertussis
Pertussis is a vaccine preventable respiratory illness commonly known as whooping cough. It is a very contagious disease caused by a type of bacteria called Bordetella pertussis. These bacteria attach to the cilia (tiny, hair-like extensions) that line part of the upper respiratory system. The bacteria release toxins (poisons), which damage the cilia and cause airways to swell.
It can cause serious illness in babies, children, teens, and adults. Symptoms of pertussis usually develop within 5 to 10 days after you are exposed. Sometimes pertussis symptoms do not develop for as long as 3 weeks.
The disease usually starts with cold-like symptoms and maybe a mild cough or fever. In babies, the cough can be minimal or not even there. Babies may have a symptom known as “apnea.” Apnea is a pause in the child’s breathing pattern. Pertussis is most dangerous for babies. About half of babies younger than 1 year who get the disease need care in the hospital.
Early symptoms can last for 1 to 2 weeks and usually include:
- Runny nose
- Low-grade fever (generally minimal throughout the course of the disease)
- Mild, occasional cough
- Apnea – a pause in breathing (in babies)
Pertussis in its early stages appears to be nothing more than the common cold. Therefore, healthcare professionals often do not suspect or diagnose it until the more severe symptoms appear.
After 1 to 2 weeks and as the disease progresses, the traditional symptoms of pertussis may appear and include:
- Paroxysms (fits) of many, rapid coughs followed by a high-pitched “whoop” sound (babies with pertussis may not cough at all)
- Vomiting (throwing up) during or after coughing fits
- Exhaustion (very tired) after coughing fits


Pertussis can cause violent and rapid coughing, over and over, until the air is gone from your lungs. When there is no more air in the lungs, you are forced to inhale with a loud “whooping” sound. This extreme coughing can cause you to throw up and be very tired. Although you are often exhausted after a coughing fit, you usually appear well in-between. Coughing fits generally become more common and bad as the illness continues and can occur more often at night. The coughing fits can go on for up to 10 weeks or more.
Recovery from pertussis can happen slowly. The cough becomes milder and less common. However, coughing fits can return with other respiratory infections for many months after the pertussis infection started.
Pinworms
A pinworm (“threadworm”) is a small, thin, white roundworm (nematode) called Enterobius vermicularis that sometimes lives in the colon and rectum of humans. Pinworms are about the length of a staple. While an infected person sleeps, female pinworms leave the intestine through the anus and deposit their eggs on the surrounding skin.

Pinworm infection (called enterobiasis or oxyuriasis) causes itching around the anus which can lead to difficulty sleeping and restlessness. Symptoms are caused by the female pinworm laying her eggs. Symptoms of pinworm infection usually are mild, and some infected people have no symptoms.
Pinworm infection often occurs in more than one person in household and institutional settings. Childcare centers often are the site of cases of pinworm infection.
People become infected, usually unknowingly, by swallowing (ingesting) infective pinworm eggs that are on fingers, under fingernails, or on clothing, bedding, and other contaminated objects and surfaces. Because of their small size, pinworm eggs sometimes can become airborne and ingested while breathing.
RSV
Respiratory syncytial (sin-SISH-uhl) virus, or RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious, especially for infants and older adults. In fact, RSV is the most common cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia (infection of the lungs) in children younger than 1 year of age in the United States. It is also a significant cause of respiratory illness in older adults.
Symptoms of RSV infection usually include:
- Runny nose
- Decrease in appetite
- Coughing
- Sneezing
- Fever
- Wheezing
These symptoms usually appear in stages and not all at once. In very young infants with RSV, the only symptoms may be irritability, decreased activity, and breathing difficulties.

RSV can also cause more severe infections such as bronchiolitis, an inflammation of the small airways in the lung, and pneumonia, an infection of the lungs. It is the most common cause of bronchiolitis and pneumonia in children younger than 1 year of age. Almost all children will have had an RSV infection by their second birthday. People infected with RSV usually show symptoms within 4 to 6 days after getting infected. Most RSV infections go away on their own in a week or two.
RSV can spread when an infected person coughs or sneezes. You can get infected if you get droplets from the cough or sneeze in your eyes, nose, or mouth, or if you touch a surface that has the virus on it, like a doorknob, and then touch your face before washing your hands. Additionally, it can spread through direct contact with the virus, like kissing the face of a child with RSV.
People infected with RSV are usually contagious for 3 to 8 days. However, some infants, and people with weakened immune systems, can continue to spread the virus even after they stop showing symptoms, for as long as 4 weeks. Children are often exposed to and infected with RSV outside the home, such as in school or child-care centers. They can then transmit the virus to other members of the family.
RSV can survive for many hours on hard surfaces such as tables and crib rails. It typically lives on soft surfaces such as tissues and hands for shorter amounts of time. Frequently, a child is infectious before symptoms appear.
Ringworm
Ringworm is a common skin infection that is caused by a fungus. It’s called “ringworm” because it can cause a circular rash (shaped like a ring) that is usually red and itchy. Anyone can get ringworm. The fungi that cause this infection can live on skin, surfaces, and on household items such as clothing, towels, and bedding.
Ringworm goes by many names. The medical terms are “tinea” or “dermatophytosis.” Other names for ringworm are based on its location on the body – for example, ringworm on the feet is also called “athlete’s foot.”

