Module 7.2 Creating Safe Indoor Environments
Learning Objectives
By the end of this module, you should be able to:
- Connect classroom design to safety and injury prevention.
- Discuss ways to handle unsafe behavior by understanding the function of behaviours.
- Describe how teachers can ensure the toys and materials they offer children do not present injury risks and are nontoxic.
- List ways to protect children from choking, poisoning, burns, drowning and falls.
- Identify how to implement safe sleep practices to protect against Sudden Infant Death Syndrome.
Introduction
Designing an effective and engaging early learning environment takes careful thought and planning, but it’s important. A well-organized learning environment that is interesting, orderly, and attractive contributes to children’s participation and engagement with the learning materials and experiences. This engagement, in turn, contributes to children’s learning.
Let’s look at it from a child’s perspective. We want children to feel safe and comfortable in the learning environment. We want them to be interested in the learning experiences and to take full advantage of the experiences you’ve planned and the materials you’ve selected. It can be helpful to get down at a child’s level and look at the environment. Does it feel welcoming and inviting? Is there enough room to move, make choices, and stay involved with a toy, experience, or project? And does the room help the child know what to do and what’s expected?

Designing an Effective and Safe Learning Environment
There are all sorts of learning environments. They differ by size and shape, amount of light and wall space, placement of sinks and counters, and amount of storage. Figuring out how to design the physical space and to maximize children’s interactions within the space will take some time. Make a floor plan. Move things around. Look at other learning environments and see what works.
Here are a few things to think about when designing your space and making it as workable as possible. Think about the number of interest areas or centers that you want or need for the group of children. Arrange the space so that noisy areas are separated from quiet areas. Locate centers next to needed storage or equipment. Use furniture or other items to provide boundaries. But make sure that the educators can see all the areas of the room.
Factors to Consider
Space and boundaries
- Are the centres clearly defined with furniture, rugs, or shelves?
- Is there enough space for all children to easily move about the room?
- In each defined area, is there adequate space for the number of children using it?
Proximity and distance
- Are the quiet and noisy areas in proximity or separated?
- Are centers located near things that children need to complete projects (art center near sink, puzzle, or game shelves within reach of tables, etc.)?
- Are educators able to view children in all centers?
Home and culture
- What home-like features are included in the environment?
- How is(are) the culture(s) of the local community reflected in the environment?
Flexibility and permanence
- How does the space accommodate gross motor experiences?
- What aspects of the physical space cannot be changed (cost or structural issues) and are challenging to overcome (e.g., limited access to natural light, cumbersome cubbies, etc.)?
Engagement and challenging behaviours
- Are there areas of the environment where challenging behaviours are more likely to occur?
- Are there areas where typically children are positively engaged in learning experiences?
Traffic patterns
- Can children move easily from space to space?
- Is running and aimless wandering discouraged?
Material selection
- Are materials chosen to support development and learning?
- Are they culturally relevant and meaningful to the children?
- Is there is a sufficient variety and quantity (without overwhelming children)?
Pause to Reflect 💭
So far, we haven’t specifically called out safety much in our discussion of environmental design. Look at some of the listed items and brainstorm how they each might be related to safety.
For example, why is looking at areas of the environment where challenging behaviours are more likely to occur a safety consideration?
Tips for Environmental Design
- Traffic patterns need to discourage running.
- Use furniture, rugs, and similar items to define boundaries.
- Ensure that educators can see what is happening in all areas of the classroom.
- Cultural and home-like features are present in the room.
- Use spaces with as much flexibility as possible.
- Quiet and noisy centers are spaced appropriately.
- Ensure interesting classroom content selection is balanced with appropriate stimulation versus overstimulation.
- Each centre provides enough information about what to do there and how to play.

Grouping of Children
Educators want to be intentional about how they group children, whether it’s a decision made in the moment or as part of experience planning. Match the size of the group with the purpose of the experience. Think about the children who will be in the group. Young children need opportunities to participate and learn with the whole group, small groups, and they will thrive with a bit of one-on-one time with an adult.
Large groups are good for:
- Introducing concepts
- Building community
- Conducting routine activities
Small groups are good for:
- Maximizing back and forth interactions
- Peer modeling of skills
- Guiding instruction
One-on-one educator/child interactions are good for:
- Tasks requiring complex skills
- Instance when a child needs specific direction and assistance
Pause to Reflect 💭
How is considering group size related to safety? What might educators need to observe for to determine if the group sizes are working well for the children?
Every learning environment is full of pros and cons; it is how educators work with the many characteristics of an environment that can make a tremendous difference. Educators can be surprised by the results when they:
- Assess the spaces for both limitations and strengths.
- Strategize how to optimize what they have to work with in their environments.
- Try a different arrangement, see what happens, and then modify based on what is working and what is not.
