14 1.3 Vitexin: A Promising Anti-Tumour Treatment?
Symptomology: Good or Bad?
Cytotoxicity
Cytotoxic drugs are characterized as having a low therapeutic index due to three factors.
- Therapeutic concentrations cannot be achieved at the site of the tumour
- Cytotoxic effects on normal non-specific tissues
- Formulation of the drug may exhibit problems.
There can be either high cytotoxic or low cytotoxic treatments. In the case of vitexin, the cytotoxicity is low.[1]
There has been debates about whether or not toxicity is a key factor in clinical outcomes of cancer treatments and if it predicts favorable outcomes.[2] Toxicity can involve clinical outcomes such as a rash, gastrointestinal toxicity, and myelosuppresion.[3] Toxicity have been found to have good implications. For example, patients exhibiting neutropenia and non-small lung cancer have increased survival rates with certain toxic therapies.[4] However, toxicity has also have been with negative implications. Treatment can lead to myelosuppression, which disadvantages the clinical outcomes of patients.[5][6] Another example of cytotoxicity-associated outcomes can be seen in the case of peripheral neuropathy. The presence of peripheral neuropathy can lead to improved results for those with ovarian cancer, but not for patients with breast cancer. In a study done by Abola, Prasad, & Jena (2014), results indicated that greater toxicity treatments induced greater clinical efficacy. The effect was dependent on the type of toxicity. Although achieving high efficacy is favourable, the unfortunate aspect of high cytotoxic treatments are the greater injury that may cause more suffering to patients.[7] Therefore, finding a low toxicity treatment with high efficacy is important, so that patients can undergo less symptomatic-effects, whilst achieving tumour-growth inhibition.
Vitexin: A Low Cytotoxic Treatment
Vitexin is known to present low cytotoxic effects, with beneficial pharmacological effects such as anti-oxidant, anti-cancer, anti-inflammatory, and neuroprotective outcomes.[8] After repeated treatment of vitexin during a 7-day period on liver and gastric injuries, no adverse symptoms were present.[9] In another study looking at the inhibition of neutrophil migration induced by vitexin, researchers found that vitexin caused the inhibition of pro-inflammatory mediators, resulting in no damaging consequences.[10] This signifies that vitexin is a safe treatment, with similar anti-proliferation effects as high cytotoxic treatments.
Though vitexin has low cytotoxicity, research is still required for understanding it’s full pharmacokinetic effects.[11] So far, what is understood is that intravenous and oral administration of vitexin causes wide and rapid distribution of the drug across different tissues.[12] Oral administration of vitexin causes poor absorption by the gastrointestinal tract, allowing it to directly reach the colon.[13][14] Vitexin treatment given intravenously, resulted in most of the drug appearing in the liver and kidney. It was least likely to be seen in fatty areas and in the brain of rats.[15] For cancer treatment, oral administration may not be an effective method if it has a low bioavailability. However, when injected, there is a more body-wide distribution of vitexin. In conjunction with the in vivo results of Liu et al’s (2019) study, testing various methods of administering vitexin may help determine the most effective treatment procedure.
