7.2.3 – Treating Psychological and Behavioural Symptoms
As Alzheimer’s disease progresses, several psychological and behavioural symptoms begin to emerge. These symptoms put strain on caregivers and medical professionals, often leading to patients being institutionalized. These symptoms are typically grouped into four distinct categories – psychosis, affective symptoms, hyperactivity, and apathy. Though acetylcholinesterase inhibitors and NMDA receptor antagonists have been shown to have mild effects on these behavioural and psychological symptoms, their effectiveness declines as the disease progresses. Thus, combination therapy with various other medications must be considered in order to treat the wide scope of symptoms.
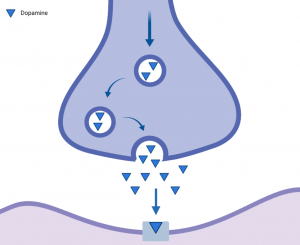
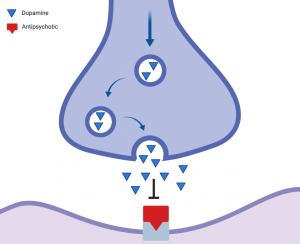
Psychosis encompasses delusions or hallucinations an individual may experience. Atypical antipsychotics such as olanzapine or aripiprazole are commonly prescribed to treat psychosis and aggression in Alzheimer’s patients, as they reduce the amount of Parkinson’s-like side effects such as tremors and body stiffness. Though the direct mechanisms are not known, they are thought to target the dopamine receptors of the brain. Excessive dopamine is thought to be the cause of the various symptoms of psychosis, and blocking its receptor reduces the appearance of symptoms. Though these antipsychotic drugs are effective in treating their symptoms, they have been shown to exert very devastating side effects such as cognitive decline, stroke, and even death.
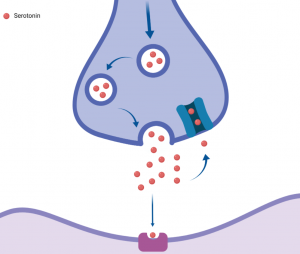
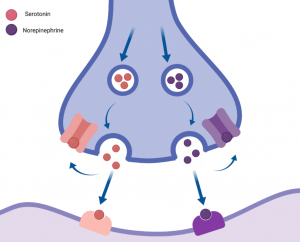
Affective symptoms include common mental health disorders such as anxiety and depression. Depression is a very common comorbidity in Alzheimer’s disease, and is usually treated with selective serotonin reuptake inhibitors or selective norepinephrine and serotonin reuptake inhibitors. Selective serotonin reuptake inhibitors include drugs such as fluoxetine, citalopram, and sertraline, which are known for their efficient treatment of the disorder in Alzheimer’s patients. They are also used in treating hyperactivity presenting as aggression or disinhibition, psychosis, and agitation. These drugs work by blocking the serotonin channels present in presynaptic cells. This is effective in increasing the concentration of free serotonin in the synapse, which contributes to the patient’s mood.
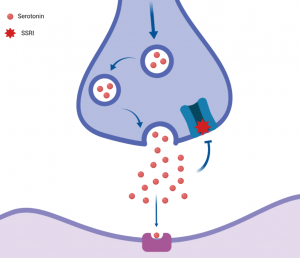
Selective norepinephrine and serotonin reuptake inhibitors include drugs such as venlafaxine and mirtazapine. They work in a similar way as selective serotonin reuptake inhibitors, while also using the same mechanism of action to block norepinephrine from binding to its receptors.
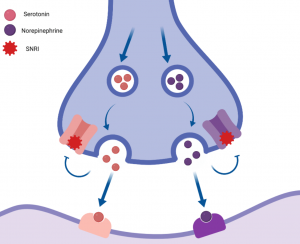
Though both classes of drugs are commonly prescribed for depression, recent studies have shown that Alzheimer’s patients may not experience any benefit whatsoever with these drugs, and are actually at an increased risk of negative side effects.
Benzodiazepines are a common class of drugs used to treat anxiety. These drugs target the GABA gated chloride ion channels. Their binding opens the channel and leads to cell hyperpolarization, resulting in an overall reduced ability of neurons to receive more action potentials. Some studies have linked the use of these drugs to faster cognitive and functional decline as well as increased levels of agitation, indicating that they may not always be effective in Alzheimer’s patients.
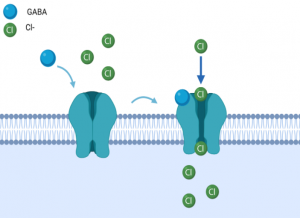
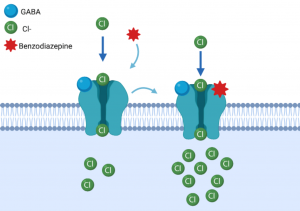
Figure 6: A. GABA gated chloride ion channels open to depolarize the cell after the GABA molecule binds. B. Benzodiazepines bind to the GABA gated chloride ion channels to attenuate the ion influx and hyperpolarize the cell, preventing it from responding to a new action potential. (adapted from https://mainequalitycounts.org/wp-content/uploads/2018/02/Benzo-and-Opioids_PowerPoint-Slide-Deck_3.14.17.pdf)