Sometimes a modification can be minor (raising or lowering a shelf, “stop” signs over unavailable areas, masking tape to better define a space, etc.). This highlights the “work-in-progress” nature of learning environments. As the needs of children change, the environment may need minor changes or must be rearranged completely to meet those needs.
A Few More Considerations for Environmental Design
When designing learning environments, there are some other considerations to keep in mind:
- Avoid grouping the same children together all the time, especially when pairing skilled with less skilled children.
- Consider limiting the number of children per center and creating a system for rotating children through favourite areas.
- Regularly rotate some of the toys and materials to generate a sense of newness.
- Instruction can be tailored within small groups to meet educational goals. For example, one group of children that is working on learning numbers can read a counting book; another group working on fine motor skills can do beading; still another group of children working on social skills can practice joining play.
- Emphasize cooperation by choosing toys and experiences that require it (e.g., large appliance boxes, games that need two or more players, balls for throwing back and forth, etc.).
- Whenever possible keep the design elements simple (both for the educator’s sake and because simple tends to be longer-lasting). Also, some aspects of designing can be done spontaneously and quickly (spur of the moment) and still be effective.
Interpersonal Safety
Children can behave in ways that hurt themselves or others so educators must prepare to handle unsafe behaviors in their duty to protect children from injury. An important way to think about behaviour is as a form of communication. Young children let us know their wants and needs through their behavior long before they have or can use words in the heat of the moment. They give us cues to help us understand what they are trying to communicate.
Educators can help children by interpreting their cues and responding to meet their needs. The following example illustrates the importance of responding to the possible meaning behind behaviour:
Javon bites Blair because he wants the block she is playing with, and we remove Javon from the situation. Not only are we not responding to his want or need, but we are taking him out of the context where he can learn to communicate his feelings in a way that doesn’t hurt others.
Forms and Functions of Behaviour
There are many reasons a child might use specific behaviours. This is why it is important for educators to carefully observe children, pay attention to their cues, get to know them, and know what part of the schedule gives them a challenging time to better understand what they are trying to tell us through their behaviour. Each behaviour has a form (the behaviour the child is using to communicate) and a function (the reason or purpose the child is using that behaviour).
Forms of Communication
- Crying
- Cooing
- Reaching for caregiver
- Kicking their legs
- Gaze aversion (looking away)
- Squealing
- Biting
- Tantrums
- Pointing
- Smiling
- Pulling the caregiver
- Clapping
- Words
- Jumping
Functions of Communication
- Obtain an object, activity, person
- Request help
- Initiate social interaction
- Request information
- Seek sensory stimulation
- Escape demands
- Escape activity
- Avoid a person
- Escape sensory stimulation
- Express emotion
- Express pain or illness
Here are some examples of communication forms and functions of toddlers and preschoolers:
Table 1 – Examples of Forms and Possible Functions of Behaviours
|
Form of Communication |
Possible Functions of Communication |
| Toddler biting |
|
| Preschooler hitting |
|
Form and function are also shaped by culture. Children are socialized to express their feelings in culturally acceptable ways. It is important to talk with families so you can look for acceptable ways that children express themselves in a culturally respectful way.
As you have probably already experienced—it is not always easy to figure out the meaning of a child’s behaviour. To add to the complexity of understanding the meaning of behaviour:
- A single form of behaviour may serve more than one function. For example, a toddler might use biting (form) for different functions (“I want the toy you have.” “I want to play with you but don’t know how to let you know.” “I’m tired.” “I’m frustrated because you don’t understand what I am trying to tell you.” “I want some attention.”)
- Several forms of behaviour may serve one function. For example, a child’s purpose (function) may be to build with their favourite blocks, but they use different forms of behaviour (biting, yelling, grabbing, running away with the blocks, sharing) based on how they feel that day, who is playing in the block area, or based on their cultural expectations.
- The meaning of behaviour is shaped by culture, family, and the unique makeup and experiences of the individual child. For example, some cultures may express sadness by crying or by having a nonchalant facial expression. Some cultures may express happiness by laughing and being exuberant, while others may expect more restrained behaviours.
Some of these functions of communication become a concern for children’s safety (of the child communicating, the other children, and other people in the environment). Educators must take the time to understand a behaviour’s meaning so that they can help the child replace unsafe forms of communication with forms that don’t hurt others or harm the environment. Pausing to try to figure out the meaning behind a child’s behaviour—instead of just reacting to the behaviour—can change the way we see a child, the way we respond to a child, and the way we teach a child. Becoming a “behaviour has meaning” detective who is always on the lookout for the meaning of behaviour will help you keep children safe. Look at the following example of an unsafe behaviour, what it might mean, and what an educator might do to support the child.