Vitexin and Other Cancer Cells
This study is consistent with most studies, as vitexin has been seen to induce apoptosis in other carcinoma cells:
| Hepatocellular carcinoma | Located within the liver. Vitexin was seen to induce apoptosis through the down-regulation of Bcl-2, which as mentioned before is an anti-apoptotic protein and induces the cleavage of caspase 3.[16] Research also shows a suppression of autophagy and the activation of the JNK-MAPK signalling pathway. |
| U397 human leukemia cells | Vitexin had induced similar results, resulting in the same changes to Bcl-2/Bax ratio and caspase expression seen in the paper by Liu et al. (2019).[17] |
| EC-109 esophageal cancer cells | Treatment with vitexin resulted in the down-regulation of Bcl-2 and the up-regulation of p53, leading to apoptosis.[18] |
| HCT-116 colorectal cancer cells | When treated with vitexin, these cells exhibited up-regulation of p53, Bax, and PUMA. Experiments have been done both in vivo and in vitro, each showing suppression of tumour formation.[19] |
Current Cancer Treatments
There are many potential treatments being researched to determine which pathways can be targeted to prevent cancer cell proliferation:
mTOR
mTOR is seen as an attractive target for many anti-cancer treatment. In previous studies, mTOR has been targeted by using anti-fungal agents such as rapamycin (branded Sirolimus). Rapamycin was originally used to treat cancers, but was later deemed unfavourable due to its negative effects on the human body. However, rapamycin has been developed into different agents, including temsirolimus, everlimus, and ridaforolimus. Each agent functions intracellularly by attaching to the FK506 binding protein. This forms a complex, which is recognized by mTOR, leading to the inhibition of cellular survival and cell cycle progression. The differences of these agents lead to various pharmacokinetic profiles that are dependent on the location of the cancer cells. For example, neuroendocrine tumors, breast cancers, and so forth, each have different optimal drugs needed for treatment.[21]
Bcl-2
Venetoclax is a chemotherapeutic drug that is currently used as a Bcl-2 inhibitor. This drug has been used as a treatment method for other cancers, such as chronic lymphocytic leukemia and small lymphocytic lymphoma. Although side effects include nausea, the reduction of white blood cells, diarrhea, and tumour lysis syndrome. Tumour lysis syndrome can lead to kidney failure as a result of the release of uric acid, potassium, and phosphorous due to rapid death of several cancer cells.[22][23]
