28 2.1: Background of Alzheimer’s Disease
What is Alzheimer’s Disease?
Alzheimer’s Disease (AD) is a progressive neurological disorder that affects nearly 50 million people worldwide (Alzheimer’s Statistics). It is the most common type of dementia which affects memory, thinking and behaviour. This disease usually occurs in older people over the age of 65, however, approximately 10% of cases of Alzheimer’s disease are early-onset which involves people ages under 65 (Wattmo and Wallin). Some signs for Alzheimer’s disease include memory loss, difficulty in completing familiar tasks, changes in mood and personality, confusion with time and place and others (Holtzman et al.). This disease was first discovered by Dr. Alois Alzheimer in 1907 when he noticed that a woman died of an unusual symptom of mental illness (Bondi et al.). He then examined her brain where he found abnormal pathological findings in her brain including amyloid plaques and tangled fibers. Until now, his early findings are still the main pathological hallmarks of Alzheimer’s disease.
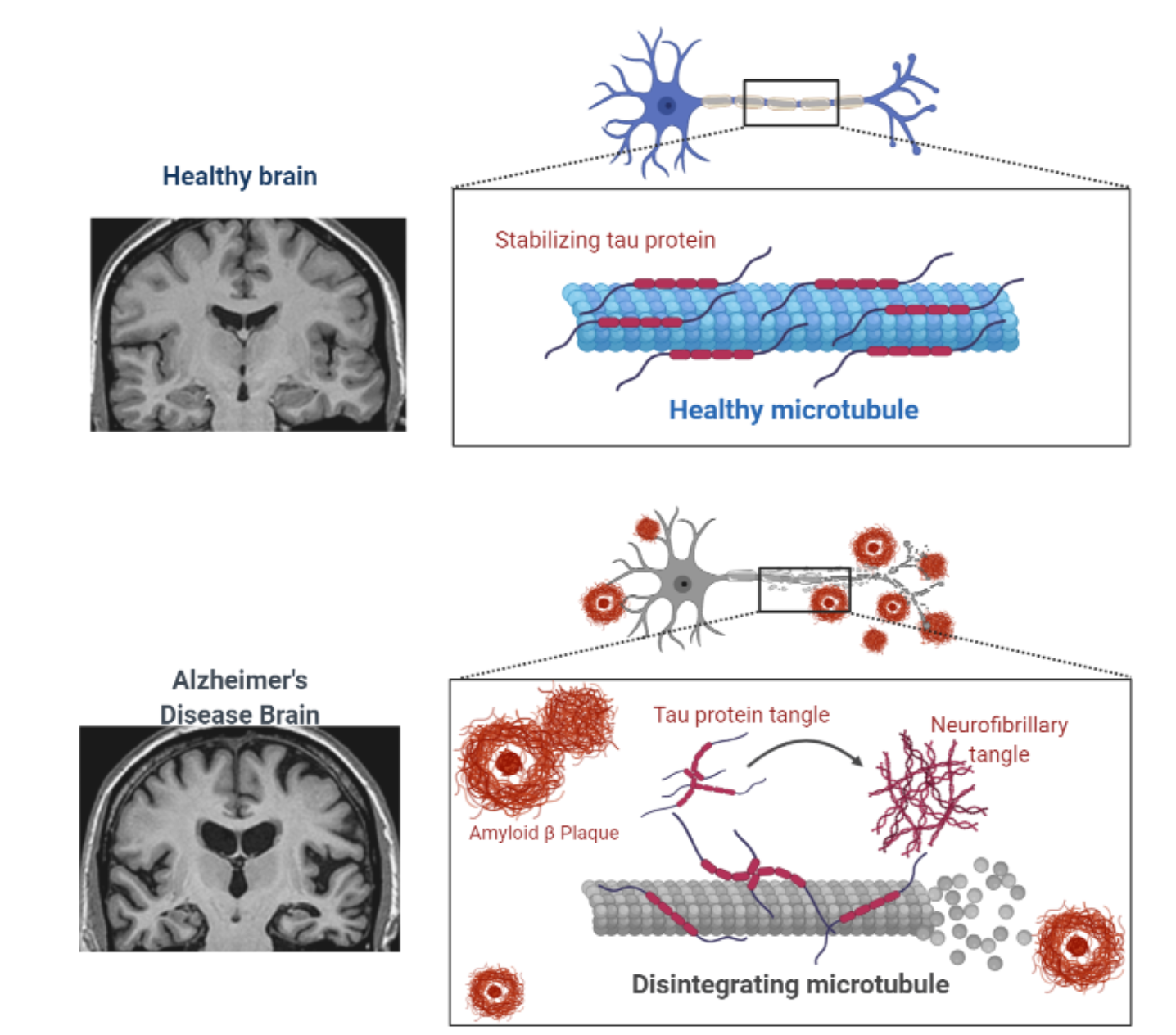
This irreversible degenerative brain disease is characterized by 2 major pathological hallmarks: 1) Accumulation of amyloid-β plaques 2) Hyperphosphorylation of Tau protein causing neurofibrillary tangles (Yin et al.). The normal function of amyloid-β is still not well understood but it has been shown that it is associated with neurogenesis and synaptic plasticity (Rajasekhar et al.). In a healthy brain, the function of tau protein is to bind and stabilize microtubules in neuronal axons (Zetterberg). In Alzheimer’s disease, these 2 hallmark pathologies both lead to extensive neuronal loss which begins early before the onset of this disease. When plaques and tangles are spread across the brain, not only does it promote loss of neurons, it also promotes loss of synaptic activity via inflammation and oxidative stress (Wang et al.).
What is happening in the brain of people with Alzheimer’s Disease?

There are billions of neurons in our brain that send and receive information throughout our body and allows us to do our day-to-day activities. In Alzheimer’s disease patients, there is a loss of neuronal function which then disrupts signal communication in our body limiting us to our activities. Brain changes in Alzheimer’s disease patients could begin as early 10 to 20 years prior to the first onset (Holtzman et al.). It has been strongly proven that there is altered neurogenesis in the hippocampus of the brain of Alzheimer’s disease patients (Mu and Gage). This is critical as the hippocampus is the section of the brain that is related to