Educator Emilia and Sarae
Educator Emilia says about a child Sarae, “I have to watch her like a hawk, or she’ll run down the hall or go out the gate, down the street, and I don’t know where.”
- What this might mean: We could reframe this to “Sarae is an active child. They may naturally be kinesthetic learner, who needs to move and shake, and have extra energy.”
- What the Educator might do: Emilia can give Sarae positive ways to exercise the way she loves. For example, when they are outdoors, the educator can set up an obstacle course or create opportunities for running with intention, such as part of a game with their peers. If it’s hard to get them back inside, give them a leadership role. Maybe they are the one who has the bell that cues everybody that it’s time to line up. So now they are going to make sure they find their friends and are the one responsible for bringing the whole group together to go inside.
- The potential result: Reframing the behavior and providing positive outlets will not only keep Sarae safe, but it will also communicate to them that how they feel is okay and that they are being supported, acknowledged, and encouraged.

Taking a Closer Look at Behaviour
You may also find it valuable to examine behaviour much the way you would injuries and traffic patterns. Gather data about unsafe behaviours:
- When are they happening?
- Are there specific times of day that children are finding more challenging to behave/communicate in safe ways?
- Where are they happening?
- Are there hot spots for challenging behaviour? What in the environment might be the focus of the unsafe behaviour/communication?
- Why are they happening?
- What happened before the led up to the behaviour? What happened after?
- Who are the behaviours happening between?
- All children will have times where they communicate with unsafe behavior, but some children may need more adult support in certain contexts (time of day, activity, groupings of children, etc.).
Look for patterns. Reflect on what can be changed in the physical environment, schedule/routine, groupings, and supervision to help prevent children from hurting themselves or others when trying to communicate their needs.
Biting
Biting is a common but upsetting behaviour of toddlers. Here is some information and tips for responding to biting.
When a child bites another child:
- Intervene immediately between the child who bit and the bitten child. Stay calm and don’t overreact, yell, or give a lengthy explanation.
- Use your voice and expression to show that biting is not acceptable.Look into the child’s eyes and say calmly but firmly, “I do not like it when you bite people.” For a child with more limited language, just say “No biting people.” Point out how the biter’s behavior affected the other person. “You hurt him and he’s crying.” Encourage the child who was bitten to tell the biter “You hurt me.” Encourage the child who bit to help the other child by getting the ice pack, etc.
- Offer the bitten child comfort and first aid.Wash broken skin with warm water and soap. Observe universal precautions if there is bleeding. Apply an ice pack or cool cloth to help prevent swelling. Inform both families of what happened. Suggest the bitten child be seen by a health care provider if the skin is broken or there are any signs of infection (redness or swelling).
Preventing biting
- Reinforce desired behaviour. Notice and acknowledge when you like what a child is doing, especially for showing empathy or social behavior, such as patting a crying child, offering to take turns with a toy or hugging gently.
- Do not label, humiliate, or isolate a child who bites.
- Discourage play which involves “pretend” biting or seems too rough and out of control.
- Help the child learn how to make more appropriate connections with others.
Why do children bite and what can we do?
Children bite for many different reasons, so to respond effectively, it’s best to try and find out why they are biting. If a child:
- Experiments by biting immediately say “no” in a firm voice, and give them a variety of toys to touch, smell and taste and encourage sensory-motor exploration.
- Has teething discomfort, provide cold teething toys or safe, chewy foods.
- Is becoming independent, provide opportunities to make developmentally appropriate choices and have some control (the bread or the cracker, the yellow or the blue ball), and notice and give positive attention as new self-help skills and independence develop.
- Is using muscles in new ways, provide a variety of play materials (hard/soft, rough/smooth, heavy/light) and plan for plenty of active play indoors and outdoors.
- Is learning to play with other children, try to guide behavior if it seems rough (take the child’s hand and say, “Touch Jorge gently—they like that”) and reinforce prosocial behavior (such as taking turns with toys or patting a crying child).
- Is frustrated in expressing their needs and wants, state what they are trying to communicate (“you feel mad when Ari takes your truck” or “you want me to pay attention to you”).
- Is threatened by new or changing situations such as a parent returning to work, a new baby, or parents/caregivers separating, provide special nurturing and be as warm and reassuring as possible, and help them talk about feelings even when they say things like “I hate my new baby.”
Safe Toys, Materials, and Equipment
Play is a natural activity for every young child. Play provides many opportunities for children to learn and grow – physically, mentally, and socially. If play is the child’s work, then the toys, materials, and equipment in the environment are what will enable children to do their work well and safely.
Safe Toys
Protecting children from unsafe toys is the responsibility of everyone. Careful toy selection and proper supervision of children at play are still—and always will be—the best ways to protect children from toy-related injuries.
It is important that educators consider both safety and durability when choosing toys for children. Toys should be constructed to withstand the uses and abuses of children in the age range for which the toy is appropriate.