Ringworm can affect skin on almost any part of the body as well as fingernails and toenails. The symptoms of ringworm often depend on which part of the body is infected, but they generally include:
- Itchy skin
- Ring-shaped rash
- Red, scaly, cracked skin
- Hair loss
Symptoms typically appear between 4 and 14 days after the skin comes in contact with the fungi that cause ringworm. The fungi that cause ringworm can live on skin and in the environment.
There are three main ways that ringworm can spread:
- From a person who has ringworm
- From an animal that has ringworm.
- From the environment.
Roseola
Roseola is a viral infection that commonly affects infants and young children. It involves a pinkish-red skin rash and high fever. Roseola is common in children ages 3 months to 4 years, and most common in those ages 6 months to 1 year. It is caused by a virus called human herpesvirus 6 (HHV-6), although similar syndromes are possible with other viruses. The time between becoming infected and the beginning of symptoms (incubation period) is 5 to 15 days.
The first symptoms include:
- Eye redness
- Irritability
- Runny nose
- Sore throat
- High fever, that comes on quickly and may be as high as 105°F (40.5°C) and can last 3 to 7 days
About 2 to 4 days after becoming sick, the child’s fever lowers, and a rash appears. This rash most often:
- Starts on the middle of the body and spreads to the arms, legs, neck, and face
- Is pink or rose-colored
- Has small sores that are slightly raised
The rash lasts from a few hours to 2 to 3 days. It usually does not itch.
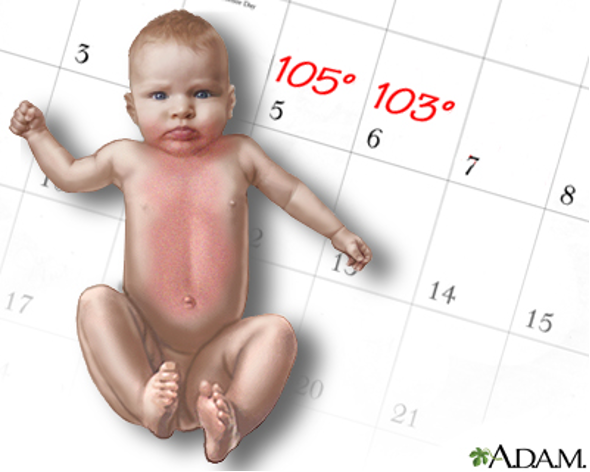
There is no specific treatment for roseola. The disease most often gets better on its own without complications.
Rotavirus
Rotavirus is most common in your infants and young children. Children, even those who are vaccinated, may get infected and sick from rotavirus more than once. That is because neither natural infection with rotavirus nor vaccination provides full protection from future infections. Children who are not vaccinated usually have more severe symptoms the first time they get rotavirus disease. Vaccinated children are less likely to get sick from rotavirus.
Symptoms usually start about 2 days after a person is exposed to rotavirus. Vomiting and watery diarrhea can last 3 to 8 days. Additional symptoms may include loss of appetite and dehydration (loss of body fluids), which can be especially dangerous for infants and young children.
Symptoms of dehydration include:
- Decreased urination
- Dry mouth and throat
- Feeling dizzy when standing up
- Crying with few or no tears and
- Unusual sleepiness or fussiness.
People who are infected with rotavirus shed the virus in their stool (poop). This is how the virus gets into the environment and can infect other people (through contaminated food, surfaces, or unwashed hands). People shed rotavirus the most, and are more likely to infect others, when they have symptoms and during the first 3 days after they recover. People with rotavirus can also infect others before they have symptoms.
Rubella (German Measles)
Rubella is a vaccine preventable disease that is also called German measles, but it is caused by a different virus than measles. It is usually mild with fever and a rash. About half of the people who get rubella do not have symptoms. If you do get them, symptoms may include:
- A rash that starts on the face and spreads to the body
- Mild fever
- Aching joints, especially in young women
- Swollen glands

Rubella spreads when an infected person coughs or sneezes. People without symptoms can still spread it. There is no treatment, but the measles-mumps-rubella (MMR) vaccine can prevent it.
Shigella
Shigellosis is a very contagious diarrheal disease caused by bacteria called Shigella. Shigella causes about 500,000 cases of diarrhea in the United States annually.
Symptoms of the Shigella infection typically start one to two days after exposure and include:
- Diarrhea (watery and often bloody)
- Fever
- Abdominal pain, cramps, vomiting
- A painful sensation of needing to pass stools even when bowels are empty
Shigella spreads when people put something in their mouths or swallow something that has come into contact with stool of a person infected with Shigella.
Tuberculosis
Tuberculosis (TB) is a contagious disease, caused by the bacteria Mycobacterium tuberculosis. The bacteria usually attack the lungs but can attack any organ in the body. Recommended treatment depends on whether a person has:
- Latent TB infection–has no symptoms and can’t spread the TB bacteria to others; has potential to develop active TB disease if not treated
- Active TB disease–has symptoms such as a fever, cough, or weight loss; these persons may be able to spread the germ to others. Needs treatment to cure the disease.
TB is spread in the air when a person with active TB disease of the lung or throat coughs, sneezes, or speaks. The germs can be inhaled by someone else, and they can become infected. TB is often spread between people who spend time together every day. TB in children usually comes from being around adults with active TB disease.
Appendix B: Sample Exclusion Guidelines |