Other Flavonoids and Their Effects
Alongside vitexin, other natural compounds have also explored for their known benefits (Liu et al, 2019). High fruit and vegetable diets are associated with lower risk of common cancers such as breast, prostate, and colon cancers.[24] The bioactive compounds leading to chemoprotective effects within these plants are unknown. Flavonoids are being researched as potential cancer prevention compounds.[25]
The following are some examples of flavonoids under investigation as potential anti-tumour treatments:
Tubeimoside-1: similar to vitexin, TBMS1 has also been used as a traditional Chinese herbal medicine.
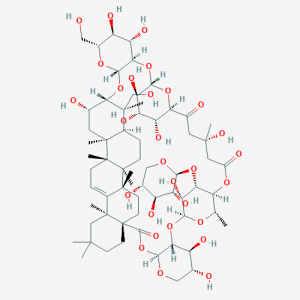
Jia et al (2015) looked at the efficacy of TBSMI as a potential cancer treatment against glioma tumour cells. Glioma are a form of inter-cranial tumours, accounting for close to majority of brain-spinal cancers, they also have a very low cure rate and high mortality rate. In this study, the effects of TBMS1 inhibited the glioma tumour proliferation in a time and dose-dependant manner, much like Liu et al’s (2019) study in regards to vitexin. Similarly effecting the same pathways: upregulating bax, while reducing expression in bcl-2, leading to the release of cytochrome c and cleavage of caspase-3 resulting in apoptosis. [26]

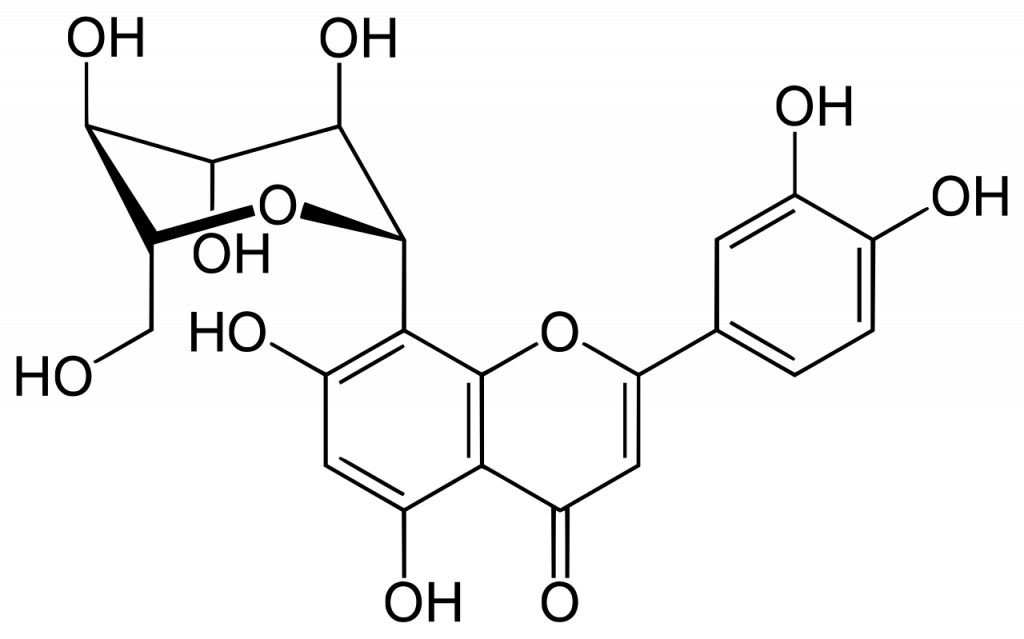
Orientin: a flavonoid monomer in the plant Trollius chinensis bunge, alongside vitexin. Orientin contains a similar chemical makeup to vitexin and has anti-thrombus and antioxidant properties. This flavonoid has been tested as a potential anti-tumor therapy treatment against esophageal cancer cells in a study done by Fang et al (2015), indicated that orientin had exhibited stronger anti-tumour effects compared to vitexin using the same concentration.[27]

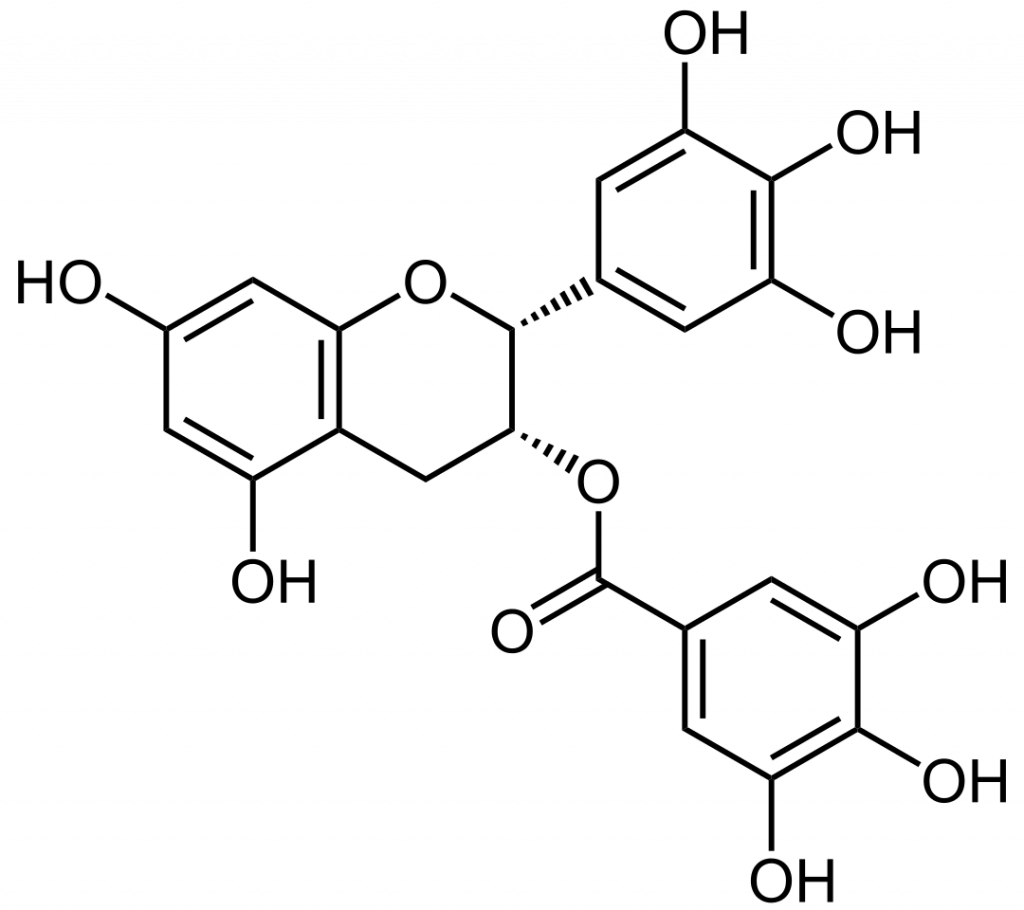
EGCG: epigallocatechin-3-gallate is a flavonoid found in green tea, and has been heavily researched for its ability to induce apoptosis and inhibit cancer cell proliferation for carcinomas such as HeLa cervical cells, laryngeal squamous carcinoma cells, melanoma cells, and A549 cells. However, the downstream mechanisms inducing apoptosis varies between cell lines; therefore, apoptosis can be completed through mitochondrial-dependent pathways, endoplasmic-dependent pathways, or extrinsic pathways (through cell-death receptor).[28]
- Cytotoxic Agent. Cytotoxic Agent - an overview | ScienceDirect Topics. [accessed 2019 Dec 5]. https://www.sciencedirect.com/topics/medicine-and-dentistry/cytotoxic-agent ↵