All toys must be checked periodically for breakage and potential hazards. A damaged or dangerous toy should be thrown away or repaired immediately.
In Canada, toy safety standards are created and enforced by Health Canada. The relevant legislation is the Canada Consumer Product Safety Act. Toy Regulations fall under this Act. “Toy” is defined as “a product that is intended for use by a child under 14 years of age in learning or play.” (Government of Canada, 2021)
Specific products covered by the Toy Regulations include dolls/plush toys/ soft toys, pull/push toys, toy steam engines, finger paints, rattles, elastics, yo-yo type balls and magnetic toys. The Toy Regulations also govern packaging, electrical hazards, mechanical hazards, auditory hazards, thermal/flammability hazards, and toxicological hazards.
Under the Toy Regulations, there is no mandatory requirement to test toys before putting a toy on the market or obtain authorization to market a toy. Also, there are no reporting requirements. The Canada Consumer Product Safety Act includes incident reporting requirements.
Age-Appropriate Toys
Educators must keep in mind the ages of children they are choosing toys for, including their typical interests and skill levels. The manufacturer’s age recommendation is a good starting place to ensure that toys are age appropriate. Warnings such as “Not recommended for children under 3” should be followed. See Table 2 for some age-appropriate toys to consider. Please note that toys appear on the list when they become appropriate and are not repeated in later ages.
Table 2 – Age-Appropriate Toys
|
Age |
Some Age-Appropriate Toys |
|
| From 6 weeks to around 4 months these toys become appropriate |
|
|
| Between 4 to 6 months these toys become appropriate |
|
|
| Between 7 to 12 months these toys become appropriate |
|
|
| These toys become appropriate for 1-year-olds | In addition to above:
|
|
| These toys become appropriate for 2-year-olds |
|
|
| These toys become appropriate at around 3 years of age |
|
|
| These toys become appropriate around 4 years of age |
|
|
| These toys become appropriate around 5 years of age |
|
|
Nontoxic Art Materials
According to the Government of Canada’s publication Information for Art Class Teachers: Chemical Safety (2012) “The Art and Creative Materials Institute (ACMI) is an independent U.S. association that provides seals on products they have evaluated and tested, taking into account how the product is used as well as its chemical content. So, when you see the seal, you know it has been evaluated and tested for both acute and chronic potential hazards.
The Art and Creative Materials Institute (ACMI) maintains that the “knowledge of materials and their proper use makes them safe. Be sure to read the label on all products you use so you will know they have been evaluated and are non-toxic or need special handling to avoid possible health potential hazards from misuse.”
Although it is not a legal requirement in Canada, many art materials you buy will have one of the following ACMI labels on them:
- According to the ACMI, the AP (Approved Product) seal “identifies art materials that are safe and that are certified in a toxicological evaluation by a medical expert to contain no materials in sufficient quantities to be toxic or injurious to humans, including children, or to cause acute or chronic health problems.”
- According to the ACMI, the CL (Caution Required) seal “identifies products that are certified to be properly labelled in a program of toxicological evaluation by a medical expert for any known health risks and with information on the safe and proper use of these materials.”
On the label, you may also see Conforms to ASTM D 4236. This does not mean the product is “non-toxic.” It means that the product has been reviewed by a qualified toxicologist, that the label lists all the ingredients that are potential acute or chronic hazards, and if the product does contain a substance with an acute or chronic hazard, it comes with instructions for using it safely.” (Government of Canada, 2012)
Safety Risks from Art Materials
For certain chemicals and exposure situations, children may be especially susceptible to the risk of injury. For example, since children are smaller than adults, children’s exposures to the same amount of a chemical may result in more severe effects. Further, children’s developing bodies, including their brains, nervous systems, and lungs may make them more susceptible than adults. Differences in metabolism may also affect children’s responses to some chemicals.
Children ‘s behaviours and cognitive abilities may also influence their risk. For example, children under the age of 12 are less able to remember and follow complex steps for safety procedures, and are more impulsive, making them more likely to ignore safety precautions. Children have a much higher chance of toxic exposure than adults because they are unaware of the dangers, not as concerned with cleanliness and safety precautions as adults and are often more curious and attracted to novel smells, sights, or sounds. Children need regular and consistent reminders of safety rules, and there is no substitute for direct supervision.
Guidelines for Selecting Art and Craft Materials
Here are some helpful reminders about choosing art materials for children:
- Note that even products labeled ‘non-toxic’ when used in an unintended manner can have harmful effects.
- Products with cautionary/warning labels should not be used with children under age 12.
- Avoid solvents and solvent-based supplies, which include turpentine, paint thinner, shellac, and some glues, inks, and a few solvent-containing permanent markers.
- Avoid products or processes that produce airborne dust that can be inhaled (including powdered tempera paint).