learning and memory. If this section of the brain is affected, then it heavily affects long-term potentiation (LTP) of synaptic transmission that is correlated to learning and memory (Penn et al.). Not only that hippocampus is affected, the cerebral cortex that is responsible for speech and decision-making is also affected (Fjell et al.). Throughout time, as there are more neuronal loss, more parts of the brain begin to shrink and are affected (Tabatabaei‐Jafari et al.).
Alzheimer’s Disease detection
Neuroimaging is the technique that is very functional and is mostly used to identify people with suspected Alzheimer’s disease. These technologies include magnetic resonance imaging (MRI), computerized tomography (CT) and positron emission tomography (PET).
One of the biomarkers that are used to detect Alzheimer’s disease is the cerebrospinal fluid (CSF). Since CSF is in direct contact with the brain, it allows us to detect the level of amyloid-β and use PET imaging to identify the deposition in the brain (Counts et al.). Another pathology of Alzheimer’s that can be used from CSF biomarkers is the phosphorylated tau proteins that are released from neurofibrillary tangles. PET imaging can also visualize tau inclusions in vivo in patients (Lashley et al.).
Early detection of Alzheimer’s disease is very crucial as it could help individuals to access more early treatment options. Also, it allows people to prepare emotionally and socially for future planning especially on resources and support programs.
Treatment of Alzheimer’s Disease
So far, there is still no cure for Alzheimer’s disease but there have been many potential treatments to slow down its progression. Alzheimer’s disease is a multifactorial disease, meaning that there has been strong evidence showing some risk factors such as age, genetics, diet, vascular health, gut microbiome and others to this disease. As for now, drug treatments that are commonly used for patients with Alzheimer’s disease are cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine. These drugs are helpful as it helps symptoms of the disease specifically in cognition function. The mechanism behind cholinesterase inhibitors drugs is due to the enhancement of cholinergic transmission by inhibiting acetylcholinesterase (AChE) as there is impairment in the cholinergic function in Alzheimer’s disease patients (Anand and Singh). By blocking AChE, it allows potentiation of cholinergic transmission.
Quick Fact!
Based on Alzheimer’s Society Canada, in 2016, there was an estimated cost of $10.4 billion per year relating to Alzheimer’s disease. It is expected to increase by 60%, up to $16.6 billion by 2031.