- Abola MV, Prasad V, Jena AB. Association between treatment toxicity and outcomes in oncology clinical trials. Annals of Oncology. 2014;25(11):2284–2289. ↵
- Abola MV, Prasad V, Jena AB. Association between treatment toxicity and outcomes in oncology clinical trials. Annals of Oncology. 2014;25(11):2284–2289. ↵
- Maio MD, Gridelli C, Gallo C, Shepherd F, Piantedosi FV, Cigolari S, Manzione L, Illiano A, Barbera S, Robbiati SF, et al. Chemotherapy-induced neutropenia and treatment efficacy in advanced non-small-cell lung cancer: a pooled analysis of three randomized trials. The Lancet Oncology. 2005;6(9):669–677. ↵
- Abola MV, Prasad V, Jena AB. Association between treatment toxicity and outcomes in oncology clinical trials. Annals of Oncology. 2014;25(11):2284–2289. ↵
- Koutras AK, Kalofonos HP. Myelotoxicity in Cancer Patients Treated with Chemotherapy: Negative or Positive Prognostic Factor? Clinical Cancer Research. 2008;14(22):7579–7579. ↵
- Abola MV, Prasad V, Jena AB. Association between treatment toxicity and outcomes in oncology clinical trials. Annals of Oncology. 2014;25(11):2284–2289. ↵
- He M, Min J-W, Kong W-L, He X-H, Li J-X, Peng B-W. A review on the pharmacological effects of vitexin and isovitexin. Fitoterapia. 2016;115:74–85. ↵
- Borghi SM, Carvalho TT, Staurengo-Ferrari L, Hohmann MSN, Pinge-Filho P, Casagrande R, Verri WA. Vitexin Inhibits Inflammatory Pain in Mice by Targeting TRPV1, Oxidative Stress, and Cytokines. Journal of Natural Products. 2013;76(6):1141–1149. ↵
- Rosa SIG, Rios-Santos F, Balogun SO, Martins DTDO. Vitexin reduces neutrophil migration to inflammatory focus by down-regulating pro-inflammatory mediators via inhibition of p38, ERK1/2 and JNK pathway. Phytomedicine. 2016;23(1):9–17. ↵
- Maio MD, Gridelli C, Gallo C, Shepherd F, Piantedosi FV, Cigolari S, Manzione L, Illiano A, Barbera S, Robbiati SF, et al. Chemotherapy-induced neutropenia and treatment efficacy in advanced non-small-cell lung cancer: a pooled analysis of three randomised trials. The Lancet Oncology. 2005;6(9):669–677. ↵
- Yin J, Qu J, Zhang W, Lu D, Gao Y, Ying X, Kang T. Tissue distribution comparison between healthy and fatty liver rats after oral administration of hawthorn leaf extract. Biomedical Chromatography. 2013;28(5):637–647. ↵
- Zhang Y, Tie X, Bao B, Wu X, Zhang Y. Metabolism of flavone C-glucosides and p-coumaric acid from antioxidant of bamboo leaves (AOB) in rats. British Journal of Nutrition. 2007;97(3):484–494. ↵
- Yin J, Qu J, Zhang W, Lu D, Gao Y, Ying X, Kang T. Tissue distribution comparison between healthy and fatty liver rats after oral administration of hawthorn leaf extract. Biomedical Chromatography. 2013;28(5):637–647. ↵