- Avoid old supplies, unlabeled supplies, and be wary of donated supplies with cautionary/warning labels.
- Look for products that are clearly labeled with information about intended uses.
- Give special attention to students with asthma or allergies, which may elevate the students’ sensitivities to fumes, dust, or products that come into contact with the skin.
- Gather your supplies beforehand so that you can continue to supervise their use without needing to step away.
- Instruct children on safety practices before you begin (such as, modeling how to cut safely with scissors).
- Do activities in well-ventilated areas.
- Use protective equipment (such as smocks).
- Assume that anything you use should be safe enough that it won’t harm children if it gets on their skin or in their mouths and/or eyes.
Preventing Injuries Indoors
Some injuries that educators should be aware of and intentionally act to prevent were discussed in previous modules. Here is some further information about injuries that are more likely to happen indoors.
Choking
Choking occurs when an object blocks the airway, preventing breathing. According to Cyr:
- “Choking and suffocation are responsible for almost 40% of unintentional injuries in infants under the age of one in Canada.
- For every choking-related death, there are an estimated 110 children treated in hospital emergency departments.
- The number of children receiving first aid or outpatient assessment for significant choking incidents in the community is unknown.” (Cyr, 2020)
Reducing the Risk of Choking
The main way to prevent choking is to recognize that objects that are 1½ inches or less in diameter are higher risk. Foods are the most common cause of choking. Having children sit during snacks and meals at an unhurried pace, allowing time for children to properly chew their food helps prevent choking on food. Food is safest when cut into small pieces or served in small amounts.
Common Choking Hazards
|
Foods |
Other Items |
|
|
Toys, and other items that children may play with, are another common source of choking hazards. Ensuring children only have access to age-appropriate toys is an important step.
Educators can use a small parts tester, a commercial product commonly known as a choke tube, to test whether an object is a choking hazard. Recognizing and responding to choking will be addressed in Module 7.4.


Poisoning
There are many hazards that put children at risk for accidental poisoning, both indoors and outdoors. Poisoning can occur at any time a harmful substance is intentionally or unintentionally ingested. Poisons come in many forms including plants, cleaning supplies, spoiled food, and medications. Children, who are naturally curious and like to explore, are in particular at risk for poisoning.
Guidelines to Prevent Poisoning
- Keep all cleaning supplies and chemicals locked.
- All medications must be kept in a locked storage area, out of reach.
- Check medications periodically for expiration dates and properly dispose of expired medications. Some medications become toxic when they are past their expiration date.
- Do not tell children that medication is “candy” as this makes it look more attractive to them.
- Ensure all medications and chemicals are properly labeled. Childproof caps should be on medicine bottles.
- Use safe food practices. (Previously covered in Module 5.4)
- Never use cans that have bulges or deep dents in them.
- Keep poisonous plants out of reach of children (see Table 3)
- Keep the number for Poison Control near a telephone.
Table 3 – Poisonous Plants
|
Common Name |
Botanical Name |
| Azalea, rhododendron | Rhododendron |
| Caladium | Caladium |
| Castor bean | Ricinis communis |
| Daffodil | Narcissus |
| Deadly nightshade | Atropa belladonna |
| Dumbcane | Dieffenbachia |
| Elephant Ear | Colocasia esculenta |
| Foxglove | Digitalis purpurea |
| Fruit pits and seeds | contain cyanogenic glycosides |
| Holly | Ilex |
| Iris | Iris |
| Jerusalem cherry | Solanum pseudocapsicum |
| Jimson weed | Datura stramonium |
| Lantana | Lantana camara |
| Lily-of-the-valley | Convalleria majalis |
| Mayapple | Podophyllum peltatum |
| Mistletoe | Viscum album |
| Morning glory | Ipomoea |
| Mountain laurel | Kalmia iatifolia |
| Nightshade | Salanum spp. |
| Oleander | Nerium oleander |
| Peace lily | Spathiphyllum |
| Philodendron | Philodendron |
| Pokeweed | Phytolacca americana |
| Pothos | Epipremnum aureum |
| Yew | Taxus |
Burns
Younger children are more likely to sustain injuries from scald burns that are caused by hot liquids or steam, while older children are more likely to sustain injuries from flame burns that are caused by direct contact with fire.
Causes of Burns
Burns can be caused by dry or wet heat, chemicals, or electricity (both indoors and outdoors).
- Burns from dry heat can occur from fire, irons, hairdryers, curling irons, and stoves.
- Burns from wet or moist heat occur from hot liquids, such as hot water or steam. These types of burns are called scalds. Scalds can occur within seconds and cause serious injury.
- Chemical burns occur from chemical sources and can also cause serious burns when exposed to skin, or if swallowed, whether intentionally or unintentionally.
- Electrical burns can cause very serious injury as they can burn both the outside and inside of the person’s body, causing injury that cannot be seen, and which can be life-threatening.
- Radiation burns can also occur from sources of radiation such as sunlight.
Types of Burns
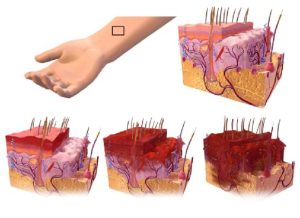
Burns are divided into first-, second-, and third-degree burns.
First degree burns affect only the outer layer of the skin (epidermis). These types of burns are the least serious as they are only on the surface of the skin. First degree burns usually appear red, dry, and slightly swollen. Blisters do not occur with this type of burn. They should heal within a couple of days. A first-degree burn is pictured in the bottom left of Figure 7.
Second degree burns affect the top layer of the skin and the second layer of skin underneath (dermis). These are more serious than first degree burns. The skin may appear very swollen, red, moist, and may have blisters or look watery and weepy. A second-degree burn is pictured in the bottom middle of Figure 7.
Third degree burns are the most serious burn. A third-degree burn affects all layers of the skin and may affect the organs below the surface of the skin. The skin may appear white or black and charred. The person may deny pain because the nerve endings in their skin have been burned away. Third degree burns require immediate medical treatment. If adults suspect a child has a third-degree burn, they should immediately call 911. A third-degree burn is pictured in the bottom right of Figure 7.
Chemical burns can occur anytime a liquid or powder chemical comes into contact with skin or mucous membranes that line the eyes, nose, or throat. Chemical burns may also occur if a chemical is swallowed. These burns can cause serious injury and emergency services should be contacted. If a person receives a chemical burn, the chemical should be removed from the skin by using a gloved hand to brush it off and then wash the area with plenty of cool water. Electrical burns can occur if a person has been using an electrical appliance and is exposed to water or if an electrical short occurs while using the electrical appliance. Using faulty or frayed cords on electrical appliances can result in electrical burns. Electrical burns are a serious injury. Emergency medical services (EMS) should be immediately activated.
Never use oils such as butter or vegetable oil on any type of burn as this can cause further injury. For first or second degree burns flush the area with plenty of cool (not ice cold) water for about 15 minutes or until the pain decreases and cover with a clean, dry bandage. Using ice or ice-cold water can cause frostbite. For major burns remove any clothing that is not stuck to the skin, cover the burned area with a dry, clean cloth, and seek emergency assistance.
Guidelines to Prevent Burns
- Install and regularly test smoke alarms.
- Practice fire drills.
- Train staff to use fire extinguishers.
- Teach children to stop, drop, and roll.
- Never allow children to use electrical appliances unsupervised.
- Never use electrical appliances near water sources.
- Never use electrical appliances in which the cord appears to be damaged or frayed.
- Never pull a plug from the cord. Always remove a cord from an outlet by holding the base of the plug.
- Cover electrical outlets with childproof plugs. Never allow children to put anything inside an electrical outlet.
- Ensure stoves and other appliances are turned off when finished with them.
- Turn pot handles inward so that a person cannot accidentally bump a handle and spill hot liquids.
- Do not use space heaters and other personal heaters.
- Check to be sure the hot water heater is not set too high. To avoid scalds from hot tap water, hot water heaters should be set to 120 degrees or less.
- Keep chemicals, cleaning solutions, and matches and lighters securely locked and out of reach of children.
Safe Sleeping
Sudden Infant Death Syndrome (SIDS) is identified when the death of a healthy infant occurs suddenly and unexpectedly, and medical and forensic investigation findings (including an autopsy) are inconclusive. In Canada, SIDS takes the life of 1 of every 2,000 live-born babies. Babies of aboriginal background are at greater risk of SIDS. It is estimated that three babies die of SIDS every week in Canada. (Baby’s Breath Canada, 2016)
Because SIDS is diagnosed when no other cause of death can be determined, possible causes of SIDS are regularly researched.
This is a very important topic for educators as one study found that while data suggests that only 7% of incidents of SIDS should occur while children are in childcare, 20.4% actually did. (Moon et al, 2000)

Risk Factors for SIDS
Babies are at higher risk for SIDS if they:
- Sleep on their stomachs
- Sleep on soft surfaces, such as an adult mattress, couch, or chair or under soft coverings
- Sleep on or under soft or loose bedding
- Get too hot during sleep
- Are exposed to cigarette smoke in the womb or in their environment, such as at home, in the car, in the bedroom, or other areas
- Sleep in an adult bed with parents/caregivers, other children, or pets; this situation is especially dangerous if:
- The adult smokes, has recently had alcohol, or is tired.
- The baby is covered by a blanket or quilt.
- The baby sleeps with more than one bed-sharer.