- He M, Min J-W, Kong W-L, He X-H, Li J-X, Peng B-W. A review on the pharmacological effects of vitexin and isovitexin. Fitoterapia. 2016;115:74–85. ↵
- Wang Z, Li S-P, Xu Y-J, Yu Y, Ding Y-J, Yu W-L, Zhang R-X, Zhang H-M, Du H-Y. Vitexin suppresses autophagy to induce apoptosis in hepatocellular carcinoma via activation of the JNK signaling pathway. Oncotarget. 2016;7(51). ↵
- Lee C-Y, Chien Y-S, Chiu T-H, Huang W-W, Lu C-C, Chiang J-H, Yang J-S. Apoptosis triggered by vitexin in U937 human leukemia cells via a mitochondrial signaling pathway. Oncology Reports. 2012;28(5):1883–1888. ↵
- An F, Wang S, Tian Q, Zhu D. Effects of orientin and vitexin from Trollius chinensis on the growth and apoptosis of esophageal cancer EC-109 cells. Oncology Letters. 2015;10(4):2627–2633 ↵
- Chen J, Zhong J, Liu Y, Huang Y, Luo F, Zhou Y, Pan X, Cao S, Zhang L, Zhang Y, et al. Purified vitexin compound 1, a new neolignan isolated compound, promotes PUMA-dependent apoptosis in colorectal cancer. Cancer Medicine. 2018;7(12):6158–6169. ↵
- Arterial Circulation - Servier Medical Art https://smart.servier.com/smart_image/artery-40/ ↵
- Porta C, Paglino C, Mosca A. Targeting PI3K/Akt/mTOR Signaling in Cancer. Frontiers in Oncology. 2014 [accessed 2019 Dec 6];4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3995050/. doi:10.3389/fonc.2014.00064 ↵
- Kalkavan H, Green DR. MOMP, cell suicide as a BCL-2 family business. Cell Death & Differentiation. 2018;25(1):46–55. doi:10.1038/cdd.2017.179 ↵
- Venetoclax (Venclexta) Chemotherapy Drug Information. [accessed 2019 Dec 6]. http://chemocare.com/chemotherapy/drug-info/venetoclax.aspx ↵
- Neuhouser ML. Review: Dietary Flavonoids and Cancer Risk: Evidence From Human Population Studies. Nutrition and Cancer. 2004;50(1):1–7. ↵
- Neuhouser ML. Review: Dietary Flavonoids and Cancer Risk: Evidence From Human Population Studies. Nutrition and Cancer. 2004;50(1):1–7. ↵
- Jia, G. et al. Tubeimoside-i induces glioma apoptosis through regulation of Bax/Bcl-2 and the ROS/Cytochrome C/caspase-3 pathway. Onco. Targets. Ther. 8, 303–311 (2015). ↵
- An F, Wang S, Tian Q, Zhu D. Effects of orientin and vitexin from Trollius chinensis on the growth and apoptosis of esophageal cancer EC-109 cells. Oncology Letters. 2015;10(4):2627–2633. ↵
- Gibellini L, Pinti M, Nasi M, Montagna JP, De Biasi S, Roat E, Bertoncelli L, Cooper EL, Cossarizza A. Quercetin and cancer chemoprevention. Evid Based Complement Alternat Med. 2011;2011:591356. ↵