- The baby is younger than 11 to 14 weeks of age.
Important Facts About SIDS
- SIDS happens in families of all social, economic, and ethnic groups.
- Most SIDS deaths occur between one and four months of age.
- SIDS occurs in boys more than girls.
- The death is sudden and unexpected, often occurring during sleep. In most cases, the baby seems healthy.
- Although it is not known exactly what causes SIDS, researchers know that it is not caused by suffocation, choking, spitting up, vomiting, or immunizations.
- SIDS is not contagious.
Reducing the Risks Associated with SIDS
Although the sudden and unexpected death of an infant cannot be predicted or prevented, research shows that certain infant care practices can help reduce the risk of a baby dying suddenly and unexpectedly. Educators can help lower the risk of SIDS for infants less than one year of age by following these risk reduction guidelines.
Sleeping Position
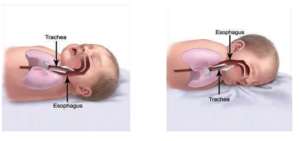
The chance of an infant dying suddenly and unexpectedly in childcare is higher when a baby first starts the transition from home to care. Research shows if a baby has been placed on his/her back by the families, and the childcare provider places the baby to sleep on his/her stomach, there is a higher risk of death in the first weeks of childcare. One of the most important things you can do to reduce the risk of sudden unexpected death is to place babies to sleep on their backs.
Healthy babies do not choke when placed to sleep on their backs. By reflex, babies swallow or cough up fluids to keep the airway clear. Since the windpipe (trachea) is positioned on top of the esophagus, fluids are not likely to enter the airway. (See Figure 9)
Babies who can roll back and forth between their back and tummy should be placed on their backs for sleep and allowed to assume their sleep position of choice. When infants fall asleep while playing on their tummies, move the baby to a crib onto his/her back to continue sleeping.
The Public Health Agency of Canada, in co-operation with the Canadian Paediatric Society, the Canadian Foundation for the Study of Infant Deaths, the Canadian Institute of Child Health and Health Canada, has developed A Joint Statement on Safe Sleep: Preventing Sudden Infant Deaths in Canada. Input was also received from provincial/territorial, national, and regional public health stakeholders.
The Joint Statement identifies the principles of safe sleep and risk factors that are modifiable.
- Infants placed on their backs to sleep, for every sleep, have a reduced risk of SIDS.
- Preventing exposure to tobacco smoke, before and after birth, reduces the risk of SIDS.
- The safest place for an infant to sleep is in a crib, cradle, or bassinet that meets current Canadian regulations.
- Infants who share a room with a parent or caregiver have a lower risk of SIDS.
- Breastfeeding provides a protective effect for SIDS. (Public Health Agency of Canada, n.d.)
LICENSING REQUIREMENTS – O. Reg. 137/15: GENERAL
33.1 (1) Every licensee shall ensure that a child who is younger than 12 months who receives child care at a child care centre it operates or at a premises where it oversees the provision of home child care is placed for sleep in a manner consistent with the recommendations set out in the document entitled “Joint Statement on Safe Sleep: Preventing Sudden Infant Deaths in Canada”, published by the Public Health Agency of Canada, as amended from time to time, unless the child’s physician recommends otherwise in writing. O. Reg. 126/16, s. 23. (O. Reg. 137/15: GENERAL)
Cribs, Sleep Surface, and Bedding
In Canada, all new and used cribs, cradles, and bassinets, either sold, borrowed, or given away for free, must meet the current requirements of the Cribs, Cradles and Bassinet Regulations made under the Canada Consumer Product Safety Act.
Cribs manufactured before 1986 do not meet current standards for spacing between slats and should not be used. In addition, it has been illegal since 2016 to sell, import or manufacture drop-side cribs in Canada.
The mattress should be firm, fit tightly, and be covered with a tight fitted sheet. Babies should not sleep on adult beds, waterbeds, couches, beanbag chairs or other soft surfaces. Do not use fluffy blankets or comforters under the baby, or put the baby to sleep on a sheepskin, pillow, or other soft materials. Keep stuffed toys, bumper pads, loose bedding and other toys and soft objects out of the crib.
Temperature
Babies should be kept warm, not hot. Babies should be dressed in only one additional layer than you are wearing for warmth. In areas where babies sleep, keep the temperature so that it feels comfortable to you. If needed, infants can be dressed in blanket sleepers for warmth. This ensures that the baby’s head will be uncovered during sleep.
Smoke Free
In Ontario, the Smoke-Free Ontario Act (2006) prohibits smoking in all enclosed public spaces and workplaces. Smoke in the infants’ environment is a major risk factor for SIDS.
Pacifiers
If the family provides a pacifier, it should be offered to the infant. If a pacifier is used, it should never be attached to a string. Infants should not be forced to take a pacifier and if it falls out during sleep it doesn’t need to be given back to the infant.
Breastfeeding
Breastfeeding has many health benefits for mother and baby, including a reduced risk of SIDS. Childcare programs should be breastfeeding friendly.
Other Things Educators Can Do to Reduce the Risks Associated with SIDS
- Families should be asked about their infant’s usual sleep position. Educators should discuss the recommended back sleeping position with families and share the program’s policy is to place infants on their back to sleep.
- Policies should be developed to address sleep position. If a family insists their baby sleep on the side or stomach, they should be referred to their health care provider for further information. Programs should request that medical care professional provide a signed statement for infants who have a medical reason for not being placed to sleep on their backs.
- Programs should be aware of resources for additional support and make them available to families as appropriate. It is vital to stay up to date with the latest recommendation for safe infant sleep.
Indoor Falls
While most falls occur outdoors, and this topic is addressed in Module 7.3, they can also happen indoors. Educators (and adults at home) can prevent falls indoors by:
- Installing stops on windows that prevent them from being opened more than four inches or install window guards on lower parts of windows. Removing furniture from near windows. Screens should not be relied on to prevent a fall.
- Installing safety gates at the top and bottom of staircases. Installing lower rails on stairs that children can reach and use. Making sure the surface of the stairs stays clear.
- Using safety straps and harnesses on baby equipment and furniture. Children should not be left unattended in highchairs or on changing tables.
- Baby walkers are banned in Canada, under the Canada Consumer Product Safety Act.
- Teaching children to walk where surfaces may be slick. Preventing these surfaces as much as possible, such as wiping up spills.
Indoor Water Safety
Small children are top-heavy; they tend to fall forward and headfirst when they lose their balance. They do not have enough muscle development in their upper body to pull themselves up out of a bucket, toilet, or bathtub, or for that matter, any body of water. Even a bucket containing only a few inches of water can be dangerous for a small child.
It’s important that educators follow the safety practices discussed in Module 7.4 for water safety both indoors and outdoors, keep children under active supervision, and be very aware of containers of water.
Pause to Reflect 💭
What are your top five tips for protecting children from safety hazards indoors?
These can relate to toy safety, safe art materials, preventing poisoning, preventing choking, prevent burns, safe sleep, protecting from indoor falls, water safety, or any other hazard/are of safety.
Important Things to Remember
- A well-organized learning environment that is interesting, orderly, and attractive contributes to children’s participation and engagement with the learning materials and experiences. This engagement, in turn, contributes to children’s learning.
- Young children communicate their wants and needs through their behavior long before they have or can use words in the heat of the moment.
- Since children are smaller than adults, children’s exposures to the same amount of a chemical may result in more severe effects. Further, children’s developing bodies, including their brains, nervous systems, and lungs may make them more susceptible than adults. Differences in metabolism may also affect children’s responses to some chemicals.
- Although it is not known exactly what causes SIDS, researchers know that it is not caused by suffocation, choking, spitting up, vomiting, or immunizations.
Resources for Further Exploration
Safe Sleep (Government of Canada)
Children’s Product and Toy Safety Regulations in Canada: An Overview (ComplianceGate)
References
- Baby’s Breath Canada (2016). What Every SIDS Parent Should Know. https://www.babysbreathcanada.ca/what-is-sids-sudc-stillbirth/what-every-sids-parent-should-know/#:~:text=SIDS%20is%20rare%20before%20one,SIDS%20every%20week%20in%20Canada.
- Cyr, C. (2020). Preventing Choking and Suffocation in Children. https://cps.ca/en/documents/position/preventing-choking-suffocation-children
- Government of Canada (2012). Information for Art Class Teachers: Chemical Safety. https://www.canada.ca/en/health-canada/services/consumer-product-safety/reports-publications/industry-professionals/art-class-teachers.html
- Government of Canada (2021). Industry Guide to Health Canada’s Safety Requirements for Children’s Toys and Related Products. https://www.canada.ca/en/health-canada/services/consumer-product-safety/reports-publications/industry-professionals/industry-guide-safety-requirements-children-toys-related-products-summary/guidance-document.html#a31
- Moon, R. Y., Patel, K. M., & Shaefer, S. J. (2000). Sudden infant death syndrome in child care settings. Pediatrics, 106(2 Pt 1), 295–300. https://doi.org/10.1542/peds.106.2.295
- O. Reg. 137/15: GENERAL. https://www.ontario.ca/laws/regulation/150137#BK83
- Public Health Agency of Canada (n.d.). Joint Statement on Safe Sleep: Preventing Sudden Infant Deaths in Canada. https://www.phac-aspc.gc.ca/hp-ps/dca-dea/stages-etapes/childhood-enfance_0-2/sids/pdf/jsss-ecss2011-eng.pdf

